Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.27 no.6 Lisboa dez. 2020
https://doi.org/10.1159/000507201
CLINICAL CASE STUDY
Fibrolamellar Carcinoma: A Multimodal Approach
Carcinoma fibrolamelar: uma abordagem multimodal
João Vasco Barreiraa, Nádia Silvab, Anuraj Parmanandea, Manuel Rochac, João S. Coelhob, Hugo Pinto Marquesb, Ricardo da Luza
aMedical Oncology Department, Centro Hospitalar Universitário Lisboa Central, Lisbon, Portugal; bGeneral Surgery Department, Centro Hospitalar Universitário Lisboa Central, Lisbon, Portugal; cGastroenterology Department, Centro Hospitalar Universitário Lisboa Central, Lisbon, Portugal
* Corresponding author.
ABSTRACT
Fibrolamellar carcinoma is a rare variant of hepatocellular carcinoma not associated with cirrhosis or viral hepatitis. Serum alpha-fetoprotein levels are usually normal; the histology is of a well-differentiated tumor, and the staging is the same as for hepatocellular carcinoma. We describe the case of a female patient in her 4th decade of life with a diagnosis of fibrolamellar hepatocellular carcinoma with a multimodal approach. The rare incidence of this cancer and its unusual clinical presentation justifies reporting this case and highlights the importance of multidisciplinary teams in the treatment of cancer patients.
Keywords: Oncology,Fibrolamellar carcinoma, Rare tumors
RESUMO
O Carcinoma fibrolamelar é uma variante rara de hepatocarcinoma, não associado a cirrose ou hepatites virais. Os níveis séricos de alfafetoproteína são geralmente normais; A histologia é de um tumor bem diferenciado e o estadiamento é o mesmo do hepatocarcinoma. Descrevese o caso clínico de um doente do sexo feminino, na sua 4a década de vida com diagnóstico de Hepatocarcinoma fibrolamelar com abordagem multimodal. A rara incidência desta neoplasia e a sua apresentação clínica incomum justificam a notificação deste caso e destacam a importância de equipas multidisciplinares no tratamento dos doentes oncológicos.
Palavras-Chave: Oncologia, Carcinoma fibrolamelar, Tumores raros
Introduction
Fibrolamellar carcinoma is a rare and distinct form of liver cancer, which differs from hepatocellular carcinoma in several peculiarities, including demography, risk factors, tumor markers, and possibly prognosis. It occurs equally in males and females, being more common in children and young adults. Inaugural symptoms are usually nonspecific. Diagnosis is typically made based on clinical and imaging presentation; negative alpha-fetoprotein may support the diagnosis in a patient with suggestive radiological findings. The histological result is considered the gold standard to confirm the diagnosis. The most important prognostic factors are disease stage and resectability. Surgical resection with complete lymphadenectomy represents the best longterm survival hypothesis. Approximately 20–25% of the patients have categorically unresectable disease, which is associated with a 5-year survival rate of 0–5% and an average 12-month survival [1]. The best therapeutic sequence in these patients is not established, and there are no guidelines [2]. The role of liver transplantation is controversial and can be considered in selected patients without extrahepatic metastases. Systemic therapy is an appropriate option for patients with unresectable tumors, but the choice of regimen is empirical. There is a case report of a sustained complete response with gemcitabine and oxaliplatin (GEMOX) [3]. Locoregional techniques, such as hepatic artery chemoembolization or microwave ablation, have been used as an alternative approach for non-resection and/or transplant patients or those who do not respond or do not tolerate systemic therapy.
Historically classified as a subtype of hepatocellular carcinoma, fibrolamellar carcinoma has a unique molecular presentation. At the genomic level, it contains a single 400- kb deletion in chromosome 19, leading to a functional DNAJB1-PRKACA fusion protein. Honeyman et al. [4] identified this chimeric transcript that is expressed uniquely in fibrolamellar carcinoma. Some patients lack the classical histological features or display a “mixed” histology, a rare liver tumor defined by the presence of features from both hepatocellular carcinoma and fibrolamellar carcinoma. In these rare tumors, the DNAJB1-PRKACA fusion transcript is expressed at high levels, therefore indicating that mixed fibrolamellar hepatocellular carcinoma is similar to pure fibrolamellar carcinoma at the genomic level [5]. Despite its high penetrance and apparent specificity, the oncogenic role of this fusion event remains unclear.
Case Presentation
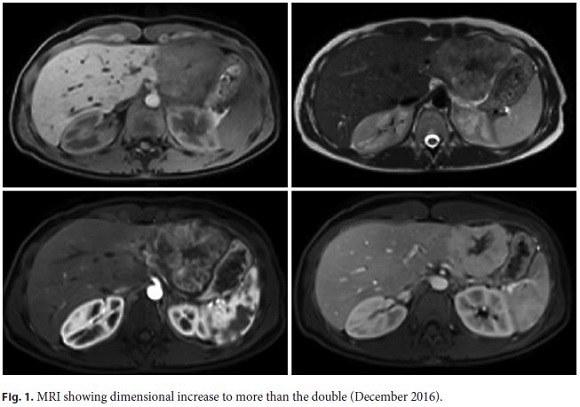
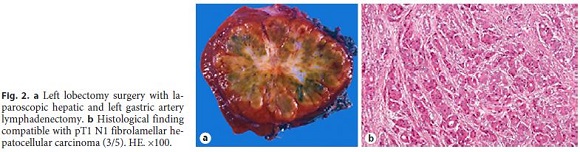
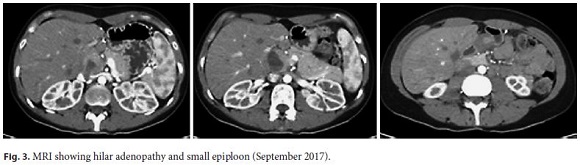
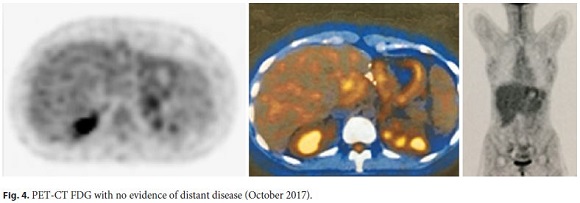
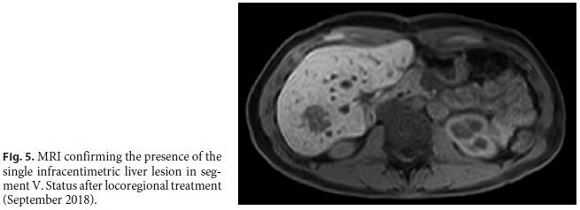
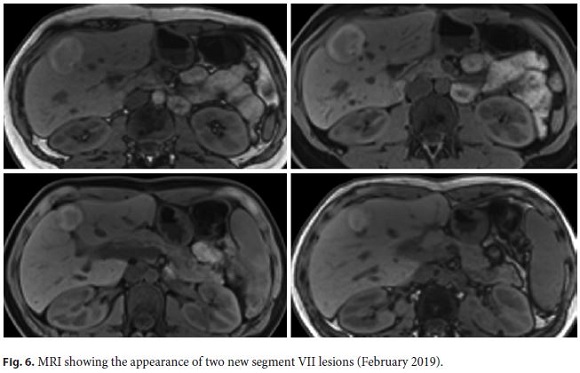
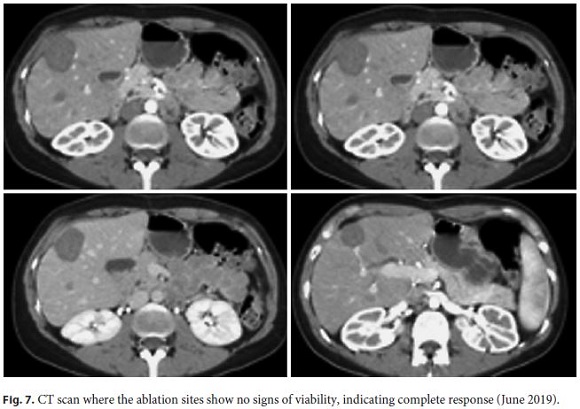
The authors describe a case with unusual presentation in a peculiar clinical context: a female patient in her 4th decade of life with no comorbidities who resorted to the emergency department for a condition of epigastric and left thoracalgia in June 2013, with negative physical examination. Of the complementary examinations, we highlight abdominal ultrasound with a 5-cm hyperechogenic nodule in the left lobe, to be clarified. The analytical assessment proved innocent. On the follow-up assessment in December 2016, the lesion was increased to 6.5 cm (Fig. 1). At the multidisciplinary evaluation, she was proposed for biopsy; however, the pre-biopsy ultrasound revealed an important arterial component, and the examination was canceled. The patient underwent hepatic lobectomy and left hepatic gastric artery and lymphadenectomy after performing a positron emission tomography-computed tomography (PET-CT) scan that showed no distant sign of disease. The histopathological report revealed fibrolamellar hepatocellular carcinoma pT1N1 (Fig. 2). In September 2017, the patient showed hepatic and small epiploon adenopathies on MRI (Fig. 3). After performing a PET-CT scan (Fig. 4) that showed no distant sign of disease, the patient underwent extensive surgical lymphadenectomy. This revealed multiple ganglion metastases (7/14). In February 2018, after a new TC scan, the patient presented a peritoneal nodule, suggestive of carcinomatosis. At this time, the team opted for systemic treatment with a platinum doublet chemotherapy (GEMOX). After 6 cycles (July 2018), the patient presented with out target organ complaints, and imagologically with disappearance (complete response) of the peritoneal nodule and a de novo liver lesion in segment V with 1 cm of diameter. Complete MRI study (September 2018) confirmed the presence of the single infracentimetric liver injury in segment V. In December 2018, she underwent microwave ablation of the aforementioned lesion (Fig. 5). Follow-up at 2 months (February 2019) revealed appearance of two new segment VII lesions (Fig. 6). Accordingly, the patient underwent percutaneous microwave ablation of the metastatic lesions in May 2019. On a control CT scan (June 2019), the ablation sites showed no signs of viability, which made us assume complete response (Fig. 7). The patient currently maintains follow-up with imaging, analytical, and clinical evaluation every 3 months, being asymptomatic (ECOG PS 0), and with no evidence of active oncologic disease.
Discussion and Conclusion
Fibrolamellar carcinoma accounts for 1% of all liver carcinomas and typically presents in young patients with no history of liver disease and normal alpha-fetoprotein levels. Treatment differs from conventional hepatocellular carcinoma, with surgery playing a central role in this entity. There are no clinical trials supporting the benefit of one systemic therapy over another, so the choice of regimen is empirical. Despite the rapid progress in the past years, there are still many critical unresolved questions in fibrolamellar carcinoma. It has immerged as a distinct molecular entity driven by a novel DNAJB1-PRKACA fusion protein that now serves as the main focus of therapeutic outcomes that can be translated to the clinic.
References
1 Eggert T, McGlynn KA, Duffy A, Manns MP, Greten TF, Altekruse SF. Fibrolamellar hepatocellular carcinoma in the USA, 2000-2010: A detailed report on frequency, treatment and outcome based on the Surveillance, Epidemiology, and End Results database. United European Gastroenterol J. 2013 Oct;1(5):351–7.
2 Chapuy CI, Sahai I, Sharma R, Zhu AX, Kozyreva ON. Hyperammonemic Encephalopathy Associated With Fibrolamellar Hepatocellular Carcinoma: Case Report, Literature Review, and Proposed Treatment Algorithm. Oncologist. 2016 Apr;21(4):514–20.
3 Gras P, Truant S, Boige V, Ladrat L, Rougier P, Pruvot FR, et al. Prolonged Complete Response after GEMOX Chemotherapy in a Patient with Advanced Fibrolamellar Hepatocellular Carcinoma. Case Rep Oncol. 2012 Jan;5(1):169–72.
4 Honeyman JN, Simon EP, Robine N, Chiaroni-Clarke R, Darcy DG, Lim II, et al. Detection of a recurrent DNAJB1-PRKACA chimeric transcript in fibrolamellar hepatocellular carcinoma. Science. 2014 Feb;343(6174):1010–4.
5 Griffith OL, Griffith M, Krysiak K, Magrini V, Ramu A, Skidmore ZL, et al. A genomic case study of mixed fibrolamellar hepatocellular carcinoma. Ann Oncol. 2016 Jun;27(6):1148–54.
Statement of Ethics
The authors confirm that written patient consent and permission to publish have been obtained.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors did not receive a specific grant for this research from any funding agency in the public, commercial, or not-forprofit sectors.
* Corresponding author.
João Vasco Barreira, Medical Oncology Department
Centro Hospitalar Universitário Lisboa Central
Alameda Santo António dos Capuchos, Serviço Oncologia Médica
PT–1169-050 Lisbon (Portugal)
Received: October 7, 2019; Accepted: February 15, 2020
Author Contributions
J.V.B., N.S., and A.P. conceived the idea, developed, and took the lead in writing the manuscript. M.R. provided critical feedback and helped shape the manuscript. J.S.C.; H.P.M; R.L. supervised the work. All authors discussed the results and contributed to the final manuscript.
João Vasco Barreira, Nádia Silva, and Anuraj Parmanande are joint first authors














