Introduction
Cystic lymphangioma (CL) is a rare benign tumor resulting from a failure in the development of the lymphatic system, which occurs more typically during childhood1. They consist of dilated lymphatic channels forming multiple cysts of variable size (macro- or microcystic lymphangioma), with craniofacial, cervical, or axillary being the most common locations1,2. Surgical excision has been historically considered the treatment of choice, but today less invasive therapeutic options are preferred2.
Sirolimus is an antitumor agent that belongs to the mammalian target of rapamycin (mTOR) inhibitors group, it blocks the mTOR/PI3K pathway and reduces the production of vascular endothelial growth factor (VEGF) and responsiveness of its receptors, thus inhibiting abnormal vascular proliferation. Sirolimus and other mTOR inhibitors are predicted to be effective agents in disorders in which the mTOR growth control pathway is affected2,3.
We present the case of a 3-year-old boy treated with oral sirolimus for a cervical CL.
Case description
A 3-year-old, previously healthy boy was referred to the pediatric outpatient clinic due to a right cervical mass, first noticed at the age of 17 months.
Physical examination was remarkable for a voluminous cervical mass on the right side, with approximately 6 cm (Fig. 1) with no other significant findings.
The ultrasound of the mass revealed a cystic multiloculated image, with anechogenic content measuring 77.7 x 65 x 29 mm and permeating through the cervical structures, below the parotid, posteriorly to the submandibular gland and around the jugulo-carotid space. Magnetic resonance imaging (MRI) confirmed the existence of a right cervical mass consistent with a CL with 6.7 x 6 x 5.2 cm (Fig. 2).
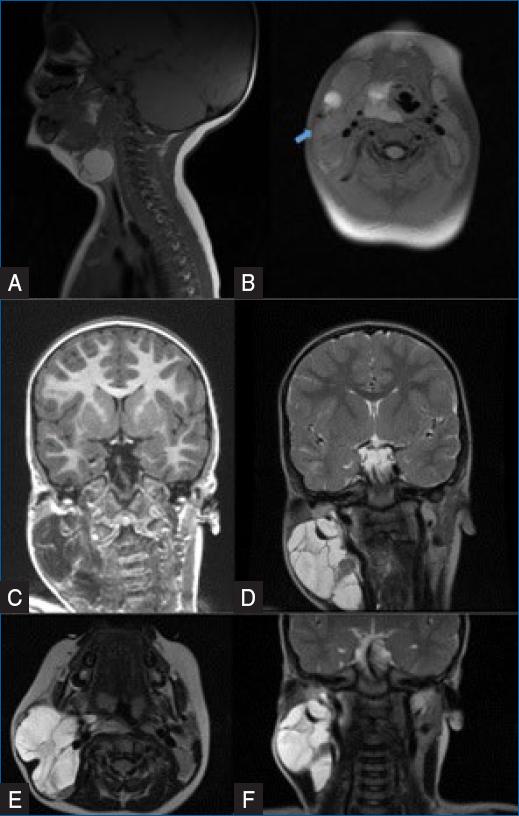
Figure 2 A and B-top: MRI images of the lymphangioma at the date of diagnosis. Bottom-C, D, E, and F: immediately before treatment with sirolimus was started.
Treatment with sirolimus was started at 1 mg/m2/dose twice daily. Regular monitoring was carried out with no adverse effects reported.
After 1 year and 3 months of treatment, an important reduction of the mass was achieved (Figs. 3A and B). An MRI showed a significant reduction of the right cervical CL (40 x 28 x 40 mm (Figs. 4A and B).
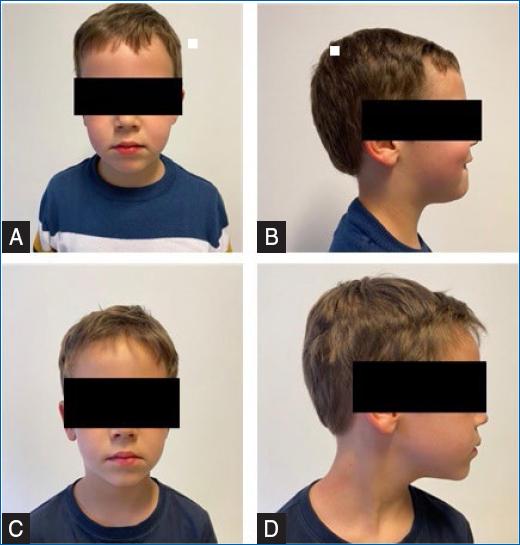
Figure 3 A and B: picture of the patients after 1 year. C and D: 2 years of treatment with sirolimus, both with no visible mass.
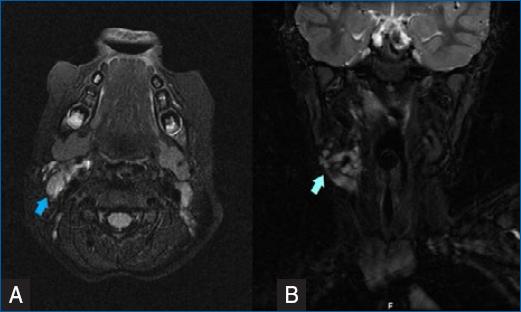
Figure 4 A and B: MRI images of the lymphangioma that was significantly reduced after treatment with sirolimus (blue arrow).
The patient maintains treatment with sirolimus after 2 years and 3 months with no side effects, and clinically he has no visible mass (Figs. 3C and D).
Discussion
It has been suggested that both the occurrence and development of CLs are caused by somatic activating mutations in PIK3CA. This mutation leads to an abnormal activation of the phosphatidylinositol-3'-kinase (PI3K)/AKT signaling pathway, which is critical in controlling cell growth and proliferation during development and has been implied in multiple syndromes with tissue overgrowth. Activation of mTOR signaling increases the expression of VEGF, therefore contributing to increased angiogenesis and lymphangiogenesis3.
Lymphangiomas management can be challenging due to their permeative growth throughout tissue layers. To date, there is no uniform guideline for the treatment of CL, which currently intends to control related symptoms, maintain functionality, and preserve aesthetic integrity4.
Sirolimus, also known as rapamycin, is a serine/threonine kinase that regulates the signaling pathway PI3K/AKT/mTOR. It is typically well tolerated3,4, with the most significant adverse effects being nausea, cytopenia (thrombocytopenia and anemia), and metabolic imbalances (hyperglycemia, hypercholesterolemia, elevated alkaline phosphatase, elevated serum creatinine, and hypophosphatemia)2, especially in the beginning of the treatment.
There have been reports of the successful use of sirolimus in children with vascular malformations1-4. The possibility of oral administration with a comfortable scheme (two administrations daily) makes it easy for parents to administer and stimulates compliance to treatment.
The optimal timing of treatment is yet to be determined, as there are no sufficient studies to state when to stop oral sirolimus in CLs.
In the case we described, there was good compliance to therapy and tolerance with no significant side effects reported during follow-up, adding evidence of the effectiveness and safety of oral sirolimus in the treatment of CLs.















