To the Editor:
We present a case demonstrating the possibility of manifestations of extragenital lichen sclerosus (LS) with angiokeratoma-like changes.
A 53-year-old woman developed a pruritic and infiltrated cutaneous lesion near the angle of the left shoulder blade, with sudden and progressive onset. It was a well-delimited plaque measuring 5 × 10 cm, hypochromic but with brownish hyperpigmentation at the periphery, with a marble-like and pearly white appearance and purplish areas on the center (Fig. 1A). Dermoscopy showed fibrotic beams/white clouds, yellow-white follicular plugs, in addition to vascular structures of dotted and comma-like formats (Fig. 1C).
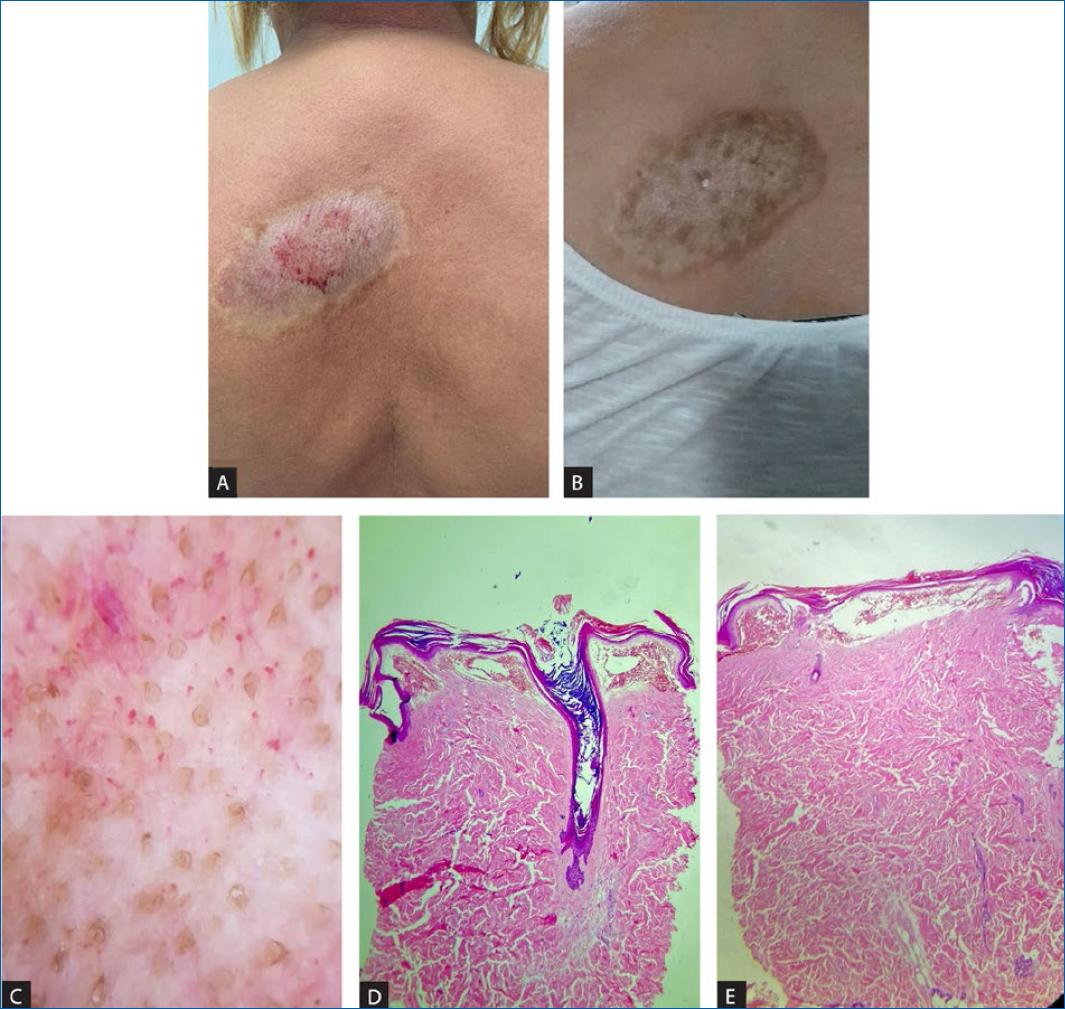
Figure 1 A: a well-delimited hardened, plaque measuring 5 x 10 cm, hypochromic, with a marble-like appearance, pearly white appearance, and purplish areas on the center. B: with improved consistency and texture and partial repigmentation after 6 months of treatment. C: dermoscopy showing fibrotic beams/white clouds, yellow-white follicular plugs and dotted and comma-like vascular structures. D and E: histopathology (H&E, 40x): D: rectified and thin epidermis, with orthokeratotic hyperkeratosis and follicular hyperkeratosis and E: vascular ectasia in the upper dermis with extravasation of red blood cells and overlying hyperkeratosis.
The clinical hypothesis of extragenital LS supported by dermoscopy was further confirmed by histopathology which revealed a rectified and thin epidermis, with orthokeratotic hyperkeratosis and follicular hyperkeratosis, marked vascular ectasia in the superficial dermis with extravasation of red blood cells in the subepidermal region and diffuse sclerosis in the middle and deep dermis (Figure 1D and E), findings compatible with LS-like angiokeratoma.
Treatment with clobetasol propionate 0.05% cream twice a day for 30 days was followed by once at night for a further 30 days, in addition to emollients. Due to relapsing pruritus, treatment with betamethasone dipropionate cream and tacrolimus ointment 0.1% in alternate days was maintained for 6 months, with improvement of pruritus, consistency and texture, and with partial lesional re-pigmentation (Fig. 1B). No other lesions were detected, namely in the genital area, nor any other concomitant pathology.
Lichen sclerosus (LS) affects mainly the anogenital area, but it occurs in the extragenital areas in about 15-20% of cases, most commonly on the thighs, neck, breasts, trunk and back1 Despite being more frequent in Caucasians2 and in women between 50 and 60 years3, its occurrence is independent of age, race and sex4.
Characteristic lesions are asymptomatic ivory or porcelain-white shiny papules and macules that coalesce to form sclerotic plaques5. Diagnosis of LS is usually clinical and can be supported by dermoscopy and, in cases with unusual lesions, by histopathology6. Findings suggestive of LS on dermoscopy include areas of erythema, linear irregular red vessels, bright white or white-yellowish patches, yellowish-white keratotic follicular plugs, whitish scaling, hemorrhagic spots, and crystalline structures7. Furthermore, as in the present case, vascular structures of different lengths and shapes have also been reported6.
Most frequent histological findings include hyperkeratosis, epidermal atrophy, hyalinosis, follicular plugging, dermal edema, basal cell vacuolization, and inflammatory infiltrate8, but vascular ectasia associated with extravasation of red blood cells in the superficial dermis, similar to angiokeratoma, can also be observed.
Angiokeratomas are superficial vascular ectasias with overlying hyperkeratosis, which manifest as single or multiple red-purple to black nodules. LS can present secondary angiokeratoma-like changes, which are due to the damage caused to the dermis by inflammation. These ectatic thin-walled vascular spaces are observed in the papillary dermis intimately associated with the epidermis5.














