A Caucasian 70-year-old male was observed with macroglossia with hemorrhagic spots and dental impressions on the border of the tongue, eyelid ecchymosis (Fig. 1), multiple brownish, lichenified papules and plaques, and diffuse ecchymosis on the neck and upper trunk (Fig. 2). Lesions were pruritic and progressively developed during 6 months. No systemic symptoms, except fatigue.

Figure 2 Diffuse ecchymoses and brownish lichenified papules and plaques, in cervical region and trunk.
Skin biopsy of a papular lesion on the upper trunk showed epidermal atrophy and diffuse dermal deposition of proteinaceous amorphous material colored with Hematoxilin & Eosin (HE) and further enhanced with Congo red stains (Fig. 3). This material showed green birefringence peculiar on polarized microscopy.
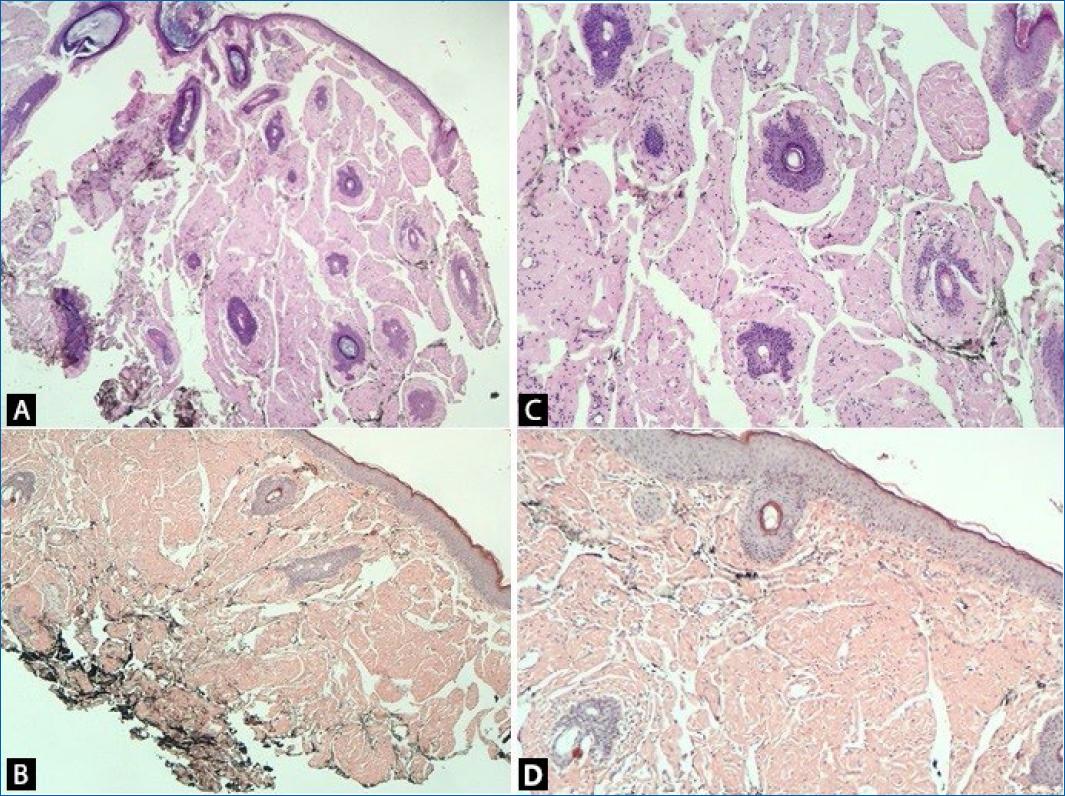
Figure 3 Histopathological examination. A and B: positive protein material in HE. C and D: Red Congo stains.
Protein electrophoresis showed a peak of gamma fraction and immunofixation showed a monoclonal IgGK, with normal IgA and IgM. Bone marrow (BM) biopsy showed hypercellularity for age (in the three hematopoietic series) and the immunohistochemically panel showed BM infiltration by plasma cell neoplasia with evident lambda light chain restriction, confirming the diagnosis of multiple mieloma (MM). Neither osteolytic lesions nor the involvement of any other organ were detected.
The diagnosis of light chain (AL) amyloidosis associated with MM was done. The patient is being followed up together with onco-hematology staff, undergoing chemotherapy with Melphalan® and Prednisone, with satisfactory evolution (important improvement in pruritus and mucosal lesions, stability of skin lesions, and the patient’s general condition).
Discussion
Amyloidosis comprises a heterogeneous group of diseases with extracellular amyloid deposits1. AL amyloidosis occurs in 5-26 % of patients with MM1,2, and originates from the deposition in the skin and other organs of amyloid substance derived from monoclonal light chain immunoglobulins, leading to a plethora of clinical symptoms, and eventually vital organ dysfunction3. Lambda light chains are the most involved (3:1);3-5 however, in the present case kappa light chain was preponderant.
The age range of involvement is between 50 and 70 years, with a slight male predominance5. The clinical manifestations are variable and nonspecific (weight loss, fatigue, paresthesia, and syncope) contrasting with highly suggestive dermatological manifestations: macroglossia with tongue hardening, with or without bleeding spots and blisters in the oral cavity; periorbital ecchymosis (raccoon sign) and ecchymosis due to minor trauma in the folds; translucent, purpuric and/or brownish papules on the scalp, face, neck, and fingertips; which may be the only manifestations of the disease prior to later-stage organ involvement, at which point treatment options are limited1-6.
All forms of amyloid show a peculiar green birefringence on microscopy after staining with Congo red, the gold standard for diagnosis5,6.
In the present case, the histopathological examination (HE and Congo red) and the monoclonal peak of the gamma fraction on protein immunoelectrophoresis confirmed the diagnosis of AL amyloidosis. Hypercellularity for age in the BM biopsy and the immunohistochemical panel showing BM infiltration by plasma cell neoplasm with evident lambda light chain restriction concluded AL amyloidosis was associated with MM.
As for the treatment, it aims to reduce the proliferation of the clonal B cell lineage and consequently the amyloid deposit, being the same used for MM (in the present case Melphalan® associated with Prednisone)1,6. Prognosis reserved1,5,6.
The rarity of this case (association), the importance of early diagnosis (minimizing/delaying the amyloid deposit) and the fundamental role of the dermatologist in this context, motivated this report.















