Introduction
Ultrasound-guided fine-needle aspiration (EUS-FNA) is considered the diagnostic standard for malignant pancreatic tumors; however, its sensitivity and specificity are widely variable, ranging from 73 to 96.5% and from 71.4 to 100%, respectively [1]. Several factors can affect the outcome of EUS-FNA such as the needle caliber and design, application of suction, use of stylet, onsite cytopathological evaluation of specimens, number of passes, location and size of the tumor, and experience of the endosonographer. The main disadvantage of FNA is that the sampled tissue does not necessarily retain the cellular architecture of the stroma, which is critical for establishing the diagnosis. Recent developments in needle design have permitted the acquisition of core biopsies to overcome the limitations of FNA and preserve the cellular architecture, thereby improving diagnostic performance [2]. This new tissue acquisition technique is denominated fine-needle biopsy (FNB). Two recently introduced FNB needles include the reverse bevel needle Echotip ProCore® (Cook Medical Inc., Limerick, Ireland) and Franseen tip needle Acquire® (Boston Scientific Co., Natick, MA, USA). FNB needles have special relevance in oncology, as this technique of tissue acquisition allows molecular tumor profiling for targeted therapy and more frequent immunohistochemical staining than FNA needles [3, 4].
Randomized clinical controlled trials have revealed that the reverse bevel needle has a threefold better ability to obtain histological core samples and a higher diagnostic yield than the standard FNA needle (92 vs. 30%, p = 0.006, 20 vs. 75%, p = 0.010, respectively) [5, 6]. Although a systematic review and meta-analysis identified no difference in diagnostic accuracy between these two needles, the reverse bevel needle required fewer passes [7]. Moreover, the Franseen needle was linked to a diagnostic accuracy rate of 96%, versus 88% for the FNA standard needle, as well as a higher mean histology cell block score with fewer needle passes (2.88 vs. 3.82; p < 0.001) [8]. More recently, a randomized clinical trial compared a 22-gauge Franseen needle and 20-gauge reverse bevel needle, revealing higher diagnostic accuracy for the Franseen needle (87 vs. 67%; p = 0.02) [9]. However, the difficulty in using a higher-gauge needle may affect tissue sampling in certain endoscopic positions. Thus, the main objective of our study was to compare the diagnostic yield of two different FNB needles with the same caliber in the EUS-guided sampling of pancre-atic solid lesions.
Materials and Methods
This was a retrospective observational study in which we compared a cohort of patients with pancreatic solid lesions who underwent sampling using a 22-gauge FNB reverse bevel needle and a 22-gauge FNB Franseen needle between September 2016 and March 2020 at Instituto Nacional de Cancerologia in Mexico City, Mexico. This study was approved by the Instituto Nacional de Cancerologia Investigation Committee with the approval No. 2020/0115. Men and women ≥18 years old were eligible for enrollment. We excluded patients who met any of the following criteria: presence of cystic lesions, pregnancy, international normalized ratio >1.5, partial thromboplastin time >42 s, platelet count <50,000, surgically altered anatomy, anticoagulant treatment, hemodynamic instability, and less than 6 months of follow-up.
Patients were divided into two groups according to the FNB needle used for sampling. Clinical and demographics variables such as age, sex, tumor size and localization, number of needle passes, biopsy route, complications, tissue adequacy, and diagnostic yield were analyzed.
The quality of the tissue sample and diagnostic yield were reported by pathologists dedicated to pancreatobiliary pathology. Sample adequacy was defined as the presence of sufficient tissue to allow complete histological evaluation.
Tissue samples submitted for cytopathological analysis were interpreted using the criteria established by the Papanicolaou Society System for pancreatobiliary cytopathology classification as follows: category I (nondiagnostic), category II (negative for malignancy), category III (atypical), category IV (benign neoplastic, other neoplastic), category V (suspicious for malignancy), and category VI (positive for malignancy) [10]. Tissue samples submitted for histopathological analysis were interpreted by surgical pathologists. Pathologists were blinded to the type of needle used.
EUS Tissue Sampling Technique
All procedures were performed under intravenous sedation using a combination of propofol and fentanyl. An Olympus Linear Echo-endoscope (Olympus GF-UCT180, Tokyo, Japan) was used with an EU-2 Premier and EU-2 Premier-Plus processor. All procedures were performed by two expert endosonographers who had performed >1,000 studies.
Once the lesion was identified under ultrasonographic examination, it was punctured using an FNB needle with stylet. After puncture, the stylet was removed, and 5 mL of suction was applied. Sampling was performed using the fanning technique, and each pass con-sisted of 10-15 back-and-forth movements. Once the pass was completed, the needle was removed for tissue preparation. Considering previous studies that found no benefit in diagnostic yield after taking more than two passes, a goal of two passes was considered the standard, and additional passes were performed at the discretion of the endoscopist after visual inspection of the obtained tissue.
Tissue Processing
Once the needle was removed, a smear was extended on glass slides, dried in air, and then preserved using Hemacolor® stain (Merck KGaA, Darmstadt, Germany). A second smear was then extended on a glass slide, immediately immersed in 96% ethyl alcohol, fixed for at least 10 min, and dyed with the Pap smear technique using the integrated Tissue-Tek Prisma® platform (Sakura Finetek USA Inc., Torrance, CA, USA).
The additional tissue was placed in a 96% ethanol-based solution with polyethylene glycol and rifampicin (Carbowax®) for at least 30 min, centrifuged, decanted, and placed in a centrifugal plastic tube to be fixed with 10% formalin to create cell blocks. Cell blocks were then placed on rice paper inside inclusion capsules and processed to generate paraffin blocks. The needle was routinely irrigated with Carbowax® to place any residual tissue in the solution. There was no pathologist or cytotechnologist present in the endoscopic room during the procedure.
The samples sent for histological analysis were placed in 10% formalin and then processed for paraffin inclusion. Subsequently, sections were generated and dyed with hematoxylin and eosin for histopathological analysis.
Statistical Analysis
SPSS software for Windows v.25 (IBM Corp., Armonk, NY, USA) was used for analysis. A sample size was calculated for a two-queue hypothesis with a type I error rate set to 0.05, study power of 90%, and β-magnitude of 20%. The required sample calculated for each group was 95 patients. The analysis was performed using 2 × 2 tables to calculate sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy for each needle type. Proportions were compared using a Z test. For quantitative variables, a descriptive analysis was performed using Student’s t test. Qualitative and unpaired outcome variables were described using Fisher’s exact test. p < 0.05 denoted statistical significance. We performed a multiple logistic regression model to determine the probability of reaching diagnosis according to the type of needle used. We adjusted our model by age, size of the tu-mor, and biopsy route. We did not include site of tumor in the analysis, as we found it to be colinear with biopsy route.
For statistical analysis and the construction of 2 × 2 tables, biopsies under categories I-IV were considered negative for malignancy. Biopsies under categories V and VI were considered positive. Biopsies considered positive for malignancy in patients who had a favorable evolution after 6 months were considered false positives. Biopsies negative for malignancy in patients who experienced progression of neoplastic disease within 6 months were considered false negatives, as were those in patients diagnosed with malignancy using other sampling methods such as surgery or image-guided biopsy or by repeating a EUS-guided FNA/FNB.
Results
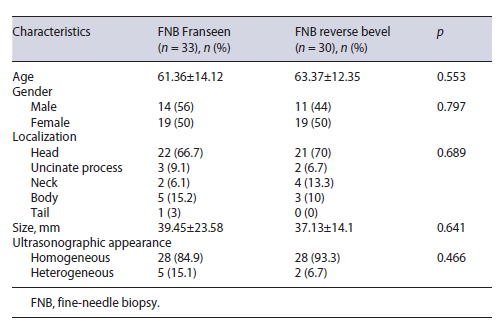
In total, 63 patients with solid pancreatic lesions were identified. The Franseen needle group included 33 patients (mean age, 61.36 ± 14.12 years), including 19 females (57.6%). The most common tumor location in this group was the head of the pancreas (66.7%), and the mean tumor size was 39.45 ± 23.58 mm. The reverse bevel needle group included 30 patients (mean age, 63.37 ± 12.35 years), 19 of whom were female (63.3%). The most common tumor location in this group was the head of the pancreas (70%), and the mean tumor size was 37.13 ± 14.1mm.
There were no significant differences in age, gender, tumor location and size, and ultrasonographic features between groups. Baseline characteristics are presented in Table 1.
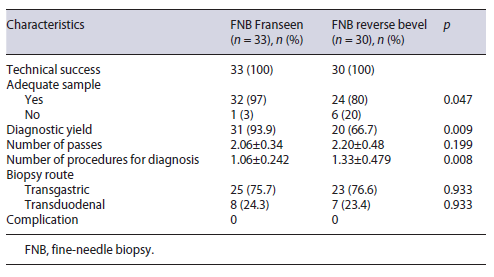
The technical success rate was 100% in both groups. The rate of sample adequacy was 97% in the Franseen needle group, compared with 80% in the reverse bevel needle group (p = 0.047). The diagnostic yield in the Franseen needle group was 93.9%, versus 66.7% in the reverse bevel needle group (p = 0.009). The mean numbers of passes were 2.06 ± 0.34 in the FNB Franseen needle group and 2.20 ± 0.48 in the reverse bevel needle group. No complications were recorded in either group. The main results are presented in Table 2.
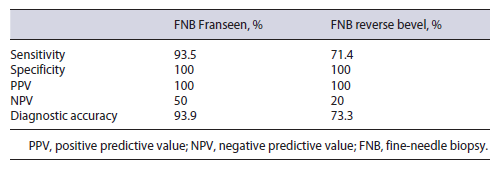
In the Franseen needle group, 29 of 33 biopsies were true positives for malignancy, whereas the remaining 4 patients consisted of 2 true negatives and 2 false negatives, resulting in a sensitivity and a specificity of 93.5 (95% confidence interval [CI] = 78.58-99.21) and 100% (95% CI = 15.81-100), respectively. The Franseen needle group had a positive predictive value of 100% and a negative predictive value of 50% (95% CI = 20.74% to 79.26%.
In the reverse bevel needle group, 20 of 30 biopsies were true positives for malignancy, whereas the remaining biopsies included eight false negatives and two true negatives, resulting in a sensitivity and a specificity of 71 (95% CI = 51.33-86.78) and 100% (95% CI = 15.81-100), respectively. The reverse bevel group had a positive predictive value of 100% and a negative predictive value of 20% (95% CI = 12.22-30.99%). The results of sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy for each needle group are presented in Table 3.
Table 3 Sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy for each needle group
In the Franseen needle group, 2 patients repeated EUS-guided biopsy, and the second biopsy was positive for malignancy in both cases. Percutaneous tomography-guided biopsy was requested for 1 patient in the Franseen needle group diagnosed with lymphoma to obtain additional tissue for immunohistochemistry staining.
In the reverse bevel needle group, of the 10 patients with nondiagnostic EUS samples, 5 repeated EUS-guided biopsy to establish the diagnosis. Two patients required a second sampling technique, and they were diagnosed via CT-guided biopsy. Two patients were proposed for best supportive care after a nondiagnostic result, but with evidence of progressive neoplastic disease, and they died within 6 months of follow-up. One patient was diagnosed by surgery.
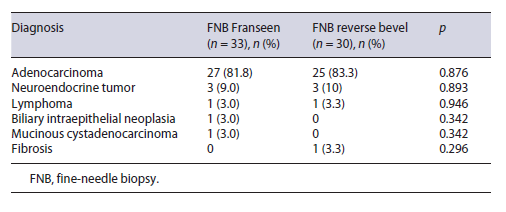
The most common pathological diagnosis was adeno-carcinoma in 82.5% of patients, followed by neuroendocrine tumor in 9.5% of patients. Diagnostic data are summarized in Table 4.
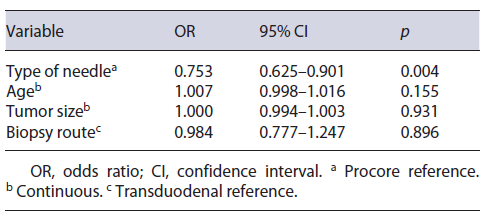
In multiple regression analysis, using the reverse bevel needle, compared to the Franseen needle, resulted in a lower risk of reaching diagnosis, accounting for the other factors. With the reverse bevel needle, we found 0.75 times the risk of reaching diagnosis, compared to the Franseen needle. Furthermore, age, tumor size, and biopsy route did not show significance when assessing their odds for reaching diagnosis. The results of regression analysis are presented in Table 5.
Discussion/Conclusion
This comparative study regarding the diagnostic performance of two FNB needles focused specifically on needle design, as the groups were balanced in terms of needle gauge, sampling technique, lesion size, and number of passes. To our knowledge, this is the first comparative analysis between the 22-gauge FNB Franseen needle and 22-gauge FNB reverse bevel needle. Our results illustrated that the FNB Franseen needle is better than the FNB reverse bevel needle regarding sample adequacy and diagnostic yield.
In particular, we observed high diagnostic performance in the Franseen needle group. A meta-analysis of pancreatic solid lesions sampled using only 22-gauge Franseen needles recorded a pooled rate of diagnostic yield of 92.7% (95% CI = 86.4-96.2) and noted no difference in conducting the rapid on-site evaluation [11]. A second recent meta-analysis comparing FNB needle performance reported a sample adequacy rate of 97% (95% CI = 94.8-99.3) and a diagnostic accuracy rate of 95% (95% CI = 92.5-97.5) for pancreatic lesions sampled using FNB Franseen needles, consistent with our results [2]. Regarding the diagnostic performance of the reverse bevel needle, our results were inferior to published findings. A subanalysis of a study comparing FNA and FNB reverse bevel needles reported a diagnostic yield of 87% for pancreatic lesions. Nevertheless, recent publications comparing different FNB needles recorded diagnostic yields of 67-81% for the FNB reverse bevel needle in pancreatic lesions in line with our results [9, 12-14]. To our knowledge, the randomized clinical trial conducted by Karsenti et al. [9] was the first study to compare the Franseen and the reverse bevel needles. However, their study used a 20-gauge reverse bevel needle, which we believe can limit tissue sampling in certain endoscopic positions. This study reported that the Franseen needle showed superior sample adequacy (100 vs. 82%) and diagnostic accuracy (87 vs. 67%). One of the observa-tions of this analysis was that the Franseen needle provided almost twofold more tissue than the 20-gauge reverse bevel needle, which may be attributable to stiffness and poor maneuverability associated with the bigger caliber [9]. In our comparison, we included only the 22-gauge caliber and obtained similar results and thus we can conclude that the higher diagnostic yield and more adequate tissue acquisition might be exclusively associated with the design of the needle independently of the needle caliber. Young Bang et al. [15] prospectively compared sample cellularity with different 22-gauge needle designs and tissue sampling techniques including the Franseen and reverse bevel needles. Samples collected by forktip or Franseen needles had significantly higher cellularity than samples collected by reverse-bevel or Menghinitip needles (p < 0.001). Pancreatic neoplasias were identified with greater than 90% accuracy using Franseen needles with an odds ratio of 5.18 in comparison to reverse bevel needles (95% CI = 2.53-10.6, p < 0.001). The reported sensitivity for pancreatic lesions sampled with suction was in accordance to our study, with a sensitivity of 73.1% (52.2-88.4) for reverse bevel needles and 92.6% (75.7-99.1) for Franseen needles (p = 0.022). In a subanalysis the best cellular-ity was achieved with a stylet retraction technique for the Franseen needles and a suction technique for the reverse bevel needles [15].
We defined two as the standard number of needle passes for the FNB procedure in our study. A retrospective cohort showed that the tissue sample adequacy rate for histological diagnosis per pass using 22-gauge Franseen needles was 89% for the first pass increasing to 99% after the second pass, without further improvement with additional passes [16]. Another retrospective study of 38 patients with pancreatic lesions biopsied using FNB Franseen needles recorded a histological diagnosis rate of 96.7% with an average of 2.1 passes [17]. Stathopoulos et al. [18] prospectively studied the quality of specimens sampled with 22-gauge Franseen needles observing a high-quality histology specimen with a Payne score of 3 in 92.5% of patients after 2 needle passes with a diagnostic accuracy of 85%. Furthermore, a subanalysis of a meta-analysis comparing the performance of FNB reverse bevel and FNA needles determined than an average of 1.3-1.4 passes was required to make a diagnosis using an FNB reverse bevel needle [19].
Twenty-two-gauge FNB needles may have the ideal size for pancreatic tissue sampling, in contrast to FNA needles, in which a smaller 25-gauge caliber may have slightly better sensitivity [20, 21]. The differences between the 22- and 25-gauge FNB needles have not been extensively studied. Two studies detailed the performance of 25-gauge FNB Franseen needles, reporting sample adequacy rates of 79 and 82%, respectively, which may be in-ferior to the aforementioned rates for 22-gauge needles [22, 23]. A randomized prospective study compared diagnostic yields for 25- and 22-gauge Franseen needles in patients with solid pancreatic lesions finding no significant difference in diagnostic yield (98 vs. 88%, p = 0.105, respectively), however finding that the 25-gauge group required additional passes to obtain an adequate cell block (1.6 ± 0.6 vs. 0.4 ± 0.7, p = 0.001) [24]. A second noninferiority study compared the same needles finding no statistical difference in adequate histological assessment, but with a superiority in high-quality tissue acquisition with the 22-gauge needle in 45.5 versus 25% in the 25-gauge group [25]. A prospective randomized trial compared the histological core procurement rate using the Gerke Score in patients with peripancreatic and pancreatic lesions finding histological core procurement rates of 87.1 versus 97.1% for the 25- and 22-gauge needles, respectively, with a better high-quality specimen rate in the 22-G group (70.0 vs. 28.6%, respectively; p < 0.001), but no difference in overall diagnostic accuracy [26].
Our study did not evaluate macroscopic on-site evaluation (MOSE) by the endoscopist. The examination of macroscopic whitish visible core or bloody tissue granules in the tissue sampled from FNB needles may further increase diagnostic accuracy. So et al. [27] found that sampling heterogenous lesions with 22-gauge Franseen needles in association with MOSE provides a high diagnostic accuracy of 97.3%. With only a median of 2 or 3 passes required to get adequate tissue in 91.2% of the patients, only 5.3% requiring 4 or more passes. Standardization of MOSE protocols are yet to be defined.
The main limitations of our study were its retrospective design and the small sample size in each group. But even with a small sample size our study was able to accurately detect a significant difference between the two nee-dle groups, and the regression model also reached statistical significance as performed. The study strengths were that the compared groups were homogeneous and all relevant information was available for comparing outcome variables. Another advantage was that the pathologists who analyzed the samples were blinded to the needle used. Our results should be further confirmed in prospective randomized trails.
In conclusion, this study demonstrated that the 22-gauge FNB Franseen needle is more effective for EUS-guided sampling of pancreatic solid lesions than the 22-gauge FNB reverse bevel needle.