Introduction
Maxillofacial trauma can occur with high frequency while playing sports, resulting in bone fractures and soft tissue lacerations, abrasions and contusions.1 Publications focusing on maxillofacial injuries treated at emergency departments attribute 4% to 41% of all facial fractures to sports accidents.2 These injuries result most commonly from direct contact between players (head-to-head collisions, facial contact with upper extremities such as shoulders of elbows and kicks to the head or face), direct hit with equipment (including ball, disc or projectiles) and falls.2-4
Epidemiological studies show that the relative incidence of facial injuries directly correlates to the popularity of each sport in a particular region, and its inherent form of play, rules and (lack of) protective equipment. Football, the most popular sport in the world, has the highest frequency of facial fractures in Italy (41.6% and 43.5%),5,6 France (25%),7 Germany (59%),8 and Finland (29%).9 Interestingly, different sports have the second highest frequency, depending on the country: cycling in Italy, rugby in France, handball in Germany and ice-hockey in Finland, reflecting regional sports popularity differences. In Switzerland and Austria, countries with mountain ranges, including the Alps, winter sports are particularly prevalent. Therefore, in both countries, skiing/snowboarding and skiing alone are the most common causes of sports-related facial fractures (27% and 31.1%, respectively).4,10 In Japan, baseball is consistently considered the most popular sport. Again, a correlation between sport popularity and sports-related facial fractures is found, as baseball accounts for 44% of all facial fractures related to sports with balls.11 Another important factor affecting incidence of facial injuries is gender. Male to female ratio has been reported to range from 3:2 in tennis12 and up to 19:1 in collective ball games.11) It has been suggested that gender differences may be explained by higher exposure of males to sports, physical factors such as bulkier muscle mass and, consequently, greater forces of impact, and behavioral factors linked to increased thrill-seeking and willingness to take risks.13 Regardless, due to unavailable data, most studies do not take into consideration sport participation rates and the injury per hours-of-exposure ratio. As shown in a study conducted in Switzerland, following standardization for total exposure during 32 sports categories in both males and females, the apparent higher rate in males was reversed and female sports presented an increased overall risk.14 Age also affects the incidence of facial injuries in sports, with some studies placing individuals ranging from 20- to 30-year-old at higher risk.8,15,16 A Japanese study analyzing facial injuries in ball games found that patients belonging to the 10- to 19-year age-group were more prone to injury, as the authors would expect, considering the age distribution of the sports population and interest of the Japanese in sports from young age.11 A North American study focusing on football (locally soccer) correlated age with injury type and found that patients over 18 had higher risk of laceration and fracture, while those with 18 and under had a higher risk of contusion.1 Facial injury incidence throughout the year also seems to fluctuate and can be correlated with certain months. Studies conducted in Germany and New Zealand found that the incidence of fractures was higher in Spring and Summer,8,17 while, in contrast, a Swiss study found a peak of injuries in winter, precisely the period when skiing, snowboarding and ice hockey are popular in the country.10
Sports-related facial fractures most frequently affect the nose, zygoma and mandible, regardless of the country and sport.3 Nevertheless, specific patterns of fracture can be predicted for different sports. One study from Australia compared facial fractures occurring in all four types of football played in the country: Australian rules, rugby union, rugby league and soccer.18 Mandibular and midface fractures were more common in high collision football (league and union) and low contact football (Australian rules and soccer), respectively. The authors hypothesized that different force vectors were involved in each fracture type: low-to-high, as in a shoulder against the face, would result in mandibular injury, while horizontal impacts of the head or elbow against the face would cause midface injury. Another study from the Netherlands corroborates these findings, as mandible angle fractures were relatively more frequent in rugby, while coronoid process fractures (secondary to zygomatic arch fractures) were only observed in football.16
Prevention of facial injuries seems to be achievable through two different mechanisms: the introduction of protective facial gear and/or rules change. An Irish study focusing on the etiology of sport-related fractures during a period of over three decades described how hurling, a game played with a wood stick and ball, was responsible for 56% of all facial injuries in 1979, while in 2010, it was associated with only 2.5% of injuries.19 The dramatic decrease in incidence was a direct result of the introduction of helmets with faceguards in 1990 and the establishment of a new rule in 2010, making the use of this gear compulsory. Regarding football, a sport with no head and face protection, a new rule was introduced in 2006, punishing direct and deliberate facial hits with the elbow with a red card (player sent off). In a study focusing on the effects of this rule introduction in the 1st German Male Bundesliga, the authors noted a reduction of 29% in head injuries, 42% in lacerations/abrasions, 18% in contusions and 16% in facial fractures, highlighting how the new rule appeared to reduce the risk of head and facial injury.20
Anatomically speaking, facial injuries related to sports may not be very different from those resulting from interpersonal violence or falls. Because of this most surgeons have been treating all these injuries over the years in the same fashion regardless of etiology.21 A new line of thought among maxillofacial surgeons, also shared by the authors, believes athletes could benefit from a more personalized approach to treatment, aimed at optimizing the timeframe for the return to play. In this review we intend to characterize some of the most common sports-related facial injuries and analyze current literature on the topic of return to play following facial trauma.
Initial evaluation of facial trauma
Facial injuries occur frequently while playing sports.3 Team physicians and health care providers for athletes should understand the most common facial injuries, the anatomy of the face, and associated management of facial trauma.3 Initial evaluation is important to distinguish between stable injuries that can be treated on the sidelines or after match and emergencies requiring prompt hospital transfer.
In a trauma setting, regardless of injury location, evaluation begins with the “ABCDE” (airway, breathing, circulation, disability and exposure) protocol. The primary goals include securing a stable airway, supporting ventilation, evaluating circulation, identifying, and controlling life threatening hemorrhage, obtaining a baseline neurologic evaluation, and exposing the patient to evaluation for injuries.22 The resulting hemorrhage and deformity from facial trauma can distract providers from recognizing critical injuries that need immediate intervention. Life-threatening injuries, including intracranial, spinal, and visceral injuries, require urgent attention.22 Therefore, it is important to stay focused on the algorithm of evaluation.23
Failure to recognize airway compromise and appropriately secure and protect the airway is the most common factor related to patient mortality in facial trauma.23 Maxillofacial trauma can contribute to airway obstruction from bleeding, posterior mobility of the maxilla to the nasopharynx, prolapse of the tongue to the posterior oropharynx in mandibular fractures, displaced dentition and other foreign bodies, soft tissue swelling, and trismus from underlying muscle spasm or fracture.23,24
After the initial assessment and stabilization, the provider can proceed to a more focused facial examination.
Head and cervical spine injuries
When approaching an athlete who suffered facial trauma, we should suspect and investigate possible head and cervical spine injuries. These lesions are often present with maxillofacial fractures: spine injury in up to 10%25 and head injury in up to 23%.26
Midline cervical spine tenderness, bilateral paresthesia or weakness, and/or alteration in mental status require immediate on-field cervical spine immobilization.25 The patient’s neurologic status must be assessed to identify those at risk for mental status decline and those who may require emergency transfer for further imaging and work-up.26
Sports related concussion is another possible consequence from a direct blow to the head, face and neck. It may also occur with impact with other body parts with impulsive force being transmitted to the head.27 Concussion is defined as rapid onset of short-lived impairment of neurologic function that resolves spontaneously.27 When suspected the athlete should be held from activity, followed by further evaluation, appropriate rest until symptom resolution, and gradual return to activity.3
Maxillofacial evaluation
After initial assessment, further neurologic, orbital, facial and neck examination should be performed. Soft tissue injuries, as well as facial bone fractures, occur frequently with facial trauma. Depending on the type of sport, maxillofacial fracture patterns may vary. The diagnosis of maxillofacial fractures is achieved by combining history, including mechanism of injury, physical examination and imaging.
The face can be vertically divided in thirds: upper, middle and lower face. Physical examination of the upper third of the face includes palpation over the supraorbital rims, assessing for tenderness or bony deformities and evaluation of the frontal branch of the facial nerve.3
Examination of the middle third of the face requires palpation of the infraorbital rims, assessing for stability and tenderness, examination of globe position and extraocular muscles movements, which could suggest an orbital wall fracture. Presence of exophthalmos decreased visual acuity, ophthalmoplegia, and fixed dilated pupils or a relative afferent pupillary defect (RAPD) can indicate an orbital compartment syndrome. This is a surgical emergency, characterized by an acute rise in orbital pressure, and should be promptly treated with lateral canthotomy and cantholysis to decompress the optic nerve.
Evidence of zygomatic arch or malar prominence flattening and widening of the midface are signs of zygomaticomaxillary complex fracture. Evaluation of the nose focuses on symmetry, presence of obstruction, epistaxis, and septal hematoma. To complete midface examination, maxillary mobility must be assessed. Presence of midface mobility may be an indication of a Le fort fracture.
In the lower face, initial inspection should look for symmetry, assess opening of mouth, and malocclusion. If any change is noted, it may indicate possible mandible fracture or temporomandibular joint dislocation. Intraoral examination may reveal soft tissue lesions and dental injuries, such as avulsion, luxation, or fracture.
The head and neck region is a highly vascular and well-innervated region of the body. Therefore, most patients with maxillofacial fractures present severe immediate pain and develop significant soft tissue edema over the fractured bones, making clinical examination more difficult.28
Computed tomography (CT) imaging has become the gold standard for the radiographic evaluation of patients with facial trauma. CT angiography is predominantly reserved for the evaluation of arterial injury in the setting of penetrating neck trauma.
Soft tissues injuries
Soft tissue trauma consists of abrasions, contusions, and lacerations. Contusions or bruises are the simplest soft tissue injuries. Minor injuries only require ice application and do not interfere with return to play. More severe contusions may affect underlying skeletal and soft tissue lesions. Soft tissue injuries can involve vascular or nerve trauma, with consequent altered motor or sensitive function. Hematomas of the masseter or temporalis muscles can cause trismus. Hemarthrosis of the temporomandibular joint can occur with jaw contusion and may also be a cause of trismus or malocclusion. Treatment generally comprises of rest and soft diet.29
Abrasions are superficial injuries to the skin, affecting only epidermis. They rarely affect immediate return to play but should be cleansed and dressed at the appropriate time and protected from reinjury.29 Antibiotic ointment can be applied, especially for extensive abrasions.
Facial lacerations involve a tear that goes through the epidermis and/or dermis including possible injuries to deeper tissues. It can be caused by blunt or sharp trauma and vary from a superficial to a through-through laceration involving significant vascular disruption or injury to collateral vital structures.3
All open wounds of the face need to be cleansed and explored to assess severity. Hemostasis is always a prime concern of initial treatment. Arterial bleeding of a facial or neck vessel can be life threatening and prompt application of pressure, and transport to the hospital is sometimes necessary. Other structures can be injured with lacerations including nerves (mostly facial and trigeminal), salivary ducts (parotid or submandibular), and lacrimal apparatus. In addition, there may be concomitant hard tissue injury to underlying bone or dentition.29
The wound is closed with non-absorbable sutures in the skin, and absorbable suture for mucosal lacerations. More complex wounds may require layered sutures to allow better approximation of tissues, eliminate dead space and reduce infection, improve the ultimate scar and function, and allow a better, more tension-free closure.29
Lesions with tissue loss are called avulsions. An avulsion can be repaired with primary closure, grafts, local flaps, regional flaps, or free tissue transfer, depending on the size and location of the defect.3
In tetanus prone wounds, status of tetanus vaccination should be evaluated. If vaccination status is not up to date, patients should receive tetanus immunoglobulin. Antibiotics in the perioperative period should be considered for mucosal wounds, contaminated wounds, bite wounds, delayed closure, and in patients with diabetes, immunocompromised, alcoholism, malnutrition, smoking, or other factors that affect wound healing.30
Frontal sinus fractures
Frontal sinus fractures result from trauma to the forehead and require high force of impact. Periorbital ecchymosis and pain in the forehead along with lacerations could be signs of these fractures.
Management of frontal sinus fractures is based on the structural integrity of three anatomic parameters: anterior table, frontal sinus outflow tract, and the posterior table/dura.31 Options of treatment are conservative treatment and open surgical management. Surgical access to the fractures is based on coronal (bitemporal) incision or through existing lacerations.32
If an isolated anterior wall fracture with depressed segment causes facial deformity, surgical repair may be required to reduce the fragment and fixate it with titanium miniplates or mesh (Fig. 1). If nasofrontal ducts are involved in the fracture, duct and sinus obliteration should be considered. This is achieved by removing any sinus lining and plugging the ducts with autogenous material such as fat, pericranium, temporalis muscle, fascia, or bone.32
When a posterior wall fracture is present, determination of dural tears and cerebrospinal fluid (CSF) leaks is fundamental. All patients should be evaluated by neurosurgery and monitored for CSF rhinorrhea. Fractures with displaced or grossly comminuted posterior wall fractures require a cranialization procedure (removal of entire damaged posterior wall). Long-term follow-up for complex frontal sinus injuries is essential.31
Nasal fractures
Due to their central location in the face and the natural projection, nasal bones are especially susceptible to trauma from sports, vehicle collisions or assault. The nasal fracture is the most common fracture of the facial skeleton and is often associated with septum fracture.32
Most of these fractures are managed with close reduction and this procedure is indicated when there is visible deformity or nasal obstruction due to the injury. One meta-analysis of studies comparing local versus general anesthesia for closed nasal bone reduction found that despite increased cost and risks of general anesthesia, patient satisfaction in esthetic and functional outcomes was higher in those who had received general anesthesia, and they were less likely to need secondary corrective surgery; however, only the improved esthetic outcome was statistically significant.33
Eye and orbital trauma
Orbital trauma is a commonly seen athletic injury and it can be associated with lesions to the eye globe or other structures of the orbit, such as orbital wall fractures.
Prevention is the most effective way to eliminate the significant morbidity and costs associated with sports-related eye injuries.34 Certain sports have a greater propensity for orbital injury and those include baseball/softball, paintball, basketball, racquetball, football, and soccer.35
Trauma to the eye may occur by blunt, penetrating, or perforating mechanisms. Blunt injuries refer to contusions or forces that strike an intact globe. Penetrating injuries occur when there is a single laceration to the eye causing an open globe, and perforating injuries occur when 2 full-thickness lacerations (entrance and exit) are present and are usually caused by a sharp object or missile.34 Timely closure of the open wound is required in the operating room to reduce the risk of infection and permanent loss of vision.
Nonpenetrating eye trauma can result in a wide variety of tissue damage to the cornea, iris, lens, vitreous, choroid, and retina. The expansion of the eyeball perpendicular to the direction of impact has been proposed to be responsible for the injuries that occur from blunt trauma.34
When an orbital bone fracture is suspected, a CT scan of the orbits is the exam of choice to confirm the diagnosis. Fractures of the orbital floor are the most common orbital fracture pattern. Patients with orbital fracture who present with diplopia, enoftalmus and/or very large fractures may have indication for surgical repair.
Approximately, 20% of orbital fractures have some associated ocular pathology.35 Ophthalmology consultation and evaluation for all patients with orbital trauma should be considered.
Orbital roof fractures are less common, but their potential for morbidity is high. Fractures that involve the anterior cranial fossa may lead to pneumocephalus or a dural tear resulting in cerebrospinal fluid leak. Concurrent traumatic brain injury with intracranial hemorrhage can be seen in approximately two thirds of cases.36 Evaluation of orbital roof fractures should involve the facial trauma team, ophthalmology, and neurosurgery.
Zygomaticomaxillary complex (ZMC) and midface fractures
Most retrospective reviews present ZMC fractures as one of the most common sports related fractures of the face.19,28 ZMC forms part of the orbit, provides an attachment point for superior masseter muscle, and forms the lateral facial prominence and frame.3
The signs and symptoms of ZMC fractures include periorbital ecchymosis, subconjunctival hemorrhage, epistaxis, hypoesthesia of the infraorbital nerve territory, midface asymmetry, palpable step-offs of the orbital rim, depression of malar prominence or zygomatic arch, orbital subcutaneous emphysema, malposition of the globe, diplopia, restriction of mandibular opening by blockage of temporal muscle or coronoid process, malocclusion and midface mobility.
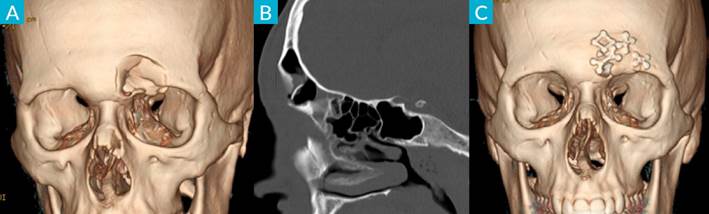
There are many classifications of zygomatic fractures, most are described on CT findings (Fig. 2).
Le Fort fractures are complex midfacial fractures that are differentiated as I, II, and III based on fracture patterns. The location of the injury, velocity, energy transfer at impact, and patient related factors determine the fracture severity and pattern.
Le Fort fractures typically occur due to blunt impact to the midface23 and can contribute to airway obstruction secondary to hemorrhage, posterior inferior displacement of the maxilla, oropharyngeal edema, and hematoma.37
Patients with midface fractures should always be evaluated by an ophthalmologist as studies have shown consistently high risks of ocular injury.34,38 Definitive management of ZMC fractures depends on the pattern of injury including degree of displacement, presence of other facial fractures, age, and degree of cooperation anticipated.28 Some fractures are nondisplaced or minimally displaced not requiring surgical intervention. Observation, soft diet, pain control, and avoidance of any activities that might further displace the bones involved, are the precautions needed after this type of fracture.
Zygomaticomaxillary complex fractures with displacement, especially those that impact form and/or function, should be surgically treated. Goals of fracture repair are restoration of normal facial contour, orbital volume, and occlusion. This type of fractures is managed with open reduction and internal fixation via combinations of intraoral, eyelid, and coronal incisions depending on the amount of exposure necessary. In the athlete, an important goal is safe and timely return to play; the need for open or closed surgical intervention can impact when an athlete can return to competition.22 In general, open reduction requires longer downtime compared with closed approaches.22
Mandible fractures
Mandible fractures are among the most common facial skeleton fractures. Patterns of fracture are highly dependable on the direction of trauma and inflicted forces. Mandibular body, condylar and subcondylar fractures more commonly result from falls and motor vehicle accidents causing anterior-posterior force. Angle and ramus fractures tend to occur from lateral force such as during assault.39 The most common fracture in the mandible is the condylar fracture (28%), followed by the mandibular angle (27%), symphysis (21%), mandibular body (17%), alveolus (4%), ramus (2%) and finally the coronoid process (1%).28
The primary goal in mandible fracture’s treatment is to restore occlusion and facial appearance. Incomplete fractures with no occlusion alterations can be managed by soft diet alone.
For horizontal portion and angle mandible fractures the most common method of treatment is ORIF (open reduction and internal fixation)28 (Fig. 3). There is the option of MMF (maxillomandibular fixation) with Erich Bars or immobilization screws for the treatment of these fractures, but it requires higher patient compliance, with 2-3 weeks of liquid diet and no mouth opening.
For subcondylar and condylar fractures, unlike other areas of the mandible, restoration of the condylar segment to its preinjury position is not required for the function to be restored.39 There are 3 options of treatment: conservative treatment with soft diet and jaw exercises, closed treatment with MMF and ORIF.
Condylar displacement into middle cranial fossa, invasion by foreign body, lateral extracapsular displacement of condyle, malocclusion not amenable to closed reduction are absolute indications for ORIF. This treatment method is strongly advised in bilateral condylar fractures, gross condylar displacement >45º (severely displaced), anatomic reduction of ramus height ≥2 mm, condylar fractures with an unstable base (associated midface fractures), unstable occlusion (e.g., periodontal disease, less than three teeth per quadrant) and condylar fractures for which adequate physiotherapy is impossible. Closed reduction is advised in nondisplaced or incomplete fractures, isolated intracapsular fractures, condylar fractures in children (except for absolute indications), reproducible occlusion without drop back or with drop back that returns to midline on release of posterior force and medical illness or injury that inhibits ability to receive extended general anesthesia.40
Dentoalveolar fractures
Dentoalveolar trauma has a significant physical, economic, and psychosocial burden on the individual. The discrepancy of access and affordability to indicated dental services often means that patients do not present to a dentist in the correct time frame for the best management.41
Those fractures can be classified in dentoalveolar injury when only the dental tissues are affected and alveolar injury when there is luxation or avulsion of the teeth.
Dentoalveolar injuries are treated by dentists and the management ranges from simple crown restoration to root canal treatment depending on the pulp affection.
Isolated luxation injuries are treated with splinting for 2 weeks but when a multiteeth segment is involved there is need for a rigid fixation for 3 to 4 weeks. In case of teeth avulsion, the tooth should be reimplanted in the first 2 hours and splinted for 7-10 days. Root canal treatment may be necessary.42
Return to play and protective devices
The subject of return to play is critical for all types of sports injuries, but unfortunately there is a lack of evidence-based studies on return to play after facial trauma, and currently no specific guidelines exist.
Literature focusing on facial fractures and return to normal activities traditionally recommends a minimum period of 6 weeks (or 8-12 weeks in case of contact sports). That is derived from an understanding of the cellular processes during bone fracture healing, demonstrating that complete fracture healing takes approximately 6 weeks to be complete.43
However, in practice there is visible variation, with surgeons recommending time to return to sports between 3 to more than 12 weeks.44
The topic of return to sports is particularly important for the professional athlete since athletic careers can be put in jeopardy by unnecessarily long absences from training and competition after facial injuries. Recently, there has been an increasing number of studies on early return to sports, especially in the context of competitive sport, with still somewhat mixed conclusions.
Roccia et al proposed a stepwise protocol to allow early return to play. It starts with abstention from any sports activities during the 3 weeks after surgical treatment, light aerobic exercise for the next 10 days and noncontact training drills for the next 10 days.45
Fowell et al provided one of the first contributions to even earlier return to sport than the one proposed by Roccia, with a prospective study that demonstrated the possibility of return to play only 3 weeks after injury/treatment with zero complications reported.46
There are also some studies that suggest a return time to sports according to the fracture site. Recommendations based on a consensus meeting with the surgeons of the British Association of Oral and Maxillofacial Surgery suggest return to sports after 1-2 weeks for isolated mandible fracture following ORIF, 3 weeks for isolated orbital floor, 3 weeks for zygomatic fractures or 1 week if ORIF has been performed and immediately after the pain has subsided for nasal fractures.21
It should be noted that contact sports, namely boxing, have their own timeline, and a longer recovery time should be considered (e.g. the British Boxing Board of Control does not allow return to sport for at least 28 days).
The majority of authors agree that recovery time should be personalized and should follow a graded protocol. Of note is a recent systematic review from Ansari et al that summarizes the recovery times from different fractures and sports for the professional athlete (Table 1).47
Another much debated topic within sport related facial injuries is the role of protective equipment. Protective equipment is intended to dissipate the impact force through the surrounding orofacial structure although scientific evidence for this is still scarce.47 Protective equipment can be used for primary trauma lesion prevention or in the context of early return to play.
Protective equipment is essentially divided into eye protection, oral protection, helmets and face guards. According to Black et al eye protection reduces eye injury risk by 69%-84%, oral protection reduces risk of dental injury by 43%-89% and helmets/face guards reduces risk of facial injuries by 28%-60%.48
Despite the low evidence particularly related to facial fractures, some countries require the use of prophylactic protective equipment for particular sports, in particular mouthguards in boxing, helmets in cycling and face masks in paintball.49
In addition to prophylactic use, protective equipment can be used as a rehabilitation device, when there is a need for an early return to sport.50 Its application is most described in professional football, with the use of face masks advised for about 1 month after nasal bones fracture.51
Although apparently useful in reducing the risk of injury, it must be taken into consideration that strong evidence does not exist and that the protective equipment also has its disadvantages, mainly the risk of false security and consequently use of greater force against the protected player49 and also, as referred by some players, the sensation of being targeted when wearing protective equipment.45
Ultimately, the return to sport must be evaluated on a case-by-case basis, depending on the type of fracture, the risk of impact within the sport, the player's motivation for an early return and the surgeon's knowledge and experience.
Table 1: Summary of study recommendations.
| Publication | Level of evidence | Conclusion and Recommendations | |
|---|---|---|---|
| Day/s | Recommendation | ||
| Fowell and Earl (2013) | 3 | 0-2 3-7 8-14 15-21 >21 | Complete rest post-surgery Moderate aerobic exercise Full fitness (nil contact or ball work) Sports-specific work, build to full training Return to sport Use of facemasks may be unpopular with players |
| Procacci et al (2009) | 4 | 0-30 | Customized facial protection to be worn post-surgery |
| Roccia et al (2008) | 4 | 0-20 21-30 31-40 >41 >90 | Abstention from activity post-surgery Light aerobic exercise Noncontact training drills Resumption of noncombat sporting activities Resumption of combat sporting activities |
| Walsh and Cooper (2008) | 4 | - | Multiple facial fractures require custom fitted face shield |
| Karsteter and Yunker (2006) | 4 | - | Face shield may allow earlier return to sport |
| Morita et al (2007) | 4 | - | Custom fitted facial guards may facilitate an early return to sport and should be worn for 1 month post-surgery It may be useful is craniofacial surgeons themselves produce facial guards |
| Koloskie and Orr (1992) | 4 | 0 1-3 >3 28 | Surgery Shooting Free throws Return to Competitive sport Hockey Helmet for training, face masks for games Fitted mouthpiece |
| Patel et al (2017) | 5 | 0 0-7 70-84 | Possible immediate return to the game if there is haemostasis, no airway blockage, no concomitant facial fracture, no suspicion of cerebral injury Return to sport post minimally displaced nasal fracture (nonoperative treatment) with facemask worn for 4 weeks Postoperative fixation, facemask to be worn for 6 weeks Post operative fixation return to sport for patients participating in combat sports |
| Marston et al (2017) | 5 | 0-42 >42 | No competitive sports post reduction of nasal fracture Earlier return possible with protective facemasks Return to competitive sports |
| Viozzi (2017) | 5 | 10-14 >56, ideally >84 | Aerobic and strength training post mandibular fracture, avoid contact or training that could induce clenching teeth vigorously Return to sport that may impact face, including soccer or hockey Use protective headgear, and custom-made mouth guard for mandibular teeth Associated ocular injury may extend recovery periods |
| Romeo et al (2005) | 5 | 0-28 0 | Return to sport post nasal fracture with protective device in contact sports Return to sport post nasal fracture if haemostasis is maintained |
| Reehal (2010) | 5 | - | Protective facemask is a possible option for sooner return |
| Cascone et al (2008) | 5 | - | Protective facemask can shorten recovery period |
| Petrigliano and Williams (2003) | 5 | 0-21 21-42 >42 | Nil activity post orbital fracture surgery Light Lifting Return to sport with protective eyewear |
| Mahmood et al (2002) | 5 | 21-84 42 | Range of surgeon recommendation on resumption of contact sport post zygomatic fracture Most common recommendation to resume contact sports post zygomatic fracture |
Conclusion
Sports-related facial injuries vary from simple to complex injuries with different impacts on long-term health of athletes. Health care providers in a sports medicine setting should understand the most common facial injuries and identify emergent conditions. Multidisciplinary evaluation in the hospital may be required.
Return to play guidelines and orientation for the usage of protective equipment after facial fractures still do not exist. Individual assessment depending on type of fracture, sport, player motivation and surgeon experience should guide the medical decision.