Introduction
As the pattern of multi-morbidity and physical and mental health disorders changes [1, 2], the need for long-term care (LTC) is expected to increase. The term “LTC” refers to a myriad of services designed to provide assistance over prolonged periods, including basic medical services, rehabilitation, social care, personal hygiene, occupational therapy, education, and psychosocial support for both patients and their caregivers [3]. Thus, an admission to a LTC setting, either an institutionalised (hereafter referred to as nursing home, NH) or non-institutionalised (hereafter referred to as home and community-based services, HCBS) environment, represents a turning point in an individual’s life, usually associated with a loss of functional independence [4]. Since LTC has been increasingly used as a post-acute care setting for individuals requiring rehabilitation and nursing services [4, 5], and the length of care (LOC) delivery is closely related to the effectiveness (and, by necessity, to the adequacy) of the care, by taking the patients’ dependency level into consideration, there is a growing interest in studying the relationship between LOC and several other features: staff mix [6-10], NH residents at the end of life [5, 11], expenditure [7, 12-15], individuals’ trajectories between care settings [2, 4, 13, 15-17], and LOC risk factors [2, 7, 8, 13-16, 18]. As for the relationship with staff mix, evidence suggests that facilities that provide higher-intensity care (e.g., number of daily hours per bed) and the number of nursing and support staff are associated with a shorter LOC [6, 9, 10]. Concerning LTC expenditure, since costs per patient are influenced by the LOC [7, 15], a financial model that does not consider variations regarding the needs of each individual could lead to a situation whereby patients with the same dependency level receive different levels of care [8]. Consequently, as also stated by Newcomer et al. [14], longer and unnecessary stays may contribute to an increase in expenditure. Information about all patients’ trajectories, including transfers between privately and publicly funded care, is helpful to identify appropriate partnerships between different settings and patterns of care [4, 13, 15, 17]. Studies from the USA concluded that stays in care homes tend to be shorter for people who have previously received domiciliary social care [15]; Long-stay residents tend to have fewer hospitalisations than Short-stay residents [17]; and among newly admitted NH residents, after a high initial community discharge rate (20% within 30 days of admission and 31% within 100 days), the majority of patients experienced a mean of 2.1 transitions in the first year, while remaining institutionalised until death or the end of 1-year follow-up [4]. Despite differences in datasets and methodologies, other reviews of the literature on the risks observed at NH/HCBS admission have also found that demographic, social, and clinical features are important predictive factors of LOC [19-21]. As for the influence of age, while some authors found no statistical significance between these variables [7, 8], recent studies have concluded that older age is associated with longer provision of care and, consequently, greater expenditure [2, 14, 17]. As for gender, mixed conclusions can be found in the literature. Some studies conclude that male gender is statistically significant with a lower LOC [5, 13, 15], while others, more recently, conclude the opposite [2, 12, 17]. Moreover, the relationship between the LOC in each setting and the geographic location where the care is provided has been assessed by several researchers [5, 12, 15]. In this case, the differences found may be a consequence of asymmetry in the regional distribution of LTC resources, either in terms of HCBS treatment places and/or NH beds. Concerning social aspects, individuals with less social support [2, 5, 11, 16], who live alone [14], or are unmarried [17] usually have longer periods of care. As for the influence of clinical features, several authors found that individuals who were more physically and cognitively impaired at admission had a longer LOC [2, 11, 13, 14, 16].
In this study, we developed statistical procedures to identify the main predictors and estimate patients’ LOC at admission, within the Portuguese National Network for Long-Term Integrated Care, by using a dataset of 20,984 patients from the national LTC system. The main points of this research may be summarized as:
LOC is mostly influenced by the type of setting to which patients are admitted;
A low level of social support is associated with a longer LOC;
Patients’ functional status at admission influences their LOC;
Patients in units with a low occupancy rate and that have been operating for a shorter time have a shorter LOC.
A second model was developed to identify the main predictors of LOC, where the death of the patient is included as an explanatory variable. Future studies and data are required to assess the relationship between the length and effectiveness of care.
The portuguese LTC system
Since LTC comprehends a myriad of services designed to provide assistance over prolonged periods of time [3, 21, 22], there is no consensus in the literature regarding its definition, types of support, organisational models, policies relating to access, and key factors needed to ensure its sustainability [22-24].
In Portugal, as recently described [25, 26], the LTC system was officially created in 2006 as a partnership of the Ministry of Health and the Ministry of Employment and Social Solidarity, and is provided in 2 main settings:
At home (HCBS) and by teams working in primary care centres, for individuals with functional dependence in need of personal hygiene and psychosocial support as well as medical, nursing and rehabilitation care, but who do not require acute care. Those requiring only social support, without any informal caregiver or with care needs during the night, are ineligible for this type of care.
At an institutional setting, i.e., in one of the three types of NH unit of care: (i) Short-stay unit, intended for individuals with an expected maximum LOC of 30 consecutive days, (ii) Medium-stay unit, for stays between 31 and 90 consecutive days, and (iii) Long-stay unit, with an expected LOC of >90 consecutive days.
Although the type, frequency, and intensity of services may vary according to people’s needs, with some needing assistance a few times a week and others needing full-time support, these units are considered as “small rehabilitations centres”. Although both settings were created to provide assistance to people who do not need acute care, the main goal of the Portuguese LTC system is to restore an individual’s (total or partial) autonomy and enable them to return to their community.
Objectives
The aim of this paper is beyond the presentation of the Portuguese LTC system. A detailed presentation can be found elsewhere [25, 26]. Despite previous research having found a positive relationship between a longer LOC and patients recovering their independence [13, 27], a recent study in Portugal concluded that the LOC has a positive but small influence on cognitive improvement but not on physical status [26].
In this work, we looked at two different but parallel research questions that have not yet been studied in a real-world context in Portugal:
What are the main predictors of patients’ LOC? Specifically, from the set of characteristics observable at admission, what are the main predictors?
Do dependency levels registered at admission influence individuals’ expected LOC?
We also investigated the possibility of estimating the expected LOC for a new individual entering the national LTC system. Since (a) there is a growing waiting list for LTC in Portugal and LOC impacts turnover, and (b) costs are associated with LOC once the care units are paid per day and per patient, this study intends to help policymakers estimate required treatment time by taking into account a patient’s level of dependency and other observable risk factors at admission. To this end, since the variable LOC considers the number of days between admission to and discharge from the LTC system, regardless of a person’s outcome, we developed two models. The first included risk factors observable at admission and estimated the LOC. With this information, policy-makers can estimate future costs and adjust resources to patients’ characteristics, so as to ensure the quality of the care provided and optimise the available resources. This information may also be used to manage patients’ expectations regarding their estimated LOC in each care setting according to their characteristics at admission. The second model, to evaluate the impact of mortality on LOC, included death as an outcome and evaluated the risk factors by taking this outcome into account.
Materials and methods
Data source
In this study, we used the national data from the Portuguese LTC monitoring system, which gathers two types of information collected by staff in all care settings and is used to develop the care plan for each individual:
Personal: information collected by means of the Bio-Psychosocial Assessment Instrument to identify the dependence level of each individual in three main dimensions (more information can be found in Lopes et al. [25]), namely: (1) biological: age, gender and functional status by testing the ability to perform eight activities of daily living (ADL) and three locomotion activities; (2) psychological: assess the ability to answer ten questions about temporal and spatial orientation; and (3) social: the availability (or not) of support from family members and/or neighbours.
Generic: type of setting of care, referral entity, region where care is provided, the number of beds/treatment places available, and the rate of occupancy and maturity of the unit (according to the number of months operating in the system and the admission and discharge dates).
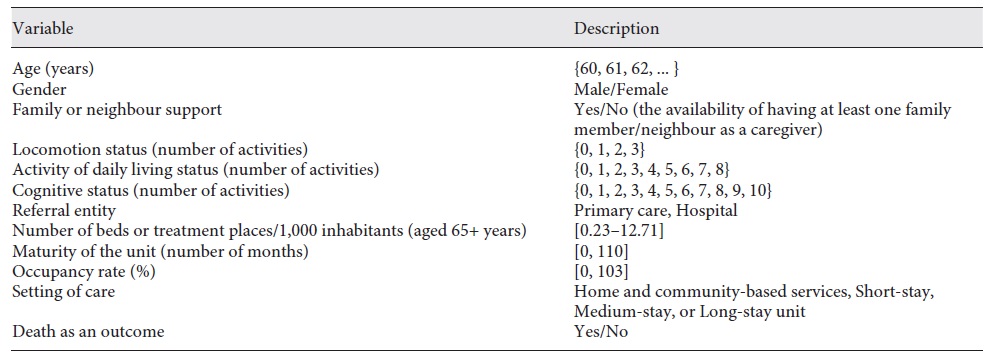
Regarding functional (locomotion and ADL) and cognitive status, each activity is assessed using a system of four scores (0-3), with 0-1 considered as “dependent” in the performance of an activity and 2-3 as “independent” [28, 29]. Considering the activities assessed in each area, locomotion status is determined by the ability to walk at home, walk in the street and climb stairs. The ADL item assesses eight activities such as going to the toilet, dressing, bathing, transferring to and from a bed or a chair, continence/urination, continence/defecation, and feeding. The cognitive status item includes questions about temporal (year, month, day, season, and day of the week) and spatial (country, province, city/town, home, and floor) orientation. Thus, the maximum number of activities in which the patient may considered “dependent” differs according to the area assessed. Table 1 describes all variables included in this research.
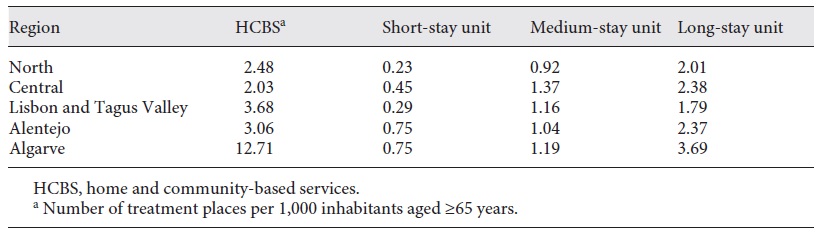
We highlight that, regarding the supply of services, we included two variables: (1) the number of beds/treatment places per 1,000 inhabitants aged ≥65 years, and (2) the occupancy rate of the unit at admission. For the first variable, the term “treatment places” refers to the maximum number of people each primary care centre can serve in each region. This variable was created by considering the dichotomy patients’ setting and region of care (represented by the Portuguese Nomenclature of Territorial Units for Statistics), reflecting the offer of LTC services and the number of inhabitants aged ≥65 years in 2015 (Table 2).
The data used was provided by the Portuguese Central Administration of Health System, the entity responsible for managing the national LTC system, which guaranteed that all identifiers, e.g., patients’ identification in each setting of care and record No., were anonymised.
Study cohort
The original dataset had information about 27,832 patients from the Portuguese public LTC system. We excluded 1,777 patients receiving palliative care; 1,924 with no information regarding gender, marital status, or family/neighbour support; 951 with no information regarding their cognitive/physical status; and 2,196 that were <60 years old. Thus, we gathered complete information about 20,984 individuals (6,844 receiving HCBS and 14,140 receiving institutionalised care), aged ≥60 years who were admitted and discharged in 2015 (on the Portuguese mainland).
Statistical analysis
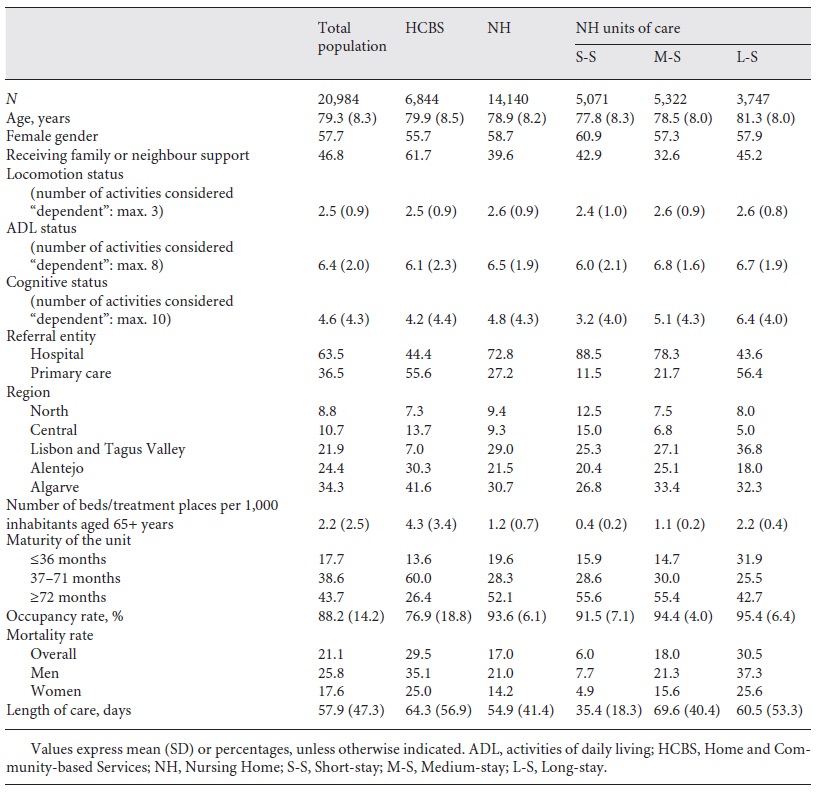
In a first approach, a preliminary descriptive analysis of the whole database was performed, considering patients’ characteristics in each care setting (Table 3). For modelling purposes and taking the substantial differences between HCBS and NH facilities into consideration, we performed a separate statistical analysis for each setting of care.
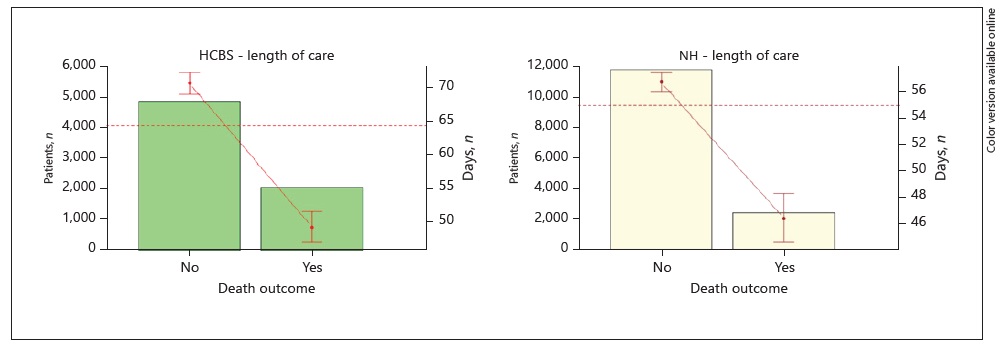
Second, we studied the relation between the LOC and several variables of interest. Figures 1, 2 provide a highly visual description of the database, highlighting several patterns regarding LOC and particular features.
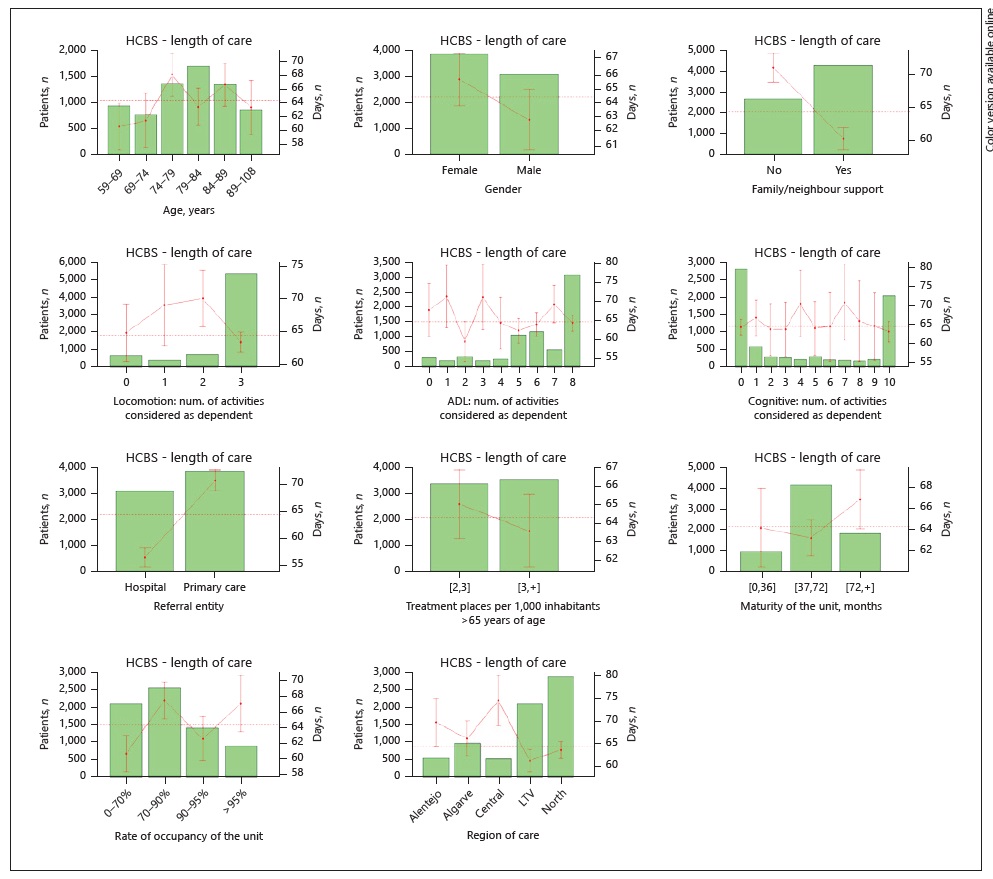
Fig. 1 HCBS. Average length of care of several variables of interest. Bars, number of patients in each group; horizontal dotted line, average LOC in days for each population; bullets, average LOC in days for each group; vertical lines, 95% CI for the expected LOC in each variable for each group. ADL, activities of daily living; num., number.
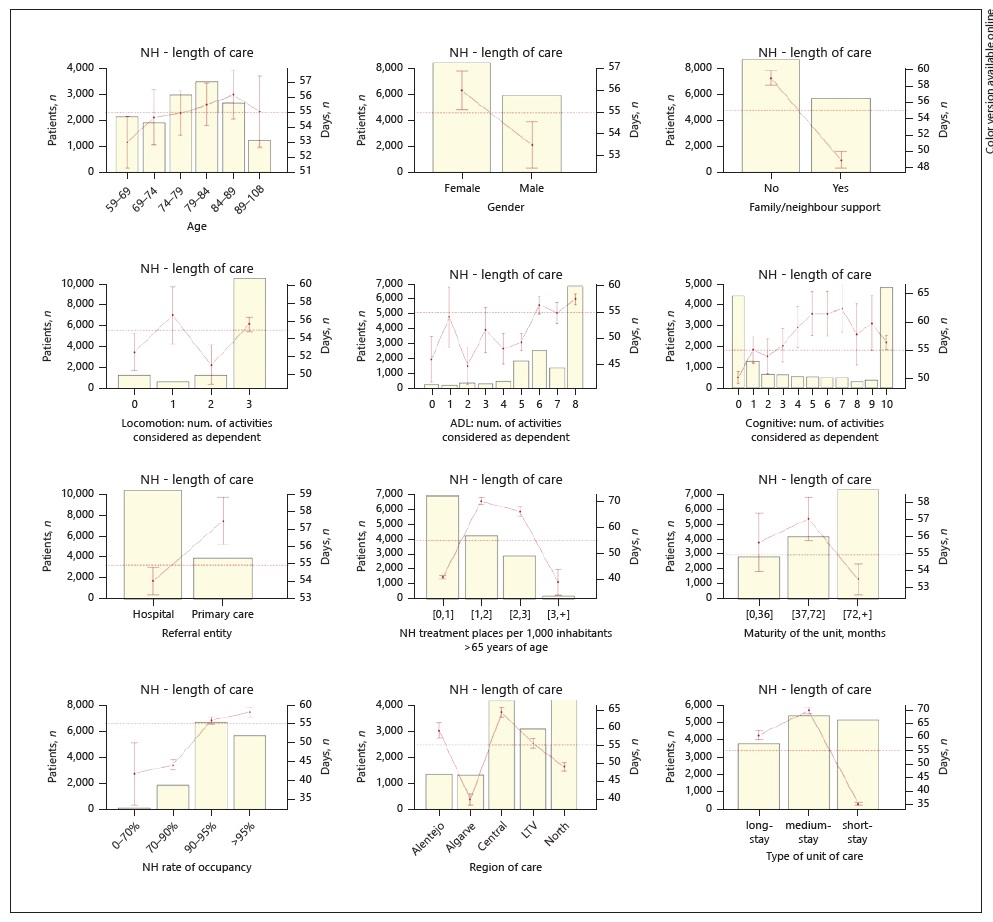
Fig. 2 NH. Average length of care of several variables of interest. Bars, number of patients in each group; horizontal dotted line, average LOC in days for each population; bullets, average LOC in days for each group; vertical lines, 95% CI for the expected LOC in each variable for each group.
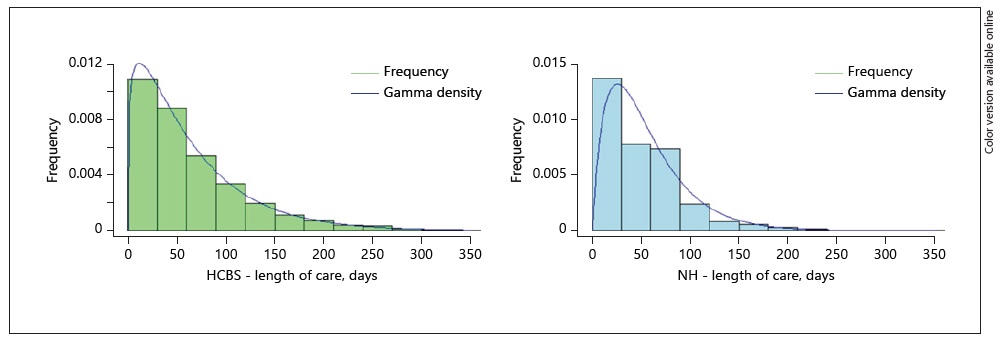
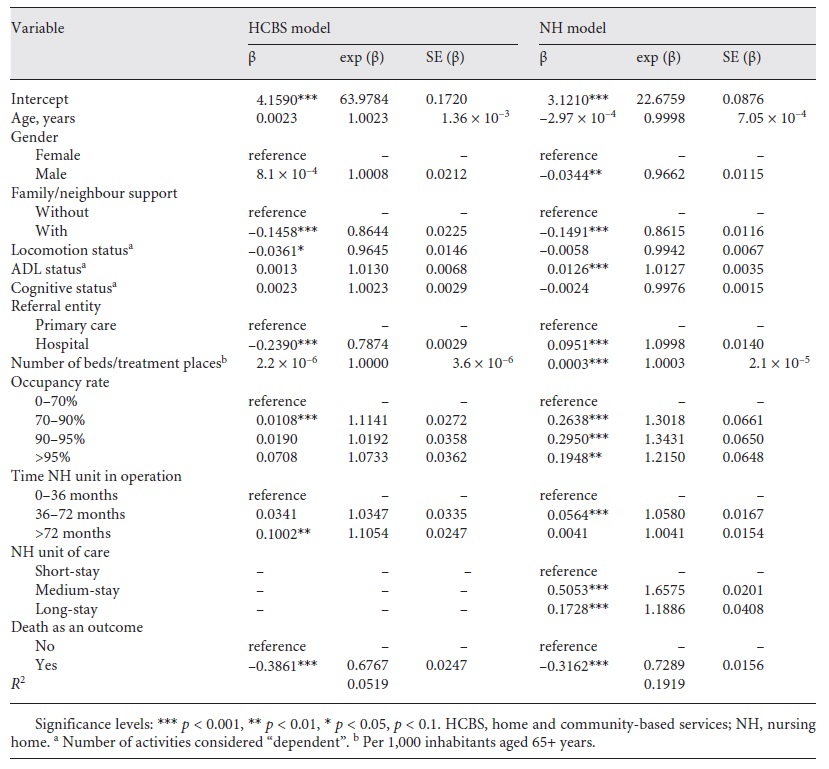
In a third step, to identify the main predictors of LOC, we used generalised linear models (GLM) with gamma distribution, considering the LOC as the dependent variable, the features described in Table 1 as explanatory variables, and logarithm link functions. We note that the gamma distribution accounts for the skewness of the density function of the LOC random variable (Fig. 3), as suggested by several authors [30, 31]. The results obtained for the GLM models are presented in Tables 4 and 5.
Table 4 Generalised linear models with gamma distribution and logarithm link function, with length of care as the dependent variable (variables observable at admission)
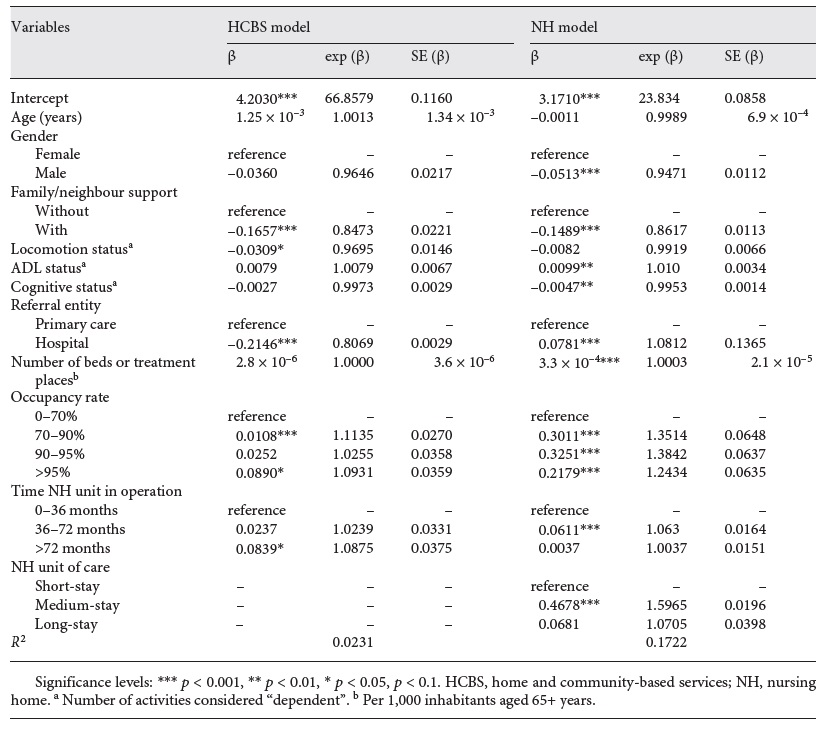
Table 5 Generalised linear models with gamma distribution and logarithmic link function, with length of care as the dependent variable (including death as an outcome)
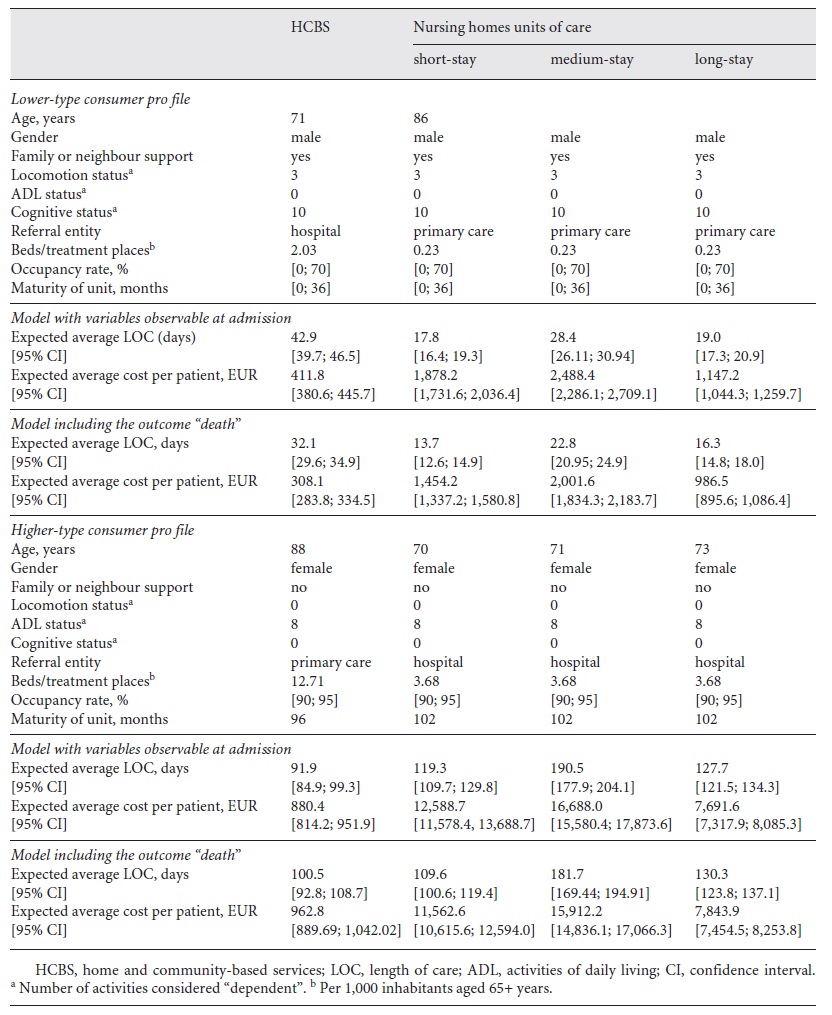
Based on the results from the GLM models, we were able to predict the LOC for each set of patients’ characteristics in each care setting. As an example, we identified the profile of a lower- and higher-type consumer of resources in each care setting, estimating the expected LOC for these patients and the associated costs (Table 6). For this estimate, we used the Portuguese national tariff for each setting, based on the per diem model (user/day) as a proxy for costs [32]: HCBS (EU 9.58), and Short-stay (EU 105.46), Medium-stay (EU 87.56), and Long-stay (EU 60.19) care units.
Table 6 Profiles of lower- and higher-type consumers of resources, their expected LOC, and costs for each type of care unit
All statistical analyses were performed using R software, and decisions based upon statistical tests reflect a significance level of p = 0.05.
Results
Patients’ Characteristics
Table 3 illustrates the patients’ characteristics observed in the database. The column “Total population” illustrates the measures obtained for the whole database. In the sections “HCBS” and “NH,” we highlight the differences between those receiving home care and those receiving institutionalised care. Finally, in the last section of the table, we illustrate the characteristics of the patients in each NH unit of care.
Although patients receiving home care and those receiving institutionalised care had a similar mean age, there are differences between the three institutionalised care settings, with the mean age increasing from a Short-stay to a Long-stay unit. Regarding gender, we note that, in all care settings, there is a larger percentage of women using the LTC services. As for family/neighbour support, although less than half of the patients have some social support, this percentage is higher among those receiving home care than among institutionalised individuals.
As for the dependency levels registered at admission, the average number of activities, in each area, in which a patient is considered “dependent” is higher in the institutionalised population than in those receiving home care and increases as one goes from a Short-stay to a Long-stay care unit, as expected.
Considering the referral entity, although most patients are referred by hospitals rather than by primary care teams, this difference decreases as we go from a Short-stay (88.5%) to a Long-stay unit (43.6%). Regarding the supply of care, the total number of NH beds per 1,000 inhabitants aged ≥65 years is lower than the home care treatment places, indicating a lower predominance of institutionalised care in the population under analysis. Regarding the maturity of each unit, although 18% have been in operation for <36 months, this increases to around 32% in Long-stay units. As for the occupancy rate, the lowest rate occurs in HCBS (mean 77%) and the highest in the Long-stay units (mean 95%). Although the overall mortality rate stood at 21%, one third of those receiving home care died during the period of this study. Nevertheless, regardless the setting of care, the mortality rate is higher in men than in women. Finally, whereas the overall mean LOC is 58 days, it is longer for those receiving home care than for those in the NH setting.
Average LOC of several variables of interest
Figures 1 and 2 illustrate the LOC for the HCBS and NH populations, with regard to several sociodemographic characteristics (age, gender, and family or neighbour support), dependency levels at admission (locomotion, ADL, and cognitive status), region, referral entity, care supply, and maturity of the unit and its rate of occupancy.
Regarding the sociodemographic characteristics, results show a similar trend in both populations. As for age, although more evident in HCBS population, as patients get older, their LOC also tend to increase. For gender, the average LOC is longer for women than men. Finally, the results show that those with less social support tend to have a longer LOC in both HCBS and the NH setting.
As for the dependency levels, although in NH the average LOC tends to increase as the number of physical and cognitive activities considered as “dependent” increases, this relationship does not seem to exist in HCBS.
Finally, as for the external factors of patients’ characteristics, several conclusions can be highlighted. First, patients referred by primary care present, on average, with a longer LOC than those referred by hospitals. Second, when patients receive care in regions with a greater availability of beds/treatment places, the average LOC is shorter than in regions with fewer places. It appears that, in HCBS, as the maturity of a unit (measured in number of months since its creation) increases, the average LOC also increases; in NH, this trend does not seem to be so evident.
We evaluated the predictors of a patient’s LOC in two different models: (i) considering only the observable characteristics at the time of admission and, (ii) including the outcome death. Figure 4 illustrates the relation between the LOC and the outcome death while a patient is using the LTC services.
Predictors of patients’ LOC
Table 4 presents the GLM estimates for LOC for both the HCBS and NH models by considering the variables observable at admission.
Considering the sociodemographic features, results show that, male gender and having some kind of social support are statistically significant factors for a shorter LOC, regardless of the setting of care. No statistical significance was found regarding individuals’ age.
As for the influence of the dependency levels at admission, only locomotion is statistically significant in the HCBS model. In this case, as the number of activities considered “dependent” increases, the LOC tends to decrease. As for the NH model, both ADL and cognitive status are statistically significant; as the number of ADL considered “dependent” increases, the LOC also increases, but the influence of cognitive status displays an opposite trend.
Finally, regarding the external factors, while in institutionalised care (NH), patients referred by hospitals have, on average, longer LOC than those referred by primary care; in HCBS, this effect is the opposite. As for the occupancy rate, results show a similar trend in both models. In this case, the average LOC of HCBS and NH units with occupancy rates >95% is 1.09 and 1.24 times longer than in units with a rate ≤70%, respectively. When compared to units that have been operating for <36 months, LOC in HCBS operating for >72 months is 1.08 times longer, and LOC in NH operating for 36-72 months is 1.06 times longer. Finally, when considering the NH settings of care, Medium-stay units display (on average) a 1.59 times longer LOC than Short-stay units.
To better understand the phenomenon of LOC in the Portuguese LTC system, we calculated the GLM estimates including the outcome, death (Table 5). Thus, when death (yes/no) is included as an explanatory variable, results differ from the previous results for both models (Table 4), particularly in HCBS. In this setting of care, the new results show that as patients’ age increases, the average LOC also tends to increase. Gender, on the other hand, is no longer has a significant influence. As for the dependency levels, the ability to perform ADL becomes an influencing factor. In this case, as the number of activities considered “dependent” increases, so the LOC tends to increase. As for the cognitive status, despite not being statistically significant, it follows the same trend as ADL, despite having the opposite influence in the previous model. Finally, regarding the variable, death, results show a shorter LOC for patients who end up dying in LTC units, regardless of the care setting.
Estimates of LOC for higher-type consumers of resources
After identifying the variables with the greatest influence on LOC (Table 4), we were able to estimate the expected LOC for a patient entering the Portuguese LTC system in each care setting. Table 6 presents the expected LOC and the total expected expenditure per patient, by including the characteristics of lower- and a higher-type consumers of resources when considering the factors observable at admission.
Although not all variables included in the model were statistically significant, we decided to include them in the estimates. With regard to age, we decided to consider the mean age of the population of each unit (Table 3), and then subtract/add the value of the standard deviation for obtaining a lower- and higher-type consumer, according to the impact on LOC (Table 4).
Regarding the profile of a lower/higher-type consumer, results show differences in the expected LOC and the respective average expenditure in each setting of care, when considering patients with similar characteristics. Concerning the profile of a lower-type consumer, although the average LOC of patients in HCBS is almost 2.5 and 1.5 times longer than that in the Short/Long-stay and Medium-stay NH units, respectively, the average cost per patient is 4.6/6.0 and 2.8 times lower, respectively. As for the higher-type consumer, patients receiving care in Medium-stay units are those with the longest expected LOC. In this case, the average LOC of these patients is 2.1 and 1.6/1.5 times longer than for those in HCBS and Short/Long-stay units, respectively, and the average cost per patient is 19.0 and 1.3/2.2 times higher, respectively.
Discussion
Considering the two main research questions of this work, we conclude that the most significant variables in predicting patients’ LOC at admission are gender, having family/neighbour support, the functional dependency level at admission, being referred by hospitals, and the setting of care to which patients are admitted.
Predictors of LOC
Regarding the sociodemographic characteristics, mixed evidence was found in the literature. Although old age and male gender are well-known factors associated with NH admission [19-21], their influence on LOC is not well proven [8, 12, 13, 15, 17]. In agreement with other studies [7, 8], we found that age is not a significant feature of a patient’s LOC. As for gender, our findings are also in line with other research found in the literature. Although it is not always a significant variable, when to be considered, males tend to present a shorter LOC [5, 13, 15], as in our study.
Regarding social support, the two main features that are commonly used to assess its influence on LOC are living arrangements [14, 16] and marital status [5, 11, 17]. Although further investigation is needed on this, our conclusion is in line with several other studies, i.e., a low level of social support is associated with longer periods of care [5, 11, 16].
Concerning previous findings, there may be two reasons for the role of age, gender, and social support in contributing to a shorter expected periods of care in the LTC system. Since there is both a longer life expectancy and a greater prevalence of physical and mental health comorbidity among females [1, 33], the absence or the death of a spouse may result in the provision of care for longer periods for women than for men. Moreover, since these features are also well-known risk factors for mortality in the LTC setting (see [26] for the Portuguese real-world situation and [17, 18] for other populations), the shorter expected LOC may be a consequence of a higher mortality rate among the individuals with such characteristics, as also referred by Häcker and Hackmann [13].
Given the overall regional asymmetries in the distribution of LTC resources, Portugal being no exception [25], much research has been done into the relationship between the supply side factors and LOC [5, 12, 15]. In our study, we observed that an increase in the number of beds/treatment places (per 1,000 inhabitants aged ≥65 years) had a residual effect on the average LOC in each care setting, although it was only statistically significant in NH. This may imply that increasing LTC resources can reduce waiting-lists and enable more individuals to have access to care, but not necessarily influence the LOC.
As for the referral entity, this is the first study to assess its influence on LOC. Although we found that patients referred by hospitals end up staying longer in the NH setting, results showed the opposite for HCBS. Despite further investigation being needed to compare these findings, a possible explanation may be related to differences between the multi-morbidity of patients referred by hospitals and primary care [2]. Regarding the setting of care to which patients are admitted, a study from Norway [8] reached a similar conclusion; the authors concluded that nearly 24% of total variation in care provision can be attributed to structure features of supply such as the number of NH beds, ownership, and average case mix. On the other hand, although we concluded that (on average) LOC is shortest in Short-stay units, followed by that in Long-stay units which is, in turn, shorter than in Medium-stay units, this may be influenced by the higher mortality rate in Long-stay units, which a recent Portuguese study found to be 30% [25].
Furthermore, to our knowledge, this is the first work to study the influence of occupancy rate and maturity of NH units on patients’ LOC in the LTC system. The fact that HCBS and NH units with low occupancy rate and those with <36 months of activity have, on average, a shorter LOC, should be considered by policy-makers when planning the provision of care and the allocation of resources. Nevertheless, further investigation is needed to assess the real impact of these variables on patients’ LOC.
The influence of patients’ dependency levels on LOC
The relationship between patients’ dependency levels and their LOC is well studied. Several studies [2, 8, 11, 13, 16] found that functional disability is a stronger predictor for the use of resources, especially in patients with ≥3 limitations when performing ADL or who are cognitively impaired [14]. In this case, although some authors have concluded that a higher level of dependency at admission is associated with a shorter LOC [11, 13], others have found that individuals who are more functionally and cognitively impaired have a longer LOC [14, 16]. We drew two main conclusions both settings of care: (i) Considering functional status, we observed a positive correlation with the number of ADL considered dependent (on admission) and the average LOC, but an opposite trend was observed for locomotion status; (ii) Regarding cognitive status, although the LOC tended to decrease with the number of activities considered “dependent,” it was only statistically significant for NH.
Regarding the functional status, considering that the Portuguese LTC system was created to restore (totally or partially) individuals’ lost autonomy in performing ADL, the fact that patients with more limitations at admission present a higher LOC may indicate a longer recovery time, as already suggested in previous investigations [34-36]. As for the influence of cognitive status, although some studies concluded that those with a higher level of impairment usually present a longer LOC [14, 16], we were not able to reach a significant conclusion. Since some patients need permanent care, given their higher level of disability, a shorter LOC in the LTC care setting may be a consequence of the transitions between different settings of care, or between publicly and privately funded care settings [4, 15]. To better study the patients’ pathways in the LTC system, it is vital to have information about transitions between different care settings, so that staff and policy-makers can plan the delivery of care delivery more accurately according to patient needs, both in terms of intensity and LOC.
Despite the importance of these findings for policy-makers, several limitations should be pointed out. There is no information regarding individuals who, although in need of LTC, were not admitted in any setting of care. Although there is insufficient evidence of the effectiveness of rehabilitation in LTC settings [34-36], the influence of patients’ functional/cognitive outcomes on their LOC was not considered. Moreover, as noted in a study conducted in the UK [15], since our study is restricted to publicly funded care, the lack of information about transfers between publicly and privately funded care means that it does not reflect the total LOC for all patients. Finally, other variables identified as significant by other authors, all of which can influence LOC, were not available, e.g., the ability to perform instrumental ADL [8], transitions between settings of care [4, 15], staff mix [6, 9, 10], and medical conditions [2, 12, 17, 18]. Further research is required to explore the influence of these and/or other variables.
Conclusion
The differences between the health and social support policies adopted by each country make it difficult to establish parameters by which international comparisons can be made, whether in terms of concepts, or organisational and financing models, but especially the assessment of the quality of care.
In this study, we show that LOC in the official Portuguese LTC system is highly influenced by the setting of care to which patients are admitted, which, in turn, follows the guidelines according to the expected LOC for each unit. Nevertheless, since almost one-third of patients discharged from Long-stay units received care within the maximum expected LOC for the other two NH units (30 and 90 days, respectively), this could indicate that, since the waiting list for LTC admission is high, the Long-stay unit, given the greater amount of care it supplies when compared with the other two NH settings (Table 2), is being used to accommodate patients with different care needs.
As the units of care are paid per day per patient, it is vital that policy-makers implement a monitoring system that assesses the relationship between LOC, patients’ care needs at admission, and patients’ outcomes. This measure would prevent the maximum expenditure due to (possibly inappropriate) prolonged stays, ensure a faster turnover of beds and a reduction of the numbers on the waiting list, and guarantee that patients are placed in the most suitable unit for their care needs.
Finally, as LOC usually determines turnover, but robust data has rarely been available, our findings should be considered when estimating the future demand for LTC services. Thus, it is essential to implement a quality control system to identify individuals’ dependency levels, redefine the information gathered by the Portuguese LTC monitoring system to incorporate other variables of interest such as staff skill mix, intensity of care provided, and patients’ comorbidities, as well as adopt a classification system for patients in LTC. Such measures are essential if we are to identify the needs of the population accurately, define risk stratification models, and assess the performance of care providers (particularly regarding the relationship between patients’ LOC and outcomes), and help bring about a more equitable allocation of funding resources.
Acknowledgement
G.G. and M.E. acknowledge the support of the Portuguese Foundation for Science and Technology through the project UID/MAT/00297/2019.
Author Contributions
H.L. conceived the original idea, collected the data, and took the lead in writing the manuscript. G.G. and M.E. developed the analytical framework and G.G. was responsible for the statistical analysis. C.M. supervised the study. All authors provided critical feedback and contributed to the final manuscript.