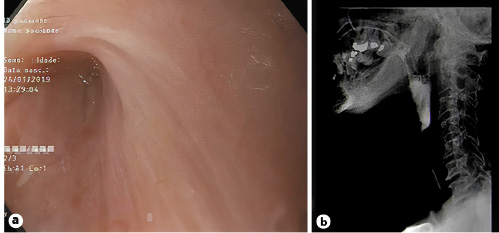
A 61-year-old female patient presented with aphagia 4 years after being submitted to neoadjuvant radiotherapy and laryngectomy for laryngeal squamous cell carcinoma. Upper digestive endoscopy and a barium esophagogram showed a completely obstructed stricture at the pharyngo-esophageal anastomosis, located at 12 cm from the incisors and causing total obliteration of the upper esophagus (Fig. 1). A surgical gastrostomy was performed to provide enteric caloric intake. Over the following 3 years, the patient maintained aphagia and inability to tolerate secretions, with compromised quality of life.
A combined anterograde-retrograde technique for esophageal recanalization was proposed, using two endoscopes: an anterograde endoscope (9.2 mm) and an ultra-slim endoscope (5.4 mm), introduced through the gastrostomy orifice. After the alignment and apposition of the endoscopes, confirmed by transillumination and radioscopy, a 19-gauge needle was anterogradely passed across the stricture, followed by a 0.035-inch hydrophilic guidewire. A proximal through-the-scope balloon dilation was performed in three stages (6, 7, and 8 mm). The retrograde endoscope provided simultaneous direct visualization and stabilization of the devices. An anterograde fully covered biliary metal stent (30 Fr/8 cm) was placed under direct and radioscopic view, allowing maintenance of lumen patency (Fig. 2). The procedure was performed under sedation, and there were no related adverse events. The patient was able to swallow her saliva and partially tolerate liquid diet. Endoscopic evaluation 1 month after the procedure documented a patent esophageal lumen and a properly positioned stent. The stent was removed, illustrating a completely recanalized esophageal lumen (Fig. 3).
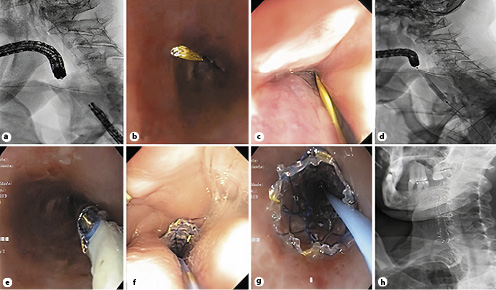
Fig. 2 a Apposition of the endoscopes: radioscopic view. b Retrograde endoscopic view of the inserted guidewire. c Anterograde endoscopic view of the inserted guidewire. d Anterograde through-the-scope balloon dilation: radioscopic view. eStent placement. f Endoscopic anterograde view of the stent. g Endoscopic retrograde view of the stent. h Radioscopic final view of the stent.
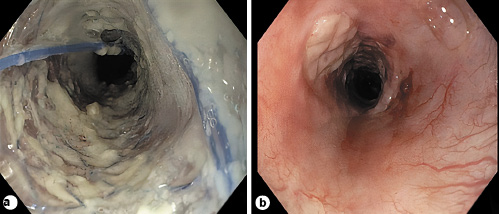
Fig. 3 Endoscopic evaluation after 1 month. a Stent correctly placed. b Esophageal lumen patency following stent removal.
Esophageal strictures are common in patients with head and neck cancers treated with radiation therapy [1]. Although infrequent, a complete lumen obstruction constitutes a therapeutic challenge [1, 2]. Even though only small case series and retrospective studies are currently published, combined anterograde-retrograde recanalization seems to be feasible, with a high technical success rate (89%) and a variable clinical success rate, measured as improvement of dysphagia (58%) and being gastrostomy-tube free (44%), ultimately showing enhanced quality of life [2-5]. Several utensils may be used to gain access through the obstructed lumen, although clear assumptions towards the ideal endoscopic technique cannot be taken [2-4]. Nevertheless, the need for repeated dilations (79%) and related adverse events (perforation 8% and pneumomediastinum 10%) requires a judicious patient selection [5]. Furthermore, the complexity of the procedure limits this technique to experienced endoscopists [5].