Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy is still a challenging procedure due to altered anatomy, even among experienced endoscopists. ERCP in patients with Billroth II gastrectomy is technically more demanding, with ERCP failures associated with afferent loop intubation, papilla identification, deep biliary cannulation in an inverted papilla, and performance of sphincterotomy [1-4]. Moreover, it presents more risks than ERCP performed in patients with normal anatomy, with perforation rates of up to 2.8% [1].
Different endoscopes may be used, including side-viewing duodenoscope, forward-viewing gastroscope (with or without cap-fitting) [4, 5], balloon-assisted enteroscope [6, 7], colonoscope [8], and anterior oblique-viewing endoscope [9]. While papilla identification and cannulation are thought to be easier with side-viewing duodenoscope; afferent loop intubation and reaching the papilla are easier with forward-viewing gastroscope with lower risk of perforation [1, 4, 10]. Regarding cannulation, different cannulation techniques have been described: standard cannulas, conventional sphincterotome [3, 8, 11], needle-knife [8, 11], and rotatable or dedicated inverted sphincterotome [11, 12]. However, the optimal approach, namely the type of endoscope and sphincter management, has yet to be defined. Indeed, comparative studies are scarce [10, 11] and the majority of the studies published are retrospective, without prospective databases, and single arm [1, 3, 4, 7, 12].
Therefore, we aim to compare the efficacy and safety, as well as their determinants, of performing ERCP using forward-viewing gastroscope versus duodenoscope in patients with Billroth II gastrectomy.
Methods
Study Design, Setting, and Selection of Participants
We conducted a retrospective, single-center cohort study including all consecutive patients with Billroth II gastrectomy and native papilla submitted to ERCP between January 2005 and March 2021 at Hospital Santa Luzia, ULSAM, Viana do Castelo, Portugal; a hospital affiliated with the School of Medicine, University of Minho, a referral center for advanced biliopancreatic endos-copy. We included only ERCP for management of biliary disease.
ERCP Procedures
Written informed consent was obtained from all patients. ERCPs were performed by two experienced endoscopists (L.L. and J.R.) who each performed ≥300 ERCPs annually for the past 15 years. All ERCPs were performed under deep sedation/general anesthesia with propofol (by an anesthesiologist). ERCP was always started with the patient in the prone position. If intubation of the afferent loop was not feasible, the patient was turned to left lateral decubitus, to facilitate entering the afferent loop. The afferent loop intubation was confirmed by the presence of bile and by the endoscope position on fluoroscopy. The afferent loop was intubated with minimal air/CO2 insufflation, and most papillae were located at the 10- or 11-o’clock position. Deep cannulation was initially attempted using a standard straight catheter (Triple Lumen ERCP cannula, Tapered Tip 5.5 Fr; Boston Scientific, Natick, MA, USA), attempting to insert the catheter gently into the bile duct; if deep insertion was not feasible, after minimal insertion of the catheter in the ampulla (1-2 mm), the guidewire was carefully advanced into the common biliary duct (CBD) under fluoroscopy. Pushing the catheter against the duodenal wall at the 9- to 10-o’clock position or changing the position of the tip of the endoscope led the tipof the catheter to the correct access to the CBD. We used a 0.035-inch hydrophilic guide wire (Jagwire; Boston Scientific). If deep cannulation was not achieved, needle-knife fistulotomy (NKF) was performed as a second-line approach, using an Olympus KD-11Q, Olympus Corporation, Melville, NY, USA). After successful biliary cannulation, if sphincterotomy was indicated, a 5-cm plastic biliary stent was inserted, and an NKF was performed in the 5-o’clock direction over the plastic biliary stent placed along the bile duct. Once the ERCP was completed, all patients were admit-ted to the inpatient area of the hospital and observed for 24 h, before discharge. When deep cannulation of the bile duct was unsuccessful after NKF, a second ERCP was scheduled in less than a week.
All procedures were performed using a forward-viewing gastroscope or a duodenoscope (Olympus TJF 160 VR, GIF-Q165, GIF-1TH190; Olympus Corporation). Between 2005 and 2015 all ERCPs were performed exclusively with a side-viewing duodeno-scope. Taking into account new-evidence-based literature [13, 14] and practice experience, after 2015 all ERCP procedures were always performed using a forward-viewing gastroscope (Fig. 1). All ERCPs performed with a forward-viewing were initially attempted without a cap (Transparent cap Olympus D-201-11804); a cap was attached to the tip of the forward-viewing gastroscope only in cases where cannulation was unsuccessful. In case of failure with either duodenoscope (2005-2015) or gastroscope (2015-2021), there was no attempt to perform ERCP with another endoscope.
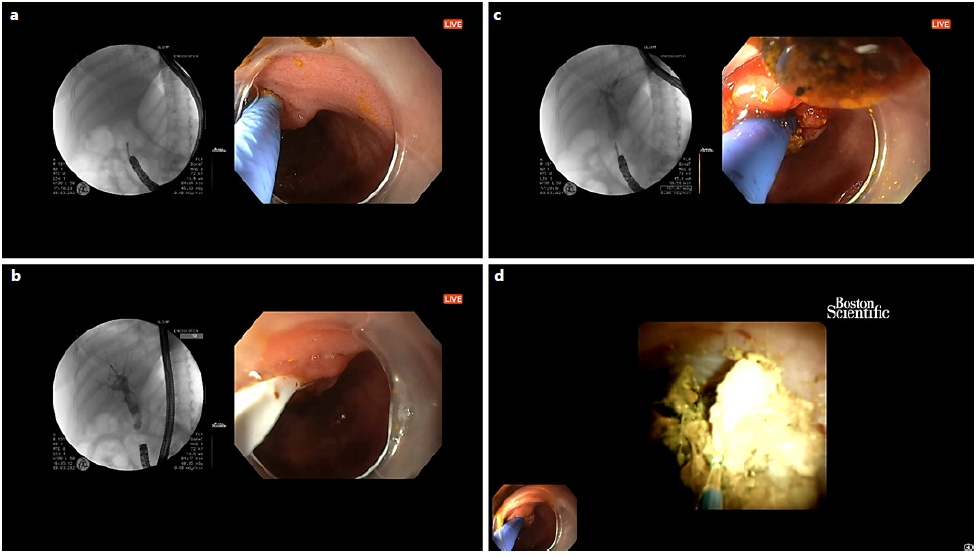
Fig. 1 Endoscopic retrograde cholangiopancreatography performed with a forward-viewing gastroscope with cap. a Cannulation. b Stone extraction. c Cholangiogram. d Cholangioscopy-guided laser lithotripsy.
Data Collection, Variables and Outcomes
Data was collected from a dedicated prospectively maintained database. Data on demographic variables, year of the procedure, ERCP indication and diagnosis, type of endoscope, biliary access technique, therapeutic interventions, complications and its man-agement were extracted from the database. The complications were reported by severity and time of occurrence (intra-procedural, early [within 14 days of follow-up] and late [after 14 days of follow-up]) according to ASGE lexicon’s severity grading system [15]. The two primary outcomes evaluated were: (1) success rate of papilla major identification and (2) deep biliary cannulation. The success rate of biliary cannulation is presented for all patients (intention-to-treat), as well as for the subgroup of patients in which the papilla major was identified. The secondary outcomes were: (3) rate of ERCP-related adverse events and (4) evaluation of reasons for not identifying the papilla major. The ERCP-related adverse events are presented for all patients (intention-to-treat) as well as for the subgroup of patients in which the papilla major was identified.
Statistical Analysis
Descriptive statistics included mean and standard deviation or median and interquartile range (IQR) for quantitative variables and proportions for categorical variables. The differences in base-line characteristics between the two endoscope groups was assessed using the Student t test for age and the χ2 test (with Bonferroni adjustment for multiple comparisons) for categorical variables. The association between endoscope and quantitative variables was analyzed using the t test or the corresponding non-parametric test. The association between endoscope and categorical variables was analyzed with the χ2 test (with Bonferroni adjustment for multiple comparisons). Multiple logistic regressions were performed to evaluate predictors of the main outcomes. In the multivariable regression model, we included variables that physiologically could be associated with the outcome or variables with a p value less than 0.25 in simple regression model. The 95% CIs were calculated and used to compare the results between endo-scope groups. A p value of <0.05 was considered statistically significant.
Results
Patient Characteristics and ERCP Indications
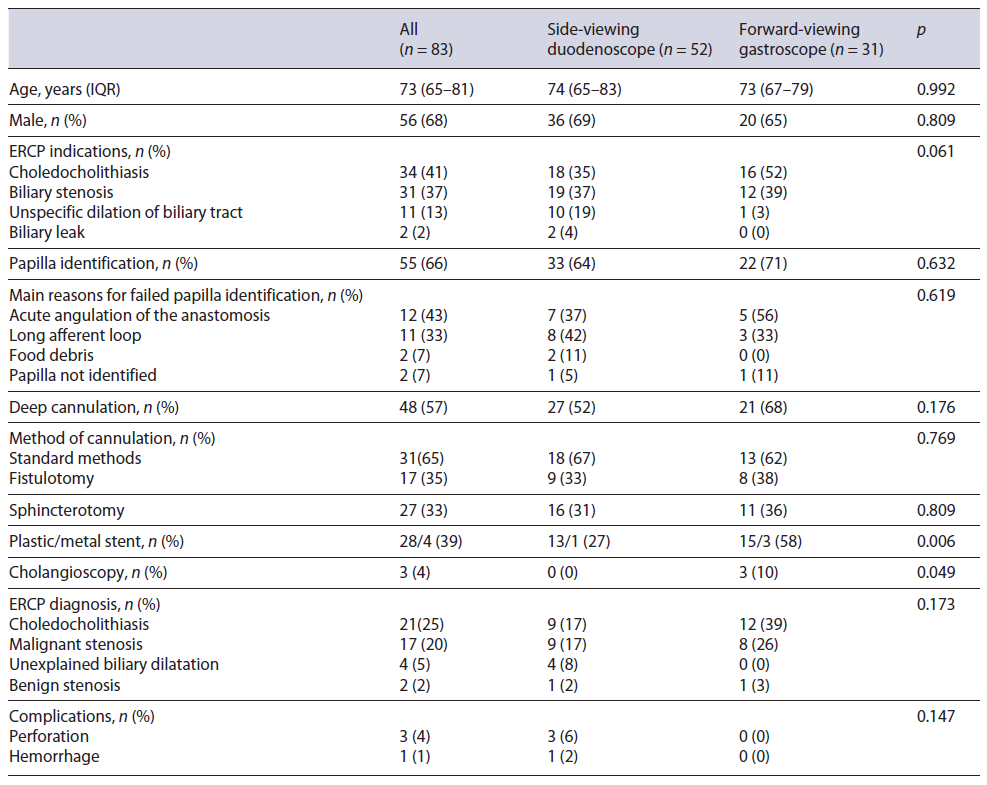
We included 83 patients with a median age of 73 (IQR 65-81) years; 68% of them were male. The main indications for ERCP were choledocholithiasis (41%), biliary stenosis (37%), unspecific dilation of biliary tract (13%), and biliary leak (2%). ERCP was performed using a side-viewing duodenoscope in 52 patients and a forward-viewing therapeutic gastroscope in 31 patients. There were no differences between endoscope groups regarding patient characteristics (duodenoscope vs. gastroscope: age, 74 [IQR 65-83] vs. 73 [IQR 67-79] years, p = 0.992; male, 69 vs. 65%, p = 0.809) (Table 1).
Primary Outcomes
Access to the papilla was achieved in 66% of patients (n = 55), of which 93% (n = 51) in the first ERCP. The rate of deep cannulation was 58% (48/83) in all patients (intention-to-treat analysis) and 87% (48/55) in the sub-group of patients in which the papilla major was identified, with 88% (n = 42) cannulated at the first ERCP. Cannulation was achieved using standard methods in 65% (n = 31) of cases (with sphincterotomy performed in 27 patients) or with NKF in 35% (n = 17) of cases. Cholangioscopy with the Spyglass system was performed in 3 cases, of which 2 underwent cholangioscopy-guided laser lithotripsy. Of the patients that underwent papilla cannulation, a biliary stent was inserted after cannulation in 66% (n = 32) when indicated (plastic stent in 28 and metallic stent in 4) (Table 1).
There was no difference between side-viewing duodenoscope and forward-viewing gastroscope in papilla identification rate (64% [95% CI: 51-77] vs. 71% [55-87], p = 0.632). Although not statistically significant, side-viewing duodenoscope had a lower deep cannulation rate than forward-viewing gastroscope when considering all patients (52% [15-39] vs. 68% [7-35], p = 0.176) and when considering only the subgroup of patients in which the papilla major was identified (82% [72-92] vs. 95% [89-100], p = 0.223).
Secondary Outcomes
Adverse events occurred in 4 patients: 3 perforations in the anastomosis (all intra-procedural and severe) and 1 hemorrhage (intra-procedural and moderate) (Table 1).
When considering all patients, duodenoscope had a higher adverse events rate (8% [1-15] vs. 0% [0-0.5], p = 0.147) namely perforation (p = 1.0) and hemorrhage rate (p = 1.0), though not statistically significant. Likewise, when considering only the subgroup of patients in which the papilla major was identified and biliary cannulation attempted, duodenoscope had a higher adverse events rate (9% [0-18] vs. 0% [0-1], p = 0.208), though not statistically significant.
There was failure to identify the papilla in 34% of cases (n = 28) due to (i) acute angulation of the anastomosis in 43% (n = 12); (ii) long afferent loop in 39% (n = 11) of cases; (iii) food debris in 7% (n = 2); (iv) papilla not identified despite afferent loop exploration in 7% (n = 2); and (v) anesthesia-related complication in 4% of cases (n = 1).
Multiple Logistic Regression
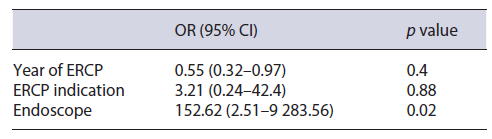
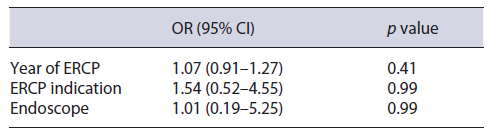
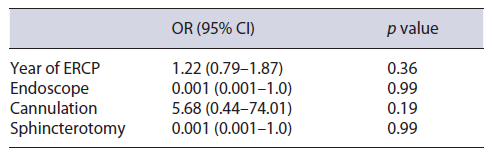
There was no significant time trend regarding papilla identification (p = 0.256), deep cannulation (p = 0.779) and adverse events (p = 0.962). In a univariate analysis, there was no significant interaction between time of ERCP and type of endoscope used regarding papilla identification (p = 0.763), deep cannulation (p = 0.16) and adverse events (p = 0.763). In a multivariate analysis, the use of gastroscope significantly increased the cannulation rate [OR = 152.62 (95% CI = 2.5-9,283.6), p = 0.02] when controlling for year of ERCP and ERCP indication (Table 2). However, the type of endoscope was not associated with papilla identification or with risk of perforation (Tables 3, 4).
Discussion
ERCP in patients with Billroth II gastrectomy has various challenges that have to be overcome. Firstly, recognition and intubation of the afferent loop, sometimes hampered by acute angulation of the anastomosis. Then, progression on the afferent loop and papilla identification can also be hampered because of angulations, adhesions or long afferent loop. After reaching the papilla, cannulation maneuvers have to be adapted to the inverted position of the endoscope. Therefore, ERCP in patients with Billroth II gastrectomy is still a challenging procedure [2, 16].
Although the side-viewing duodenoscope is the most commonly used endoscope for ERCP in Billroth II gastrectomy patients, forward-viewing gastroscope has been increasingly used. However, each endoscope has its advantages and drawbacks. While papilla identification and cannulation are thought to be easier with side-viewing duodenoscope due to its elevator and large working channel; afferent loop intubation and reaching the papilla are easier with forward-viewing gastroscope with consequently lower risk of perforation [1, 2, 4, 10]. Although the choice of endoscope has been a matter of controversy, there is still lack of comparative studies regarding ERCP in patients with Billroth II gastrectomy. Indeed, Park and Song [1] conducted a recent systematic review showing that there is only 1 retrospective and 1 prospective comparative study about the choice of endoscope [10, 17]. Besides these two comparative studies, 3 retrospective cohorts have been published reporting the use of forward- and side-viewing endoscope in ERCP in patients with Billroth II gastrectomy [3, 8, 18]. In this systematic review, the overall rate of papilla cannulation was 87.9%, and the overall rate of adverse events rate was 7.3%. When analyzed by endoscope, the success rate of papilla cannulation was 95.3% for side-viewing endoscope and 95.2% for forward-viewing endoscope. Moreover, the authors demonstrated that the rate of perforation was slightly higher in side-viewing endoscope (3.6%) compared with forward-viewing endoscope (1.7%) [1]. Likewise, we found that the use of forward-viewing gastroscope significantly increased the deep cannulation rate in a multi-variate analysis. Although the type of endoscope was not associated with the risk of perforation in a multivariate analysis, the risk of perforation was higher with side-viewing duodenoscope (6%) compared with forward-viewing gastroscope (0%). Recently, Nennstiel et al. [19] published the daily clinical management of patients with altered anatomy and the need of biliary intervention in four tertiary endoscopic centers in Munich. In 33 patients with Billroth II that underwent ERCP with gastroscope, the success rate (defined as reaching the papilla with successful cannulation) was 79%, with 71% of cases with unsuccessful papilla identification and 29% with unsuccessful papilla cannulation. In 72 patients with Billroth II that underwent ERCP with duodenoscope, the success rate was 86%, with 50% of cases with unsuccessful papilla identification and 50% with unsuccessful papilla cannulation [19].
In our study, the favorable results of forward-viewing gastroscope in comparison to the side-viewing duodenoscope can result from the fact that we used a therapeutic gastroscope with an extra-large channel associated sometimes with a transparent cap fitted to the distal end, facilitating not only afferent loop intubation and progression due to its flexibility and good visual field, but also deep cannulation due to its large working channel and use of cap. Recently, two retrospective cohorts of 18 and 46 patients with Billroth II gastrectomy that underwent ERCP using therapeutic double-channel gastroscope reported afferent loop intubation of 83% and papilla cannulation of 100% [20, 21].
This study has some limitations. It is a single-center retrospective cohort with no randomized allocation of the type of endoscope which can lead to bias. Another pos-sible limitation is the sample size, which can influence the effect size, especially in the subgroup analysis. Indeed, the non-statistically significant lower adverse events rate with the forward-viewing gastroscope may traduce the small sample size. However, the majority of the studies published to date have smaller sample sizes [7, 8, 10, 11, 19-21]. Moreover, this study was performed in a tertiary referral center with expertise in ERCP, which could have positively impacted the results, stressing the need to referthese patients to expert centers. In our study, before 2015, all ERCPs were performed with a side-viewing duodenoscope and after 2015, all ERCP were performed with a forward-viewing gastroscope. This change of type of endoscope in 2015 resulted from a discretionary decision of the endoscopy team and evidence-based literature [13] in order to improve the safety of the intubation of the afferent limb. Therefore, we conducted a multivariate analysis that excluded any significant impact of time on papilla identification, deep cannulation, or adverse events suggesting that the favorable results of forward-viewing gastroscope were not due to experience of the endoscopist but rather due to the type of endoscope used.
Besides the side-viewing duodenoscope and forward-viewing gastroscope (with or without cap-fitting), other endoscopes and techniques have been studied in surgically altered anatomy according to centers experience and technique availability, namely balloon-assisted enteroscope [6, 7], colonoscope [8], anterior oblique-viewing endoscope [9], endoscopic ultrasonography-guided transhepatic antegrade interventions [22], and underwater cap-assisted ERCP [23]. Future comparative studies are warranted.
Although Billroth II anatomy will become less frequent, we will encounter these patients in our endoscopic practice, and we will have to face the challenges to safely and successfully perform ERCP [2]. Current data and this study demonstrate that therapeutic forward-viewing gastroscope with capfitting, when necessary, is at least as effective and as safe as side-viewing duodenoscope for ERCP in patients with Billroth II gastrectomy. However, future multi-center randomized trials with large sample size are needed to validate these results and to define the optimal endoscopic approach.