Introduction
Gastric cancer is the 5th most common cancer worldwide and the 3rd leading cause of cancer-related death [1]. Portugal is a country of moderate to high incidence, with an estimated crude incidence rate of 28.0/100,000 in 2018 and a crude mortality rate of 22.1/100,000. This high lethality rate is due to the fact that more than half of the patients with gastric cancer are diagnosed at advanced stages (at least in non-screened populations), and overall 5-year survival of patients with gastric cancer is 31% according to the American Cancer Society data [2]. Although gastric cancer incidence has been declining over the past century, it is expected that the number of new cases will increase in the next decades due to an ageing population [3, 4].
The risk factors for intestinal-type gastric adenocarcinoma, the most frequent subtype of gastric cancer and the more preventable, can be divided into non-modifiable and modifiable. Age, male sex, family history and race are the more important non-modifiable risk factors. The incidence rate of gastric cancer increases progressively with age, and male sex is also associated with an increased risk of both non-cardia (2-fold) and cardia (5-fold) gastric cancer [5, 6]. Family history is also a well-established risk factor for gastric cancer, with a reported risk of 2- to 10-fold, although only 5% of the gastric cancer cases are caused by an autosomal dominant trait [7, 8]. The majority of cases of familial aggregation are probably explained by unknown genetic alterations and also by a high degree of exposure to shared environmental carcinogens.
Regarding modifiable risk factors, Helicobacter pylori infection, smoking, low socioeconomic status, high intake of salty and smoked foods, and low consumption of fruits and vegetables are the most common reported risk factors [3]. H. pylori is a type I carcinogen and contributes to 75-89% of all non-cardia gastric adenocarcinomas [9]. Although mass eradication programmes have shown to significantly decrease gastric cancer incidence in high-risk areas, it is unclear whether this strategy is beneficial and cost-effective in areas of low or moderate risk [10, 11]. Furthermore, the high resistance of H. pylori to antibiotics could decrease the effectiveness of this primary prevention strategy [12].
In this review we summarize the findings of our studies on this topic, which can contribute to improve the diagnosis and management of patients with precancerous conditions and early neoplastic lesions in Western countries.
Diagnosis of Preneoplastic Conditions
Why Is It Important?
Intestinal-type gastric adenocarcinoma (Lauren classification) is the most frequent type in high-incidence areas, is related with environmental factors (mainly H. pylori infection) and is the last step of the gastric carcinogenesis cascade [13]. According to this model, H. pylori infection and chronic gastritis are the first steps, and a significant proportion of infected individuals develop chronic atrophic gastritis and intestinal metaplasia (precancerous conditions), the background in which dysplasia (prencancerous lesion) and adenocarcinoma develop. This progression generally takes decades, and is influenced by host genetic background, H. pylori genotype and environmental co-exposures (smoking, salt intake). H. pylori eradication and lifestyle modifications can thus decrease the incidence of intestinal-type gastric adenocarcinoma.
The incidence of gastric cancer in patients with precancerous conditions was evaluated in some studies. A Swedish cohort with long follow-up found a standardized incidence ratio of 2.8 (95% CI 2.3-3.3) for patients with atrophic gastritis and of 3.4 (95% CI 2.7-4.2) for patients with intestinal metaplasia (IM) [14]. The 20-year gastric cancer risk in this North European cohort was 2.0% in the atrophic gastritis group and 2.56% in the IM group. A Dutch cohort also found an annual gastric cancer incidence of 0.1% for atrophic gastritis and 0.25% for intestinal metaplasia [15]. Thus, we can broadly say that in low-incidence countries the annual risk of developing neoplasia is 0.1-0.25%, which gives a long-term risk of 2-5% in 20 years, but we should bear in mind that these rates are higher in Eastern countries. For instance, a Japanese study showed a higher progression risk that can reach 10% in 5 years for patients with severe atrophy [16].
The slow progression between the development of precancerous conditions and dysplasia/neoplasia can allow the identification of early neoplastic lesions if these patients with a higher risk of intestinal-type gastric adenocarcinoma undergo endoscopic surveillance. Screening gastric cancer within colorectal screening programmes is also cost-effective in intermediate-risk countries [17]. However, it remains unclear how the identification of these high-risk patients can be improved.
How Can We Improve the Identification of Gastric Precancerous Conditions?
The ability of non-invasive markers (e.g., serum pepsinogens and/or H. pylori serology) to identify individuals with high-risk conditions is only moderate [18]. A meta-analysis found that the sensitivity of pepsinogens for atrophic gastritis was 0.69 (95% CI 0.55-0.80), and the pooled specificity was 0.88 (95% CI 0.77-0.94). These markers can thus have a role in mass screening, but their sensitivity is suboptimal, the heterogeneity concerning accuracy is high and the best cut-offs are unclear, and they were never adopted in European countries. The identification of patients with precancerous conditions in the West is thus not systematic, but the diagnosis can be opportunistically made when a patient is submitted to an endoscopy performed for gastrointestinal symptoms or signs. Endoscopy is the gold-standard for detection of gastric pathology, but the concordance between endoscopy and histology concerning precancerous conditions is suboptimal, and random biopsies are advised in order to diagnose atrophy or IM [19-23]. However, in a real-world setting, biopsies are often not performed in the absence of recognized abnormalities since biopsies increase bleeding risks, procedural time and costs. Another problem is that these precancerous conditions are unevenly distributed, and thus random samples can be prone to sampling error. Thus, how can we improve the identification of precancerous conditions when a patient is submitted to endoscopy?
Conventional chromoendoscopy (CE) is frequently used in Eastern countries with high gastric cancer incidence such as Japan and Korea, but it did not gain wide acceptance in Europe. In the last decade, virtual CE was developed - a technique in which the image is modified to increase the contrast between structures in order to achieve a better image of the glandular architecture and microvascular pattern. This is achieved using only a part of the visible spectrum by using optical or digital filters, decreasing the amount of red light in the image and narrowing the bandwidth of green and blue light. There are now some CEs available, such as flexible spectral imaging color enhancement, i-scan and blue-laser imaging, but narrow-band imaging (NBI) was the first commercially available virtual CE system that entered clinical practice, and several studies mainly from Japan and using magnification endoscopes showed a high accuracy in the diagnosis of gastric precancerous conditions. However, the majority of the studies were conducted in Eastern countries, most were unicentric and there was a lack of studies evaluating the impact of NBI without the use of magnification endoscopes.
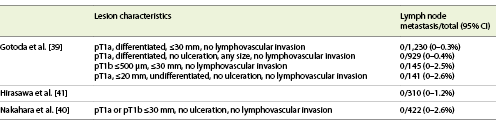
In 2012, our group performed a derivation and multicentre validation of a simple classification for gastric pathology (Fig. 1) [24]. The correlation of previously described NBI features (regular tubulovillous mucosal pattern, irregular pattern and light blue crest) with histology was evaluated, as well as inter-observer reproducibility, and a simple classification was proposed and further validated in 40 patients/100 videos. Pattern A (normal) showed a sensitivity of 0.76 (95% CI 0.63-0.89) and a specificity of 0.94 (95% CI 0.83-0.97) for normal mucosa (accuracy 0.83, 95% CI 0.75-0.90); pattern B (IM) presented a sensitivity of 0.90 (95% CI 0.79-1.00) and a specificity of 0.81 (95% CI 0.72-0.91) for the diagnosis of IM (accuracy 0.84, 95% CI 0.77-0.91); pattern C had a sensitivity of 0.84 (95% CI 0.70-0.99) and a specificity of 0.98 (95% CI 0.95-1.00) for dysplasia/cancer (accuracy 0.95, 95% CI 0.90-0.99). Experts achieved higher accuracy compared with the non-experienced observers.
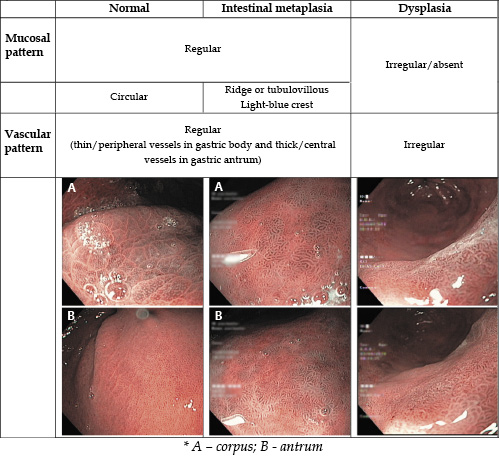
Fig. 1 NBI simplified classification for gastric pathology (adapted from Pimentel-Nunes et al.[24]). A Corpus. B Antrum.
Subsequently, we performed a multicentric prospective study to evaluate this classification in a real-world setting, including 238 patients and 1,123 biopsies [25]. In this study, the overall diagnostic accuracy increased from 83% with high-definition white-light endoscopy to 94% with NBI, increasing also the sensitivity for IM (53% [95% CI 47-58%] vs. 87% [95% CI 84-91%]) and for dysplasia (74% [95% CI 52-90%] vs. 92% [73-99%]), without compromising specificity for IM and dysplasia (both >97%). The results of this study suggest that NBI should be used for target biopsies instead of performing random biopsies in order to increase the diagnostic yield of upper gastrointestinal endoscopy in the identification of patients with precancerous conditions, and this is nowadays recommended in European guidelines [26].
Which Is the Best Method to Stage Precancerous Conditions?
Gastric precancerous conditions are prevalent in the general population - a meta-analysis found that the prevalence of chronic atrophic gastritis and IM was 33.4% (95% CI 25.9-40.8%) and 25.0% (95% CI 19.5-30.5%), respectively, in endoscopy-based studies, and that the prevalence of chronic atrophic gastritis was 23.9% (95% CI 18.6-29.2%) in serology-based studies [27]. The high prevalence and the relatively low annual incidence rate make impracticable to endoscopically follow up all the patients with precancerous conditions, and there is the need to select those at higher risk of progression. Family history of gastric cancer and incomplete type metaplasia (intestinal metaplasia type III or colonic metaplasia) were associated with an increased risk of progression [28-31]. The extent of precancerous changes has also been found to be related with progression risk and is probably the more reliable marker to stratify the risk, although there is controversy on which is the best method to stage precancerous conditions - histological or endoscopy-based classifications.
Histological systems such as OLGA and OLGIM (Operative Link on Gastritis Assessment and Operative Link on Gastric Intestinal Metaplasia assessment, respectively) were found to correlate with gastric cancer risk. A meta-analysis found that high-risk OLGA/OLGIM stages (OLGA/OLGIM III/IV) are associated with a significantly higher gastric cancer risk (OLGA III/IV: odds ratio [OR] 2.64, 95% CI 1.84-3.79 [case-control studies]; OLGIM III/IV: OR 3.99, 95% CI 3.05-5.21 [case-control studies] and risk ratio 27.70, 95% CI 3.75-204.87 [cohort studies]) [32]. However, although accurate, grading the severity of the lesions is not always possible and not always reported by pathologists, and it makes sense that an endoscopic assessment of the entire gastric mucosa can also select patients for surveillance with similar accuracy (or even better since it is not subjected to sampling a small portion of gastric mucosa). Furthermore, the higher interobserver agreement for IM both at histology and at endoscopy, along with the higher odds of gastric cancer using OLGIM (when compared with OLGA), favor that IM is preferable over atrophy for the stratification of gastric cancer risk.
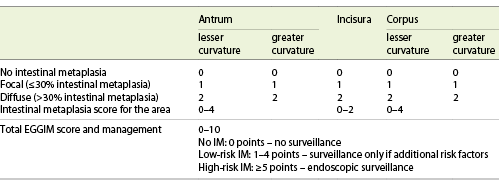
In a proof-of-concept study, we found that the sensitivity and specificity of NBI for extensive IM was high (0.92, 95% CI 0.67-0.99, and 0.96, 95% CI 0.79-0.99, respectively), and >90% of patients were correctly allocated to surveillance or no surveillance based on the endoscopic evaluation alone [33]. In a post hoc analysis of the multicentre validation of the simple NBI classification, an endoscopic classification of IM (Endoscopic Grading of Gastric Intestinal Metaplasia - EGGIM; Table 1) that was subsequently validated in a multicentric study was also proposed. According to this scale (0-10 points), the stomach is divided into 5 areas (lesser and greater curvature of the antrum, incisura, lesser and greater curvature of the body), and to each area 0-2 points are assigned according to the extension of IM in that area (0 points if no IM; 1 point if focal IM [≤30% of the area]; 2 points if diffuse IM [>30% of the area]). We found that EGGIM correlates well with the OLGIM classification - the endoscopic assessment alone had a sensitivity of 89% for the detection of high-risk OLGIM stages (OLGIM III-IV), showing that the great majority of patients who benefit from surveillance can be identified without biopsies [34]. This scale has recently been shown to correlate with early gastric neoplasia risk in a case-control study - EGGIM 5-10 was associated with a significantly increased risk of neoplasia in multivariable analysis (adjusted OR 21.1, 95% CI 4.9-90.2) [35].
Table 1 Endoscopic Grading of Gastric Intestinal Metaplasia (EGGIM) scale (adapted from Pimentel-Nunes et al. [25] and Esposito et al. [34])
Together, these studies confirm the usefulness of NBI to increase the detection of patients who benefit from surveillance and suggest that risk stratification based on endoscopic evaluation alone is feasible and is associated with both OLGIM stages and gastric neoplasia risk, although biopsies are still needed if H. pylori status is of interest, given the low accuracy of virtual CE for the diagnosis of H. pylori infection.
Treatment of Early Gastric Cancer
Which Is the First-Line Treatment for Patients with Early Gastric Lesions?
Early gastric cancer (EGC) is defined as a cancer confined to the mucosa or submucosa, irrespective of regional lymph node involvement [36]. Gastrectomy with lymphadenectomy was the standard treatment for early gastric lesions until the development of advanced endoscopic resection techniques and the perception that surgical treatment could not be necessary for the majority of EGCs, that have a low risk of lymph node metastasis (LNM). Indeed, the rate of LNM in EGC is between 0 and 20% (0-4% in intramucosal carcinomas and 0-20% in carcinomas with submucosal invasion), and under certain conditions this risk is minimal or null (Table 2).
Gastrectomy is a surgical procedure that involves the resection of the stomach and regional lymph nodes and achieves high rates of complete resection and long disease-free survival and overall survival (5-year survival >90%) [37, 38]. Gastrectomy also eliminates the risk of metachronous gastric lesions in total gastrectomy and significantly reduces this risk in subtotal gastrectomy since more than two thirds of the stomach are generally removed. On the other hand, the procedure has a significant risk of adverse events, and the removal of the stomach leads to impairment of its reservoir and digestive function, which can result in symptoms, impairment of nutrient absorption (namely iron and vitamin B12) and potentially impact health-related quality of life (HR-QoL).
As gastrectomy is a major surgical procedure with a significant risk of adverse events and impact on HR-QoL, and as it was perceived that lymphadenectomy could not be needed in the majority of EGC, several studies evaluated risk factors for LNM in EGC in order to define criteria for endoscopic resection. Three landmark studies evaluated the association of tumor characteristics with the presence or absence of LNM and found that when certain histopathological characteristics were met there was no LNM, which were in the basis of the proposed curability criteria for endoscopic resection (Table 2) [39-41].
These studies were useful to define indications for endoscopic therapy, which is indicated when there is a low risk of LNM and the lesion is suitable for en bloc resection.
Endoscopic mucosal resection using a cap-fitted endoscope and a snare was first described in 1993 by Inoue et al. [42] and was used thereafter for the resection of mucosal gastric adenocarcinomas. This technique is effective and safe, although due to the diameter of the cap, lesions above 15 mm generally cannot be resected en bloc, limiting accurate histopathological assessment that is important for the decision on the need to undergo further surgical treatment. Moreover, piecemeal and/or incomplete resections are frequently associated with local recurrence that should be treated with further endoscopic or surgical treatment [43].
Endoscopic submucosal dissection (ESD) was developed to overcome the size limitations of endoscopic mucosal resection, allowing en bloc resection of lesions virtually of any size with the aim of achieving higher complete resection rates, adequate histopathological assessment and lower recurrence. This technique was first performed by Gotoda et al. [39] in 1997 using an insulation-tipped electrosurgical knife (IT-knife) that was developed by Hosokawa and Yoshida in 1995 [43, 44]. In this technique, the margins of the lesion are assessed with conventional or virtual CE, and then coagulation marks are placed circumferentially around lesion margins. After that, a solution is injected into the submucosal layer, and access to the submucosa is gained generally performing 3-4 electrosurgical incisions with a pre-cut needle knife [45]. These incisions are used to perform a circumferential incision with a knife and then the submucosa is dissected in the horizontal plan under direct vision, allowing the resection of lesions in a single fragment.
The outcomes of endoscopic mucosal resection and ESD have been compared in several studies, and 3 meta-analyses were published to compare their efficacy and safety outcomes [46-48]. These studies found that although ESD had a significantly higher mean operative time, it was associated with significantly higher rates of en bloc resection (93-94 vs. 56-67%), complete resection (86-92 vs. 48-52%) and lower recurrence (0.2 vs. 5.2%). However, ESD was associated with a higher perforation risk (3.2 vs. 1.2%), although bleeding rates were similar between the two techniques (7.0 vs. 7.2%).
In Europe, the lower incidence of gastric cancer and the absence of gastric screening programmes results in a low absolute number of early lesions that are amenable for endoscopic therapy, which impacted the learning curve of ESD and its widespread dissemination. ESD was introduced in our centre (Portuguese Oncology Institute of Porto [IPO-Porto]) in 2003, and on our first report promising results with this technique were found [49]. In 2014 we retrospectively evaluated the short and long-term outcomes of 164 patients submitted to gastric ESD in IPO-Porto between 2005 and 2014 [50]. We found that en bloc and complete resection (R0) were achieved in 95.3 and 93.8%, respectively, with a curative resection rate of 84.5%. In the entire cohort, and during a median follow-up of 40 months, the overall survival was 94.5 and 89.5% at 1 and 3 years, respectively, and the disease free-survival was 99.4%, with only 1 patient dying of gastric cancer (a patient with non-curative resection who refused further surgical treatment).
These findings suggest that ESD is effective in the treatment of early neoplastic lesions including long-term follow-up, although comparative studies with competing treatments are needed in order to define which is the first-line treatment. However, studies comparing endoscopic and surgical treatment for EGC, namely evaluating the impact on HR-QoL and patients’ perspectives, were scarce and all of them retrospective [51, 52], and there were no prospective studies with pre-post assessment evaluating the impact of surgical and endoscopic treatment on HR-QoL. Thus, a prospective study was conducted comparing the outcomes of endoscopic and surgical treatment in patients with early gastric neoplasms, focusing mainly on safety and patient-reported outcomes [53].
In this study including 254 patients with early gastric neoplasms (153 in the ESD arm and 101 in the gastrectomy arm), we found that ESD has a significantly better safety profile (intraprocedural adverse events 1.3 vs. 10.9%, p < 0.001; severe postprocedural adverse events 7.8 vs. 21.8%, p = 0.003; surgical re-intervention 0.7 vs. 10.9%, p < 0.001), being also associated with shorter procedural duration (mean difference -92 min, p < 0.001) and shorter in-hospital stay (3 days [IQR 3-4] vs. 11 days [IQR 9-17]).
Regarding patient-reported outcomes, ESD was associated with significant advantages on several symptom scales, role function and global health status at 1 year. While ESD was not associated with significant deterioration in any symptom scale, gastrectomy was associated with significant worsening of several symptoms compared with baseline that persisted 1 year after treatment (namely fatigue, pain, appetite loss, diarrhoea, dysphagia, eating restrictions, taste and body image). Regarding functional scales, between-group comparisons showed a significant benefit of ESD in physical, role, emotional and social functioning at 1 month, physical and role functioning at 3-6 months, and role functioning at 1 year. With respect to worry of recurrence, there were no significant differences between groups regarding fear of recurrence, new tumours or death. Regarding global health status (visual analogue scale, 0-100 points), ESD was associated with improvement at 1 year (+5.58; p = 0.007), while in the gastrectomy group there was a decrease in global health at 1 year (−4.35; p = 0.17), corresponding to a net benefit of 9.93 points in the mean global health change favouring ESD (p = 0.006). We also found that the higher risk of metachronous lesions and recurrence (of which patients are aware due to the information given before endoscopic resection) does not seem to significantly influence emotional and psychological dimensions of HR-QoL.
Prediction of Adverse Outcomes of Gastric ESD
Even if ESD is safer than gastrectomy and preferred by patients, the technique is associated with a long learning curve and a non-negligible risk of adverse events, and it is important to predict the outcomes of ESD to improve patient selection and patient information.
Postprocedural bleeding (PPB) is the most common adverse event after ESD and is associated with prolonged hospital stay and the need of transfusion, endoscopic intervention, surgery, and ultimately death. Thus, it is important to evaluate risk factors for PPB to identify patients who can benefit from additional preventive measures (e.g., tissue shielding or hemoclip application) or adaptation in surveillance strategies after the procedure (namely time of inpatient surveillance) and also better communication of the information regarding the risk of this adverse event. The benefit of routinely performing second-look endoscopy after the procedure even in the absence of clinical signs of hemorrhage was also a matter of controversy.
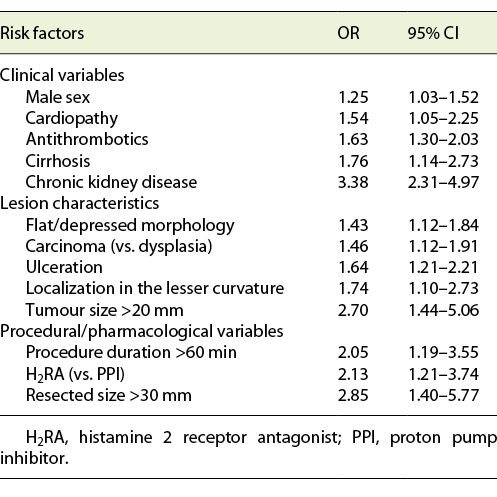
Our systematic review and meta-analysis that included 71 studies found that PPB occurs in 5.1% of the cases and identified risk factors significantly associated with PPB (Table 3) [54]. Clinical variables associated with PPB were male gender, heart disease and antithrombotic therapy, cirrhosis and chronic kidney disease. Tumor-related characteristics significantly associated with this outcome were tumor size >20 mm, resected specimen size >30 mm, localization in the lesser curvature, flat or depressed morphology, carcinoma histology, ulceration and expanded criteria. Periprocedural risk factors for PPB were procedure duration >60 min and the use of histamine-2 receptor antagonists as acid-suppressive therapy (instead of proton pump inhibitors). Second-look endoscopy was not associated with lower PPB (ORbleeding 1.34, 95% CI 0.85-2.12), and it was found that more than one half of bleeding episodes occur before second-look endoscopy, and even prophylactic hemostasis on second-look endoscopy is not capable of significantly reducing PPB. These findings strongly suggest that second-look endoscopy should not be routinely performed and can help to define individualized management - patients with 0-1 risk factors can be considered for early discharge, while patients with more risk factors can benefit of a more prolonged inpatient surveillance and may benefit from additional prophylactic measures (e.g., mucosal closure, selective artery clipping and use of poly glycolic acid sheets and fibrin glue) [55]. However, the benefit of these preventive measures needs to be assessed in further studies.
Another drawback of ESD is that nearly 20% of the lesions resected do not meet curative criteria, and further surgical therapy is needed [56]. The selection of patients for ESD is based on endoscopic evaluation since endoscopic ultrasound does not seem to improve selection and is not routinely recommended in European guidelines [56]. It is thus important to evaluate pre-resection risk factors for non-curative resection, which can improve patient information, patient selection and decision making.
In our retrospective cohort of 194 lesions submitted to ESD, male sex, tumor size ≥20 mm and carcinoma in pre-resection biopsies were associated with non-curative resection, although only the presence of carcinoma in pre-resection biopsies was identified as an independent predictor for this outcome (adjusted OR 3.04, 95% CI 1.02-9.06) [50]. This suggests that patients with carcinoma already present on pre-resection biopsies have a lower probability of curative resection, although it is difficult to value this information in clinical decision making and patient information. A further study was performed using Bayesian statistical methods in order to provide readily human-interpretable evidence [57]. In this study, using patient and lesion-related variables available at the pre-resection stage (American Society of Anesthesiologists Physical status, lesion size, morphology, location and pre-resection histology), Bayesian models to predict non-curative resection and PPB were constructed, and their accuracy was evaluated. The models for both outcomes presented good discriminative power (area under receiver-operating characteristic ∼80% in the derivation cohort and ≥74% in cross-validation), and although Bayesian models’ performance was not statistically significant from logistic regression models, they provide information that is more usable in clinical practice. Risk matrices were constructed to allow utilization in everyday practice and showed that the probability of curative resection decreases with lesion size ≥20 mm, more advanced histology in pre-resection biopsies, localization in the middle third of the stomach and polypoid morphology. We also performed a systematic review that identified location in the upper third of the stomach (OR = 1.49 [95% CI 1.24-1.79]), depressed morphology (OR = 1.49 [95% 1.04-2.12]) and expanded indication criteria or beyond (OR = 3.56 [2.31-5.48]) as risk factors for non-curative resection [58].
What Is the Best Management after Gastric ESD?
After endoscopic resection, the specimen is evaluated in order to classify the resection. According to European and Japanese guidelines, the resection is considered curative when all the following conditions are fulfilled: en bloc resection, tumor size ≤2 cm, histologically of differentiated type, pT1a, negative horizontal margin (HM0), negative vertical margin (VM0) and no lymphovascular infiltration (LV-) [56, 59]. The resection is also curative when there is minimal risk of LNM (expanded criteria), i.e., the lesion was resected en bloc, HM0 and VM0, LV-, and all the following conditions are fulfilled:
(a) tumour size >2 cm, differentiated type, pT1a, without ulceration;
(b) tumour size ≤3 cm, differentiated type, pT1a, with ulceration;
(c) tumour size ≤2 cm, undifferentiated type, pT1a, without ulceration;
(d) tumor size ≤3 cm, differentiated type, pT1b sm1 (submucosal invasion ≤500 µm from the muscularis mucosa).
After resection, patient management is based on this histopathological evaluation. In patients meeting curative criteria, guidelines recommend annual or biannual endoscopy (and abdominal ultrasonography or computed tomography in cases of expanded indication). H. pylori should also be treated if positive to decrease the risk of metachronous lesions. On the other hand, if the resection is considered non-curative (high-risk resection), it is recommended to pursue a curative oncological resection with gastrectomy and lymphadenectomy unless the patient is unfit for surgery or refuses surgical treatment. If the resection does not meet strict curative criteria and there is a local recurrence risk (e.g., positive or indeterminate horizontal margin with clear vertical margin) but the risk of LNM/distant metastasis is null or minimal, the decision should be individualized. In these cases, tight surveillance, further endoscopic re-resection or surgical treatment are acceptable options, depending on the findings of the resected ESD specimen and patient preferences.
In cases of curative resection, endoscopic follow-up is needed to timely detect metachronous lesions. The knowledge of the risk of metachronous lesions is important to define the follow-up schedule, and identification of risk factors for metachronous lesions can contribute to individualized surveillance. In our retrospective cohort with long-term follow-up, we found that the cumulative risk of metachronous lesions was 18.4%, and the median time to detection was 24 months. Older age was identified as an independent risk factor for metachronous development (OR10 years 1.68, 95% CI 1.03-2.74). Our findings are in line with other studies that identified older age as a risk factor for metachronous lesions [60]. Other factors that were associated with metachronous development in other studies were male sex, persistent H. pylori infection and intestinal metaplasia in the body. These results suggest that a tight endoscopic surveillance should be performed, even many years after resection because as age increases so does the risk of metachronous lesions.
In cases of non-curative resection, gastrectomy with lymphadenectomy is the standard treatment, although in certain conditions surveillance can be an option. It is important to compare the overall survival between patients submitted to surgery and patients allocated to surveillance (due to surgery refusal or frailty), since it is unclear whether patients with comorbidities and short life expectancy benefit from surgery in this context. In our retrospective cohort with long-term follow-up, overall survival was significantly higher in patients with curative resection when compared with patients with non-curative/high-risk resections [50]. However, in patients with non-curative/high-risk resection, overall survival was not significantly different between patients submitted to gastrectomy and patients submitted to follow-up, suggesting that an individualized management after non-curative resection is acceptable. Indeed, in case of significant comorbidities, this suggests that not every patient benefits from pursuing an oncological resection.
Our results are in line with a study that found a 5.1% rate of residual disease in gastrectomy specimens, and a low rate of LNM or distant metastasis (3.8%) on long-term follow-up after non-curative resection, and 5-year disease-specific survival was similar between gastrectomy and follow-up groups (98.8 vs. 96.8%) [61]. Another study that included 1,969 patients with non-curative resection (1,064 submitted to surgery and 905 surveilled) also found a similar 3-year disease-specific survival (99.4 vs. 98.7%) but a higher difference in 3-year overall survival (96.7 vs. 84.0%), suggesting that careful follow-up may be acceptable in patients with comorbidities and lower survival expectancy with low risk of LNM [62]. The eCura scoring system was developed to predict LNM based on tumor characteristics and help to predict LNM risk and thus individualized decisions. According to this score, 3 points are assigned if there is lymphatic invasion, and 1 point for each of the following variables: (a) size >30 mm, (b) positive vertical margin (c) venous invasion, (d) submucosal invasion ≥500 µm [63]. Patients can be grouped in 3 LNM risk groups: low (0-1 point; 2.5% LNM risk), intermediate (2-4 points; risk 6.7%) and high (5-7 points; risk 22.7%). This classification was validated, and it was found that cancer-specific survival at 5 years was significantly different between the 3 groups (low-risk 99.6%, intermediate-risk 96.0% and high-risk group 90.1%; p < 0.001).
This suggests that even after non-curative resection the decision to undergo further surgical treatment should be individualized taking into account the patient’s performance status and comorbidities, as well as pathological factors such as the presence of lymphovascular invasion that seems to be the most important prognostic factor for adverse oncological outcomes.
In summary, virtual CE increases the diagnostic accuracy of endoscopic diagnosis, increasing the sensitivity for intestinal metaplasia, and its use can improve the identification of patients with gastric precancerous conditions. Endoscopic grading of IM correlates well with the histological system OLGIM and with the risk of early gastric neoplasia, and can be used to stratify gastric cancer risk. In patients with early gastric lesions, ESD is the first-line treatment since it is associated with a better safety profile and benefits in HR-QoL when compared with surgery. However, the risk of metachronous lesions is high (15-20%) and endoscopic follow-up is necessary. Moreover, the identification of risk factors for non-curative resection and PPB is important to improve patient selection and patient information.