Introduction
Superficial mycoses or Tinea are fungi infections preferentially affecting the epidermis and its annexes1, caused by dermatophytes, which include genera Microsporum, Trichophyton, and Epidermophyton2. All dermatophytes share morphological and physiological peculiarities in relation to the affected body region. These species have keratinophilic affinity and can cause pathology in humans and animals3.
Dermatophytosis affects approximately 20% of the world population, particularly in tropical and subtropical regions. Geographic location, weather, cultural factors (e.g., exposure to domestic animals), socioeconomic conditions, and personal hygiene practices contribute to epidemiological differences between distinct regions4,5.
Fungi can be found in humans, animals, and in the environment. Transmission can occur through direct contact with sick animals or humans or carriers, or even with contaminated objects or environments such as hairbrushes, bedding, carpets, or other contaminated surfaces. The diagnosis of dermatophytosis is clinical, based on anamnesis and physical examination. However, in cases of uncertain diagnosis or treatment failure, direct mycological exam and culture are useful tools to confirm the infection6.
The clinical picture varies on the affected body region and the previous use of topical medications. The relevant forms of infection are Tinea capitis, Tinea corporis, Tinea cruris, Tinea unguium and Tinea pedis. Tinea capitis affects children more frequently and is uncommon in adults. It can cause conditions that range from an isolated or a group of circular pseudoalopecia and scaly lesions (tonsurans) to an intense inflammatory form of high morbidity (kerion). Erythematous plaques associated with an annular border with desquamation and papules and central healing characterize Tinea corporis and Tinea cruris. Tinea unguium or onychomycosis occurs due to invasion of the nail plate and leads to discoloration, hyperkeratosis and fragility of the nails. The appearance of grooves, roughness and fractures, with a yellowish appearance is typical for nail infection7.
Available topical therapies include agents such as azoles, allylamines, butenafine, ciclopirox, and tolnaftate. Oral treatments namely terbinafine, itraconazole, fluconazole, or griseofulvin are reserved for extensive or refractory skin infections and infections that extend to follicles or nails. It is noteworthy that oral ketoconazole increases the risk of severe liver damage, adrenal insufficiency and drug interactions8.
One of the primary concerns of patients is pruritus. In severe forms, it can affect patient's quality of life and the condition can extend and become chronic if treatment is not adequate. Another major impact is the aesthetic aspect, always present in dermatological diseases, because of the clear visibility of the lesions. This limits social interaction and contributes to the loss of quality of life. Considering the prolonged treatment in some forms of tinea, this can cause a financial burden and make it difficult to adhere to treatment9.
Due to the significant prevalence of dermatophytosis in Brazil, especially in the Amazon region, it is of great importance to know the main epidemiological, clinical, and therapeutic aspects in services of reference and excellence in dermatology. Early diagnosis and adequate treatment prevent quality of life reduction in the affected population.
Methods
Ethical aspects and type of study
This is an observational, descriptive, cross-sectional, unicentric study carried out at the dermatology service of the Center for Biological Sciences and Health of the Universidade do Estado do Pará, in Belém, Pará, one of the reference centers for general and tropical dermatological diseases in Amazon region. University's Research Ethics Committee (opinion No. 3,853,185) approved and authorized this research.
Casuistry
The study sample consisted of all patients evaluated at the dermatology outpatient clinic between January 2016 and January 2020, who had a clinical diagnosis of dermatophytosis, regardless of the causative species, location, age and sex, or previous medication use. 75 medical records were analyzed. We performed direct mycological examination and culture only in cases in which the clinical diagnosis was insufficient and there was a need for complementary semiology. Patients with incomplete medical records, as well as those whose diagnosis of dermatophytosis was ruled out after direct mycology and/or culture, were excluded from the study.
Data collection
The authors used a standardized protocol to collect and analyze medical data. The variables collected were epidemiological data and occupation, clinical aspects, type of treatment, recurrence, and presence of comorbidities.
Data analysis
Regarding statistical analysis, Chi-square test of adherence was used. p-value < 0.05 or 5% was considered statistically significative. Significant values were indicated with an asterisk (*). We used Microsoft Word 2016 and Microsoft Excel 2016 software to process the manuscript, graphs, and tables.
Results
The sample comprised 75 patients during the years 2016–2020. Data analysis showed a predominance of females (66.67%) and a mean age of 49 years (Table 1).
Table 1 Sociodemographic characteristics of patients with dermatophytosis treated at a reference service, 2016–2020
| Sociodemographic characteristics | n | % | p-value |
|---|---|---|---|
| Gender | |||
| Male | 25 | 33.33 | Chi-square |
| Female | 50 | 66.67 | 0.0056* |
| Age group | |||
| Under 18 | 20 | 26.67 | Chi-square |
| 19-29 years | 3 | 4.00 | < 0.0001* |
| 30-39 years | 6 | 8.00 | |
| 40-49 years | 9 | 12.00 | |
| 50-59 years | 9 | 12.00 | |
| 60 years or older | 28 | 37.33 | |
| Mean ± standard deviation | 49 ± 26.41 | ||
| Occupation | |||
| Retired | 9 | 12.00 | Chi-square |
| Domestic worker | 9 | 12.00 | 0.0092* |
| Dressmaker | 3 | 4.00 | |
| Domestic | 2 | 2.67 | |
| Student | 15 | 20.00 | |
| Others | 12 | 16.00 | |
| No information | 25 | 33.33 | |
As resources for the statistical analysis, the Chi-square test of adherence was used and for decision making, a p-value < 0.05 or 5% was adopted, signaling with an asterisk (*) the significant values.
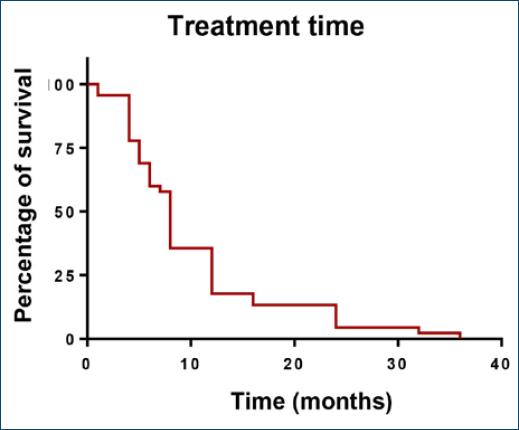
The dominant type of dermatophytosis diagnosed was onychomycosis (49.33%), followed by Tinea capitis (24.0%) (Table 2). Most patients were treated with topical and systemic medications in combination (75%). Griseofulvin (28%) and terbinafine (25.33%) were the most prescribed for systemic treatment and, as preferred topical medication, Ciclopirox olamine was chosen in 36% of cases (Table 3). As for patient follow-up, after starting treatment, 77.33% attended follow-up appointments, 75% of them for 10 months or less, while approximately 10% for over 20 months (Fig. 1).
Table 2 Clinical characteristics of patients with dermatophytosis treated at a referral service, Belém–Pará, 2016–2020
| Clinical features | n | % | p-value |
|---|---|---|---|
| Type of dermatophytosis/agent* | |||
| Onychomycosis | 37 | 49.33 | Chi-square |
| Tinea capitis | 18 | 24.00 | < 0.0001* |
| Tinea corporis | 15 | 20.00 | |
| Tinea cruris | 5 | 6.67 | |
| Tinea pedis | 9 | 12.00 | |
| Number of lesions | |||
| 1 | 21 | 28.00 | Chi-square |
| 2-5 | 19 | 25.33 | 0.0059* |
| 6-10 | 4 | 5.33 | |
| More than 10 | 21 | 28.00 | |
| No information | 10 | 13.33 | |
| Return inquiry | |||
| Yes | 58 | 77,33 | Chi-square |
| No | 17 | 22,67 | < 0.0001* |
| Previous clinical condition | |||
| Yes | 5 | 6.67 | Chi-square |
| No | 13 | 17.33 | 0.0990 |
| No information | 57 | 76.00 | |
| Recurrence in less than 1 year | |||
| Yes | 19 | 25.33 | Chi-square |
| No | 23 | 30.67 | 0.6434 |
| No information | 33 | 44.00 | |
*The same patient may have been affected by more than one dermatophytosis/agent.
Table 3 Treatments for dermatophytosis in patients treated at a reference service, 2016–2020
| Treatment | n | % | p-value |
|---|---|---|---|
| Carrying out treatment | |||
| Yes | 72 | 96.00 | Chi-square |
| No (other diagnosis) | 3 | 4.00 | < 0.0001 |
| Type of treatment | |||
| Systemic | 7 | 9.72 | Chi-square |
| Topic | 11 | 15.28 | < 0.0001 |
| Combined | 54 | 75.00 | |
| Type of systemic treatment* | |||
| Fluconazole | 17 | 22.67 | Chi-square |
| Griseofulvin | 21 | 28.00 | 0.0040 |
| Itraconazole | 3 | 4.00 | |
| Topical treatment* | |||
| Amorolfine | 11 | 14.67 | Chi-square |
| Butenafine | 12 | 16.00 | < 0.0001 |
| Ketoconazole | 9 | 12.00 | |
| Ciclopirox olamine | 27 | 36.00 | |
| Clotrimazole | 1 | 1.33 | |
| Fenticonazole | 2 | 2.67 | |
| Piroctone olamine | 2 | 2.67 | |
| Selenium sulfide | 1 | 1.33 | |
*The same patient may have used more than one type of systemic/topical treatment.
In 57.33% (n = 43) of the patients, a direct mycological examination was performed and 40 patients (93.02%) confirmed the clinical suspicion (Table 4).
Table 4 Laboratory characteristics of patients with dermatophytosis treated at a reference service, 2016–2020
| Laboratory characteristics | n | % | p-value |
|---|---|---|---|
| Mycological examination | |||
| Yes | 43 | 57.33 | Chi-square |
| No | 31 | 41.33 | 0.2010 |
| No information | 1 | 1.33 | |
| Direct mycological test result | |||
| Yes | 40 | 93.02 | Chi-square |
| Negative/inconclusive | 3 | 6.98 | < 0.0001 |
| Culture performed | |||
| Yes | 2 | 2.67 | Chi-square |
| No | 72 | 96.00 | < 0.0001 |
| No information | 1 | 1.33 | |
Some characteristics correlated with dermatophytoses, such as domestic animals and family members affected by a similar condition. However, most medical records did not report this information. There were only descriptive results of comorbidities, because many categories had a very low number of patients (Table 5).
Table 5 Characteristics associated with the development of dermatophytosis in patients treated at a reference service, 2016–2020
| Associated features | n | % | p-value |
|---|---|---|---|
| Animals at home | |||
| Yes | 3 | 2.67 | Not applicable |
| No | 2 | 1.33 | |
| No information | 70 | 96.00 | |
| Affected family members | |||
| Yes | 5 | 4.00 | Chi-square |
| No | 3 | 2.67 | < 0.0001 |
| No information | 67 | 93.33 | |
| Comorbidities | |||
| Yes | 20 | 26.67 | Chi-square |
| No | 17 | 22.67 | 0.7423 |
| No information | 38 | 50.67 | |
| Type of comorbidity* | |||
| Asthma | 2 | 2.67 | Not applicable |
| Diabetes mellitus | 10 | 13.33 | |
| Dyslipidemia | 1 | 1.33 | |
| Viral hepatitis | 2 | 2.67 | |
| Arterial hypertension | 11 | 14.67 | |
| Heart disease | 1 | 1.33 | |
| Lymphoma | 1 | 1.33 | |
| Vitiligo | 1 | 1.33 | |
| Immune thrombocytopenic purpura | 1 | 1.33 | |
*The same patient may have had more than one comorbidity.
Discussion
Data showed a female predominance. This association is often correlated with women's greater demand for assistance in health services and self-care compared to the male population4,5,10,11.
The mean age of the patients was 49 years (±26.41), similar to studies carried out in another Brazilian state and in Valparaíso2. According to literature data, the most affected age group varies in relation to the type of dermatophytosis. For example, Tinea capitis is more common in children, especially in prepubertal children12, and onychomycosis, the most prevalent dermatophytosis in this study, is more prevalent in adults13. Hormonal changes during puberty that perpetuate during adulthood, such as the greater secretion of acids by the sebaceous glands and their type prevent the growth of species that cause tinea in the scalp, explaining the lower occurrence of Tinea capitis in adult and elderly patients14.
The expressive number of onychomycosis in this series is due to several reasons. The major factors associated are the age group, characteristically more affected by this location; presence of comorbidities, local components (trauma, inadequate nail care, use of closed shoes), sports activities and dermatological changes15,16. In a recent Brazilian systematic review involving 24 studies, Bodman and Krishnamurthy13 also observed that onychomycosis was the most prevalent dermatophytosis.
Topical and systemic drugs are treatment options for dermatophytosis. Most dermatophyte infections require only topical agents, whereas oral systemic treatment is recommended in extensive, refractory and/or relapsing cases and in infections with extension to follicles (e.g., Tinea capitis) and nails, as in onychomycosis1,17. In our study, 75% of the patients underwent topical and systemic treatment in combination, possibly because onychomycosis and Tinea capitis were the most prevalent, in agreement with the literature17.
Approximately 25% of the patients received treatment with terbinafine, which along with itraconazole, are drugs approved by the Food and Drug Association in the treatment of onychomycosis. Systemic drugs are a feasible treatment of onychomycosis because of their accessibility, lower cost and high efficacy18. A recent Cochrane review of oral antifungal agents in the treatment of onychomycosis showed terbinafine was more effective than azoles in achieving clinical cure with no difference in adverse effects or recurrence rates19.
The most frequently prescribed topical treatment in our study was ciclopirox olamine (36%), which is widely used in nail varnish preparations for onychomycosis, in combination with systemic treatment. Recurrence rate is higher in monotherapy. However, it is also possible to use monotherapy in cases of minimal (distal and lateral) subungual onychomycosis (less than 50% of the total nail area involved) and/or when the patient is not a suitable candidate for oral antifungal therapy20.
The second most prevalent dermatophytosis in the series was Tinea capitis. In these cases, oral antifungal agents such as terbinafine and griseofulvin are the first line of treatment. The duration of treatment ranges from 4 to 6 weeks or even 12 weeks for griseofulvin21. In our casuistic, 83.33% (n = 15) of the patients diagnosed with Tinea capitis underwent treatment with griseofulvin and all cases had clinical cure confirmed by direct mycological examination. Besides systemic treatment, in many medical records, ketoconazole or topical selenium sulfide shampoo, was prescribed to prevent the spread of the fungus22.
Regarding treatment of Tinea capitis, it is essential to identify potential sources of infection at home or in pets. Transmission between members of the same family is the most common route, mainly through contaminated fomites. In addition, zoophilic species such as Microsporum canis can cause infection after contact with infected domestic dogs and cats. Zoophilic species are more often associated with more severe and difficult-to-treat forms, such as kerion celsi21,23. In the analyzed sample, 96% (n = 70) and 93.3% (n = 67) of the medical records did not present information on the presence of affected domestic animals or family members, respectively.
Regarding follow-up, 77.33% of the patients attended successive consultations, which is essential for an effective treatment, especially in cases of onychomycosis, whose therapy is long, occasionally needs monitoring with laboratory tests and permanent cure may be difficult, as highlighted by Bentine24. Treatment duration varies according to the clinical response, type, location and extent of dermatophytosis. Another factor is the appropriate use of the drug, which can last from two weeks to several months, as in the case of onychomycosis (generally, 12 months in toenails)16. In the present study, more than half of the patients completed treatment and follow-up in less than 10 months.
The correct identification of the etiological agent by culture may be an important step as it can influence the prognosis15; however, in the present study, only 2 patients (2.67%) had fungi cultures.
Several predisposing factors facilitate the infection and spreading rate by dermatophytes, such as gender, local trauma, peripheral circulation changes, immunosuppression, occupation, hormonal changes, and even local weather25. A classic example is type 2 diabetes mellitus, because of microangiopathy, poor healing, and sensory neuropathy19,24. We identified only 26.67% (n = 20) of the patients with comorbidities, half of them (n = 10) had type 2 diabetes mellitus.
Conclusion
The present study provided demographic data, characterization of clinical aspects, and treatment regimens used in medical practice at a reference center in northern Brazil. Analyzed data emphasize the importance of early diagnosis and treatment of dermatophytosis, especially in the most fragile age groups (pediatric and elderly) and reflects how onychomycosis is most frequent in adults and Tinea capitis in children.