Introduction
In December 2019 a new coronavirus (SARS-CoV-2) emerged, responsible for an unprecedented respiratory disease called COVID-19 [1, 2]. This virus rapidly spread worldwide, leading the World Health Organization to declare a pandemic on March 12, 2020 [3]. This pandemic has already caused over one million deaths and brought tremendous suffering and disruption to normal life [4].
In the health system, a large variety of measures were adopted to stop the virus’ dissemination, with the postponement of scheduled surgeries, outpatient clinic appointments, and non-urgent treatments and exams in order to minimize the burden of patients on health care facilities overwhelmed with COVID cases [5]. With the reorganization of the hospitals and primary care centers in response to the pandemic, there was significant concern regarding the possible delay in the diagnosis and treatment of other conditions, including oncologic diseases.
Cancer patients represent a priority population in terms of accessibility to health resources since, if left without treatment and adequate surveillance, the prognosis can be fatal. At our hospital, we hold a weekly multidisciplinary digestive oncology reunion (DOR) to discuss the digestive oncologic patients, both initial digestive cancer diagnoses and follow-up patients, in which we define the optimal course of action for each one. This multidisciplinary reunion includes gastroenterologists, surgeons, oncologists, radiotherapists, radiologists, pathologists, palliative care professionals, and nutritionists, in order to provide the best and fastest care for these patients. The present study aimed to assess the impact of the CO VID-19 pandemic on the diagnosis, treatment, and outcome of patients with digestive cancer managed at our hospital.
Materials and Methods
Every week, during our hospital’s DOR, we perform several clinical discussions of patients with digestive cancer, including first time clinical discussion of patients with an inaugural digestive cancer diagnosis, as well as discussion of follow-up patients. The follow-up clinical discussions include patients who lacked diagnostic exams in the first clinical discussion, patients who underwent neoadjuvant therapy and need to be referred to surgery, patients who underwent surgery and require adjuvant therapy, and patients with disease progression who need to be referred to palliative care. Also, whenever there is a general patient status or tumor staging alteration, we perform another clinical discussion to adjust the optimal management option.
The authors performed a retrospective analysis of patients with an inaugural digestive cancer diagnosis, discussed for the first time in our weekly DOR, from March to August of 2020 (study group) and from the same period of 2018 (control group). The exclusion criteria were: age under 18 years, and a previous digestive cancer diagnosis/discussion in the DOR.
The following clinical data was collected for each patient from the hospital database: age, gender, referral origin, tumor site and staging at diagnosis, time from diagnosis to first DOR discussion, treatment(s), time from DOR to the beginning of treatment, elective versus urgent surgery, and outcome.
Statistical analysis was performed using the Statistical Package for Social Sciences (IBM SPSS® Statistics, version 25.0). Categorical variables are presented as frequencies and percentages and continuous variables as means and SD, or medians and interquartile ranges for variables with skewed distributions. Normal distributions were checked using the Shapiro-Wilk test or skewness and kurtosis. A parametric Independent t test was used to compare normally distributed variables. The χ2 test was used for categorical variables. The Kaplan-Meier curve was used to compare 30-day mortality between the groups. All reported p values are 2-tailed, with a p value <0.05 indicating statistical significance.
Results
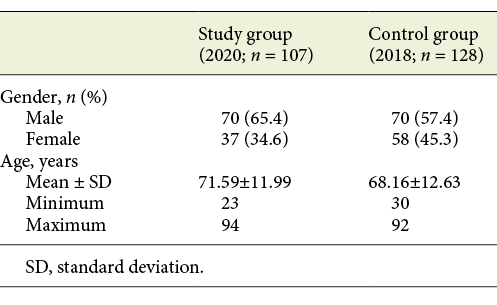
A total of 235 patients were included: 107 in the study group and 128 in the control group. In the study group, 70 (65.4%) were males and 37 (34.6%) were females, aged between 23 and 94 years (mean age 71.59 ± 11.99). In the control group, 70 (54.7%) were males and 58 (45.3%) were females, aged between 30 and 92 years (mean age 68.16 ± 12.63). The characteristics of the study population are presented in Table 1.
In total, we performed more clinical discussions during our hospital DOR in 2018 compared to 2020 (total of 355 clinical discussions in 2018 vs. 256 in 2020), with a higher mean of clinical discussions per week in 2018 (13.65 vs. 10.67, p = 0.040). Nevertheless, there was no statistically significant difference in the mean number of first clinical discussions for patients with an inaugural digestive cancer diagnosis in DOR between both periods (p = 0.670). The distribution of total clinical DOR discussions and first clinical discussions for patients with an inaugural digestive cancer diagnosis in both groups is illustrated in Figure 1.
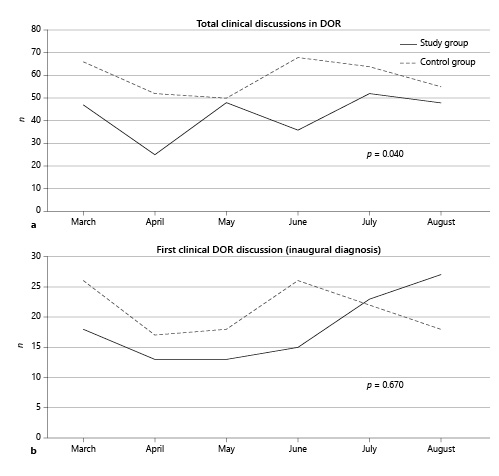
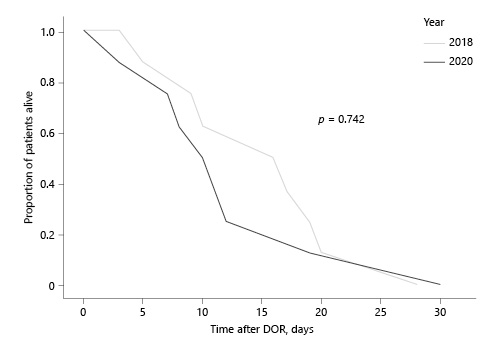
Fig. 1 a Distribution of total clinical DOR discussions in both groups. b Distribution of first clinical discussions for patients with an inaugural digestive cancer diagnosis in both groups.
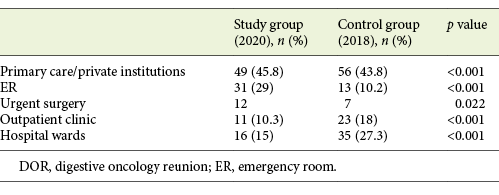
Most patients were referred to DOR from primary care/private institutions in both groups (45.8% in the study group and 43.8% in the control group). More patients were referred from the emergency room (ER) in 2020 (29 vs. 10.2%) and fewer from the outpatient clinic (10.3 vs. 18%) and hospital wards (15 vs. 27.3%; p < 0.001). Furthermore, a higher number of patients were referred to DOR after urgent surgery in the study group (12 vs. 7; p = 0.022). The origin of referral for both groups is presented in Table 2.
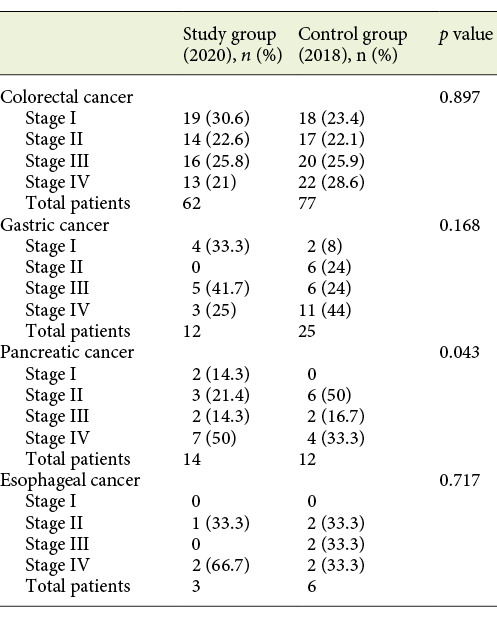
No statistically significant difference was found when comparing the mean wait from diagnosis until the first DOR discussion in both groups (mean 29.52 days in 2018 vs. 41.21 days in 2020; p = 0.087). Tumor staging at the time of diagnosis for colorectal, gastric, and esophageal cancer was not statistically significant different between the groups (p = 0897, p = 0.168, and p = 0.717, respectively). Regarding pancreatic cancer, a higher number of patients in the study group presented with stage IV at the time of diagnosis, compared to the control group, in which 50% of patients presented with stage II pancreatic cancer at diagnosis (p = 0.043). The distribution of the different tumor stages at diagnosis of the most prevalent tumor sites in both groups, and respective p values, are presented in Table 3.
Table 3 Distribution of tumor stages at diagnosis of the most prevalent tumor sites in both groups, and respective p values
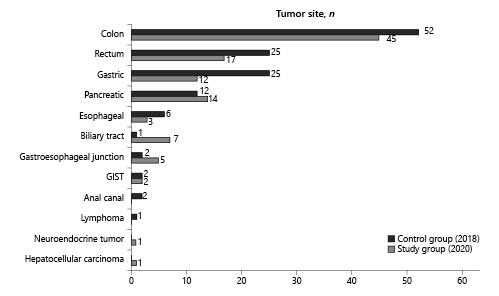
Colon cancer was the most frequent neoplasia in both groups (42.1% [n = 45] in the study group and 40.6% [n = 52] in the control group), followed by rectal cancer (15.9% [n = 17] and 19.5% [n = 25], respectively). The distribution of tumor sites in both groups is presented in Figure 2.
After a first DOR discussion, the team decided on a curative treatment plan in 64 (59.8%) patients in 2020 and 82 (64.6%) patients in 2018, whereas 43 patients in 2020 and 45 patients in 2018 were referred for best palliative care. No statistically significant difference was found between both groups considering the proportions of curative and palliative care (p = 0.455).
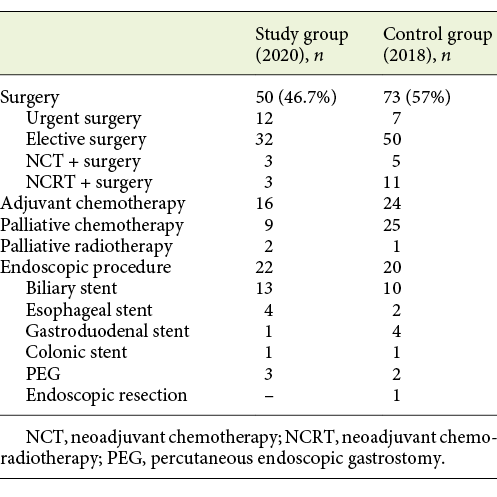
Regarding treatment in the study group: 50 patients (46.7%) underwent surgery (12 urgent surgery), 3 of which were after neoadjuvant chemotherapy (NCT) and 3 after neoadjuvant chemoradiotherapy (NCRT). In most patients (84%) the resection margins were tumor free. Sixteen patients (15%) required adjuvant chemotherapy (ACT). Nine patients (8.4%) underwent palliative chemotherapy (PCT) and 2 (1.9%) palliative radiotherapy (PRT). Twenty-two patients (20.6%) underwent palliative endoscopic procedures. As for the control group, 73 patients (57%) underwent surgery (7 urgent surgery), 11 of which were after NCRT and 5 after NCT. Also, in most patients (83.6%) the resection margins were R0. Twenty-four patients (18.9%) required ACT; 25 patients (19.7%) underwent PCT and 1 (0.8%) PRT. Twenty patients (15.7%) underwent palliative endoscopic procedures. The treatments in both groups are described in Table 4.
No statistically significant difference was found in the mean period from first DOR discussion until first treatment of NCT (48.86 days in the study group vs. 57.59 days in the control group, p = 0.680). Also, no statistically significant difference was found in the mean period from first DOR until elective surgery (60.81 days in the study group vs. 79.45 days in the control group, p = 0.198). Also, there was no statistically significant difference in the time from surgery until ACT (55 days in the study group and 55.7 days in the control group, p = 0.396).
Eight patients died within 30 days from the first DOR discussion in 2018 and 8 patients died in the same period in 2020. The 30-day mortality rate was 6.25% in the control group and 7.48% in the study group. There was no statistically significant difference in survival between the groups (p = 0.742). Figure 3 illustrates the survival distribution in both groups.
Discussion
Cancer patients represent a particular population since, from diagnosis, treatment should be initiated as soon as possible due to the risk of disease progression and a poor clinical outcome in most cases. This group of patients frequently need to visit the hospital for treatment and disease surveillance, thus representing a priority to the health care institutions. With the COVID-19 pandemic, health care facilities around the world had to make tremendous efforts and changes to accommodate and treat COVID-19 patients, while attempting to maintain the best support to other non-COVID patients and guaranteeing everyone’s safety [6]. At the end of August in Portugal, there were over 14,000 active cases of SARS-CoV-2 infection and over 1,800 deaths due to COVID-19 disease, with a total of 58,000 confirmed cases since March. To the best of our knowledge, there are no national studies regarding the true impact of the COVID-19 pandemic on the diagnosis, treatment, and outcome of cancer patients in general, and particularly in digestive cancer patients.
Colorectal cancer (CC), the most frequent cancer type in our study population, is a very prevalent cancer worldwide [7]. Screening and prevention programs are of utmost importance to reduce the burden of this condition. In Portugal, prevention of CC greatly relies on primary care centers which alert adult patients, mostly over 50 years old, to undergo screening (either through colonoscopy or occult blood stool samples), and hospitals/private institutions that perform the endoscopic examinations.
On March 18, 2020 a state of emergency was declared in Portugal, leading the health care systems to prioritize urgent visits and delay elective care in primary care institutions, hospitals, and private practices, to mitigate the spread of COVID-19 in health care settings. Private practices in Portugal are responsible for the majority of screening exams. When the state of emergency was declared, they had to suspend non-urgent procedures, at least until this state was lifted. Also, according to the European Society of Gastrointestinal Endoscopy [8], at the beginning of the pandemic outbreak, it was recommended that endoscopic exams should only be performed in urgent or emergent situations. Therefore, non-urgent exams, such as screenings, were delayed. In April 2020, activities slowly began to return to normal, although with several hygienic measures to prevent virus spread.
The present study aimed to assess the impact of the COVID-19 pandemic in the diagnosis, treatment, and outcome of patients with digestive cancer referred to or diagnosed at our center. The total number of clinical discussions in our hospital’s weekly DOR was significantly lower in the pandemic era, although the number of first clinical discussions for patients with an inaugural digestive cancer diagnosis was not significantly different. In the study group, similarly to the control group, a large percentage of patients discussed at the DOR were referred from primary care/private institutions, reinforcing at least some priority attendance to confirmed/suspected cancer patients. However, more patients were referred from the ER in the pandemic era, probably in relation with an impaired health system response to elective diagnostic exams, and for some fear and delay among patients in seeking medical attention. In fact, a study in the USA showed a reduced ER incidence in some acute life-threatening conditions after the state of emergency declaration, which might be explained by many pandemic-related factors, including fear of exposure to COVID-19, unintended consequences of public health recommendations to minimize non-urgent health care, or stay-at-home orders [9]. In the study group, more CC patients were submitted to urgent surgery due to malignant colorectal obstruction compared with the control group, probably reflecting the delayed diagnosis in these patients.
Regarding the time of DOR discussion, the patients in the study group were not significantly delayed by the COVID-19 pandemic. However, the mean waiting time from diagnosis until first DOR discussion came close to statistical significance, which may be due to a relatively small sample size in the present study.
Tumor staging at the time of diagnosis was not significantly different for colorectal, gastric, or esophageal cancer. However, there was a statistically significant difference regarding the tumor staging of pancreatic cancer, this having been diagnosed at a later stage in the study group, probably reflecting a reduced amount/delay in diagnostic exams performed during the COVID-19 pandemic era. Tumor staging at diagnosis for the residual tumor sites could not be adequately compared between the groups due to the small sample size. The treatment course of digestive cancer patients in our center was not significantly delayed compared to the non-pandemic period, reflecting the maintenance in quality of care to this priority subset of patients.
The COVID-19 pandemic had a negative impact on the total number of patients discussed at our center’s DOR, but did not affect the number of patients with an inaugural digestive cancer diagnosis discussed for the first time during our DOR. More patients were referred to DOR from the ER in the pandemic era, with more patients being referred after urgent surgery, and less from outpatient clinic/hospital wards. The patients in the study group were not significantly affected by the COVID-19 pandemic regarding timely DOR discussion, beginning of treatment, or 30-day mortality, again reflecting the maintenance in quality of care to this priority subset of patients.
There is a lot of uncertainty regarding the second wave of COVID-19. The numbers of new infections are rising every day, and the number of patients requiring hospitalization is higher than in the first outbreak. The health services are warning about the imminent collapse of hospitals, tiredness of the health care professionals, and the increasing number of in-hospital COVID-19 cases. Maintaining the best care for non-COVID patients during the next COVID-19 waves will be an enormous challenge.