Introduction
Primary liver sarcoma is a rare diagnosis, accounting for less than 1% of primary malignancies of the liver [1]. According to some studies angiosarcoma, leiomyosarcoma, and epithelioid hemangioendothelioma are the most prevalent primary liver sarcomas [2]. While occurring predominantly in children from 6 to 10 years of age, ESL is a rarer entity that can also affect adults as some have reported [3]. ESL is a malignant neoplasm with an aggressive course, but its treatment and prognosis may be more optimistic than was previously thought. In this paper, we describe a case of a 43-year-old female with a diagnosis of ESL.
Case Report
A Portuguese woman of 43 years of age resident in Southeast Asia presented to her local hospital emergency room with complaints of asthenia, abdominal bloating, anorexia, and nocturnal sudoresis with 2 months evolution. A CT-scan showed a 19 × 14 cm mass ranging from the epigastrium to the left hypochondrial region with centripetal peripheral hypervascularization suggesting the presence of necrosis or a cystic component. The origin of the mass was not evident. It seemed to encompass part of the liver, and it was attached to the diaphragm and spleen. Back in Portugal, the clinical presentation was unaltered, and the physical examination identified diffuse abdominal pain during palpation with objectified hepatomegaly and a homogeneous epigastric mass. The bowel movements were maintained, the aspect of faeces and urine unchanged and there was no jaundice. The blood work-up showed upper borderline levels of alkaline phosphatase and gamma-glutamyl transferase (187 U/L and 54 U/L), a considerable rise of C-reactive protein (16.04 mg/dL) and a slight rise of prothrombin time (14.5 s) as the only abnormal values. Alpha-fetoprotein, CA 19.9, and carcinoembryonic antigen were within normal ranges.
The images were reviewed with identical findings and the radiological diagnostic hypothesis were of gastrointestinal stromal tumour (GIST), angiosarcoma, or a neurogenic lesion. An ultrasound-guided biopsy of the mass was then performed. Stained slides were observed in light microscope - Nikon Eclipse 50i, and images were obtained using a Nikon-Digital Sight DS-Fi1 camera.
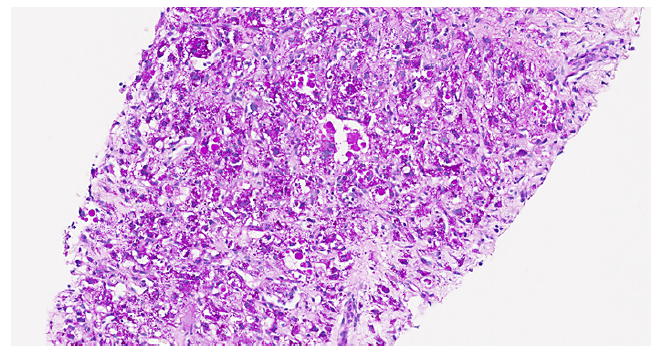
The collected material consisted of two biopsy cylinders in total with 18 mm width, showing hepatic tissue with normal architecture and signs of compression in relation to the presence of an adjacent space-occupying lesion. The lesion was well demarked from the liver tissue by a fine connective tissue band and was composed by a highly variable cell population (shown in Fig. 1), exhibiting multinucleated giant cells with enlarged irregular hyperchromatic nuclei, eosinophilic clear cytoplasm with fading limits. There were PAS-positive hyaline globules (shown in Fig. 2, 3), and other smaller cells with epithelioid, stellated, or spindled configuration, supported by a myxoid richly vascularized stroma. No mitotic activity was detected.
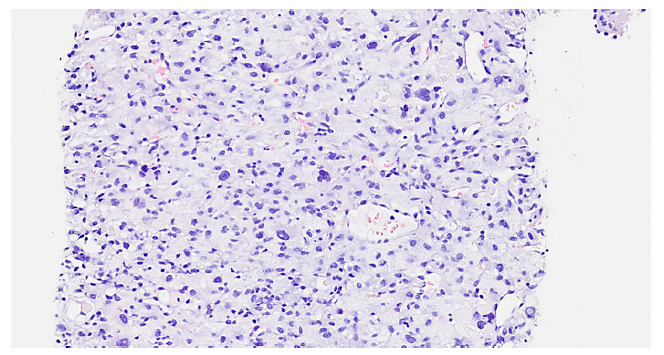
Fig. 1 Lesion with severely pleomorphic cell population (haematoxylineosin, original magnification, ×200).
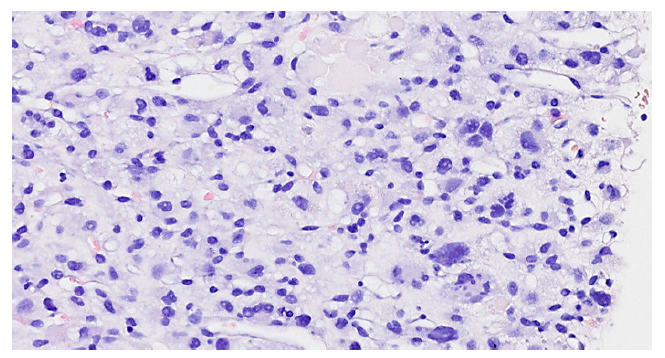
Fig. 2 Multinucleated giant cells with hyaline globules are a key feature of ESL (haematoxylineosin, original magnification, ×400).
Several immunochemical panels were sequentially performed. The tumour cells were positive for vimentin, CD10, glypican-3, and α1-antitrypsin, with the latter two especially positive in the giant cells. They showed no expression of MNF-116, EMA, HepPar1, LCA, CD31, CD34, ERG, HMB45, S100, SOX10, CD117, DOG1, smooth muscle actin, desmin, MDM2, CD23, and AFP.
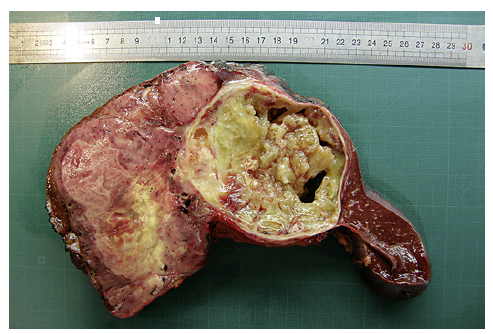
The conjugation of H&E morphology and ancillary studies was consistent with the diagnosis of ESL. The case was discussed by a multidisciplinary team that attested to the conditions for the tumour resection. The patient underwent left hepatic lobectomy with splenectomy and partial resection of the diaphragm. Upon gross examination of the main specimen, there was a 22 × 17 × 8 cm bilobate mass with a solid component stemming from the left hepatic lobe and a cystic component adherent through a fibrous pseudocapsule to the spleen (shown in Fig. 4). The microscopic examination of the surgical specimen showed once again stellated and spindled cells amongst multinucleated giant cells with hyaline globules. The cells were positive for vimentin, CD10, glypican-3, and α1-antitrypsin and negative for desmin, EMA, HepPar1, CD34, CD117, and S100, overlapping with the biopsy findings. The diaphragm showed involvement by the neoplasia.
Fifteen days after the surgery, the patient presented to the emergency room with a fever. Analytic studies revealed leucocytosis, thrombocytosis, and a rise of C-reactive protein (12.2 mg/dL). Thoracic and abdominal ultrasound exhibited pleural effusion and a liquid anechoic collection with 12 cm between the liver and the stomach suggestive of biloma. The pleural effusion was drained and sent for cytological examination that showed no tumour cells. The patient was treated with ceftriaxone and discharged after 5 days.
Almost 4 months after the primary diagnosis and 2 months after the surgery, a CT-scan showed a 0.7 cm nodule in segment 7 of the liver. The lesion was hypervascular during the arterial phase and, subsequently isodense suggestive of metastasis. The patient underwent segmental hepatectomy during which a peritoneal perigastric nodule was found and submitted for intraoperative pathological examination that attested to its neoplastic nature. The post-surgery histological study confirmed the metastatic essence of the two nodules. The patient recovered from the surgery without further issues.
Two months after the second surgery and 7 months after the primary diagnosis a follow-up, CT-scan detected a solid, vascularized nodule in the inferior lobe of the left lung. The patient is currently undergoing her second month of chemotherapy.
Discussion
ESL is a malignant mesenchymal tumour with predominance in children, with rare cases described in adults. This entity does not have a particular clinical or radiological presentation. Patients usually have no laboratory disturbances but may have leucocytosis or high serum alkaline phosphatase, while elevated tumour markers are rare. In this case, the patient had elevated alkaline phosphatase, gammaglutamyl transferase and reactive C protein while the tumour markers are within normal ranges. The radiologic findings are nonspecific, showing most of the time a large and complex intraperitoneal mass usually with cystic degeneration. This cystic component is not uncommonly misdiagnosed as a benign lesion [4, 5]. In fact, the radiologic re-evaluation of our patient is reported as suggestive of a liver haemangioma. The gross presentation of this entity consists of a pseudocapsulated mass usually larger than 10 cm; it has severe heterogeneity on cut surface with solid and mucilaginous cystic components with haemorrhage and necrosis, being coincident with what we observed in the surgical specimen.
Histological analysis of ESL usually displays an array of pleomorphic cells supported by a myxoid stroma. While these cells include stellate and spindled shapes, multinucleated giant cells with cytoplasmic PAS-positive eosinophilic hyaline globules are the most distinctive histological feature of ESL. A very frequent facet that is not consonant with our analysis is the mitosis sum [3]. Although mitosis is frequently described in the medical literature, we only identified 1 mitosis/11.85 mm2 and when using Ki67 stain less than 10% of the neoplastic cells were stained. Regarding the fact that the diagnosis was made in a biopsy sample, one might conjecture that there may be areas with different proliferation rates. On the other hand, as we obtained the same results in the surgical specimen, the existence of a subset of ESL with lower proliferation and therefore better prognosis can be hypothesized.
No specific immunophenotype of ESL is known but several reports denote positivity in most cases for vimentin, α1-antitrypsin, CD68, CD10 and, in a subset of tumours, glypican-3. Other stains that show variable results include desmin, keratins, and muscle specificactin, and we should be on the lookout for pitfall diagnosis that this expression might suggest. Tumour cells are negative for EMA, HepPar1, AFP, myogenin, MYOD1, CD34, CD117, ALK-1, and S100 [3, 4]. Our immunochemistry results are concordant as neoplastic cells show positivity for vimentin, CD10, glypican-3, and α1-antitrypsin and are negative for EMA, HepPar1, AFP, CD34, CD117, and S100.
An extended immunochemistry study is designed to guide us regarding the differential diagnosis of ESL, which in adult patients include angiomyolipoma, epithelioid haemangioendothelioma, high-grade sarcomas, GIST, malignant melanoma, and HCC. Angiomyolipoma is predominant in female middle-aged adults, and its gross presentation is variable; histologic features include epithelioid cells, spindled cells in some cases, and pleomorphic cells are not uncommon [6]. Adipocytes and thick-walled vessels, other characteristic findings, were not found in our case. The hypothesis of epithelioid haemangioendothelioma is supported by the age and sex of our patient, as it is more common in middle-aged women and by the microscopic features as they have spindled, stellated and even giant multinucleated cells, with rare mitosis. Its macroscopic presentation of a firm and white mass on the cut surface, however, is not assonant with our observation [6]. In spite of our findings not being exceptionally consistent with high-grade sarcomas, such as angiosarcoma, leiomyosarcoma, and liposarcoma, these diagnoses are also taken into account as they present as a large mass, sometimes having cystic degeneration (leiomyosarcoma), and histological elements include spindled and epithelioid cells with marked atypia [6-8]. Liposarcoma, especially, was considered as at the moment of the biopsy, since radiology cannot determine if the tumour had origin on the liver. GIST gross examination may present as a large mass with cystic degeneration and necrosis. Although it usually has little to no pleomorphism, epithelioid GISTs sometimes have a sarcomatous morphology [6]. Albeit extremely rare, malignant melanoma of the liver also presents as a large liver mass and microscopically reveals pleomorphic cells with spindled, round, and irregular morphology [9]. Malignant melanoma metastasis to the liver is a much more credible hypothesis but no history of cutaneous, ocular, or mucosal melanoma is present. HCC must simply be considered due to its prevalence, as it is by far the most frequent primary hepatic malignancy. In addition, its microscopic presentation encompasses a wide spectrum.
The tumour cells were negative for several markers, supporting the exclusion of differential diagnosis, namely CD117 and DOG1 (GIST), HMB45 and S100 protein (angiomyolipoma and melanoma), CD34 and CD31 (epithelioid haemangioendothelioma and angiosarcoma), MDM2 (liposarcoma), smooth muscle actin, and desmin (leiomyosarcoma). HepPar1 negativity is not enough to exclude hepatocellular carcinoma firstly because poorly differentiated HCC may lose HepPar1 expression and secondly because our case showed positivity for glypican-3. On the other hand, we have MNF-116 negativity and the histologic features are not concurring with that diagnosis.
There is not a well-defined treatment for ESL. However, hepatectomy seems to be a key part of it, as patients that do not undergo surgery - radical hepatectomy or hepatic lobectomy - have a significantly lower survival rate. Multimodal therapies such as neoadjuvant or postoperative chemotherapy or radiotherapy, paediatric age and negative surgical margins status have been reported to be favourable factors for both the survival rate and the disease-free survival of patients with ESL. While extrahepatic disease appears not to be a factor of major preponderance regarding prognosis, tumour size effect on survival is still uncertain. Wu and colleagues have reported a 65.8% 5-year survival rate for any treatment, featuring liver transplantation as the best therapeutic option [10, 11].
ESL is a rare sarcoma that while predominant in infancy ages must always be in the back of the pathologist’s mind when thinking of differential diagnosis for large, heterogeneous masses of the liver. PAS-positive hyaline globules within giant multinucleated cells are a characteristic histopathological key finding. Although proper immunophenotyping of this entity is lacking, the majority show positivity for vimentin, α1-antitrypsin, CD68, CD10, and glypican-3. Even when a case is concordant to ESL, other diagnoses must be rejected first. Currently, there are no fitting guidelines for the management of ESL but the multimodal treatment seems to attain decent results. Further studies must take place to fill in the knowledge gaps for more efficient diagnosis and therapy.