A 60-year-old female patient presented with obstructive jaundice and pruritus. Laboratory tests revealed a total bilirubin of 17.23 mg/dL (direct 14.84 mg/dL) and an elevation of CA 19-9 of 3,820 U/mL. Computed tomography scan showed an infiltrative intrahepatic mass measuring 65 × 55 mm, involving segment IV, with unclear limits and invasion of the common bile duct. The tumour caused capsule retraction, slight dilation of the intrahepatic bile ducts and marked distention of the gallbladder (Courvoisier sign) (Fig. 1). The reported findings were suggestive of an intrahepatic cholangiocarcinoma, in association with hilar and lumbar-aortic lymph nodes enlargement and peritoneal carcinomatosis. Considering the typical radiological findings and the advanced stage of the disease, no further biopsy was performed.
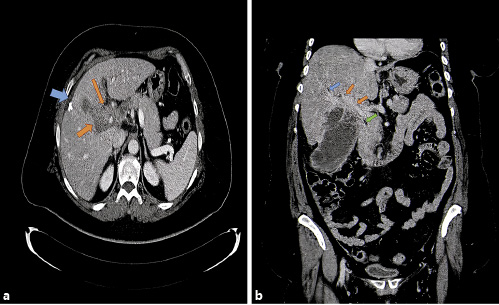
Fig. 1 CT scan showed an intrahepatic infiltrative mass (a) with unclear limits, involving segment IV and causing hilar invasion, capsule retraction, slight dilation of the intrahepatic bile ducts and marked distention of the gallbladder (b). a Orange arrows: intrahepatic infiltrative mass causing hilar invasion; blue arrow: capsule retraction. b Orange arrows: intrahepatic infiltrative mass causing hilar invasion; blue arrow: slight dilation of the right intrahepatic bile duct; green arrow: distal common bile duct.
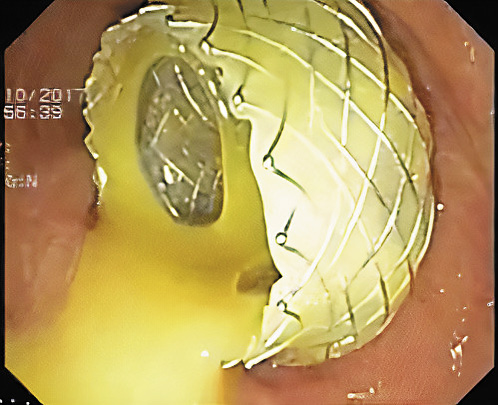
The case was discussed in a multidisciplinary meeting, in which a palliative biliary drainage was proposed. Endoscopic retrograde cholangiopancreatography was not possible due to failed cannulation. A lack of significant dilation of the common and intrahepatic bile ducts was observed, as well as a marked distention and wall thickening of the gallbladder, which suggested some degree of distal common bile duct obstruction. Considering this later aspect, to provide biliary drainage, and to prevent complications such as cholecystitis or gallbladder perforation, an endoscopic ultrasound (EUS)-guided gallbladder drainage was performed. As shown in Figure 2 and 3, an electrocautery-enhanced lumen-apposing metal stent (LAMS) (Hot AXIOSTM, 15 × 10 mm, Boston Scientific, Marlborough, MA, USA) was placed between the dilated gallbladder and the gastric wall, providing adequate biliary drainage. The freehand technique was employed on stent deployment and no balloon dilation was required. The transgastric approach was chosen because it provided a better apposition between the two surfaces. There were no related immediate or late adverse events. Following the procedure, the patient showed improvement of jaundice and normalization of bilirubin levels in 2 weeks. However, functional status deterioration inhibited further chemotherapy. The patient died 2 months after the procedure without related complications.

Fig. 2 Ultrasonographic view of LAMS deployment between the dilated gallbladder and the gastric wall.
Recently, EUS-guided gallbladder stent deployment has emerged as an efficient alternative drainage method to percutaneous or transpapillary gallbladder drainage for patients with acute cholecystitis who are poor surgical candidates [1-3]. Adapted from benign disease, EUS-guided gallbladder drainage has also been described as a palliative drainage method in certain cases of malignant biliary obstruction, when other EUS approaches are not feasible, if patency of the cystic duct is assured [4, 5].