Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
GE-Portuguese Journal of Gastroenterology
Print version ISSN 2341-4545
GE Port J Gastroenterol vol.27 no.5 Lisboa Oct. 2020
https://doi.org/10.1159/000505034
CLINICAL CASE STUDY
Esophageal Mucosal Bridge of Unknown Etiology Causing Dysphagia in an Elderly Female: Endoscopic Management and Literature Review
Ponte mucosa esofágica de etiologia desconhecida como causa de disfagia numa mulher idosa: Orientação endoscópica e revisão da literatura
Prasanta Debnath, Suhas Udgirkar, Pravin Rathi, Shubham Jain, Sujit Nair, Vinay Pawar, Qais Contractor
Department of Gastroenterology, T.N.M.C. and B.Y.L. Nair Charitable Hospital, Mumbai, India
* Corresponding author.
ABSTRACT
Esophageal mucosal bridge is an elastic stretchable structure,connecting across the lumen, extending either obliquelyor horizontally, more commonly seen in the mid or loweresophagus. It can be either congenital or secondary (acquired).Acquired ones are secondary to reflux esophagitis,corrosive esophageal injury, drug-induced esophagitis, radiationesophagitis, Crohn’s disease, Mallory-Weiss syndrome,malignant tumors, and infections like candidiasis,HSV, CMV, or tuberculosis. We present a case of an elderlyfemale, who presented with progressive dysphagia for 3months, more commonly to solids without any history of anorexiaor weight loss. No history of corrosive ingestion, radiationexposure, or prior history of any surgical or endoscopicintervention was present. Upper gastrointestinal endoscopyrevealed esophageal mucosal bridge at 20 and 25cm from incisors and mucosal tag. Endoscopic resection wascarried out successfully with hot biopsy forceps and needleknife after prophylactic application of hemoclips at two endsof each bridge, without any adverse event. Esophageal mucosalbridge, though rarely reported, should be kept in thedifferential diagnosis of patients presenting with dysphagia.Endoscopic resection with hot biopsy forceps or needle knifeseems to be effective.
Keywords: Esophagus, Mucosal bridge, Dysphagia, Endoscopy
RESUMO
Uma ponte mucosa esofágica é uma estrutura elástica que se estende obliquamente ou horizontalmente através do lúmen esofágico, sendo a sua posição mais comum no esófago médio ou distal. Pode ser congénita ou secundária (adquirida).Estas geralmente são secundárias a esofagite de refluxo, lesão corrosiva, medicamentosa, rádica, doença de Crohn, síndroma de Mallory-Weiss, tumores malignos ou por infeções como candidíase, HSV, CMV ou tuberculose. Apresentamos um caso de uma mulher idosa com disfagia progressiva com 3 meses duração, mais para sólidos, sem história de anorexia ou emagrecimento, sem história de ingestão de caústicos, radioterapia, cirurgia ou qualquer intervenção endoscópica prévia. A endoscopia digestiva alta revelou uma ponte mucosa aos 20 e 25 cm dos incisivos e uma prega mucosa. Procedeu-se a resseção endoscópica com pinça de hot-biopsy e com needle-knife após colocação profilática de hemoclips em ambas as extremidades de cada ponte, com sucesso e sem qualquer efeito adverso. Apesar de raramente reportadas as pontes mucosa esofágicas devem ser consideradas no diagnóstico diferencial de doentes com disfagia. A resseção endoscópica com pinça de hot-biopsy ou needle-knife parece ser eficaz nestes casos.
Palavras-Chave: Esófago, Ponte mucosa, Disfagia, Endoscopia
Introduction
Mucosal bridges have been infrequently reported in the upper gastrointestinal tract [1–3]. Endoscopically, they appear as cord-like mucosal connections across the lumen, looking very much like a bridge. They are elastic stretchable structures that may be seen in any site from the esophagus to the colon. The esophageal mucosal bridge may extend obliquely or horizontally across the lumen and commonly occurs in the mid and lower esophagus [4]. However, cases of proximal esophageal mucosal bridge have been reported as congenital malformation in infancy, and involvement of distal esophagus is incriminated to gastroesophageal reflux [5–7]. Clinically, symptoms vary greatly depending on their location, and occasionally a patient may be asymptomatic [8].
The first case of esophageal mucosal bridge was reported by Dafoe and Ross in 1969 [9]. Since then, multiple such cases have been reported. An esophageal mucosal bridge can be either congenital or acquired; cases of unknown etiology are usually designated as congenital. Among acquired cases of mucosal bridge, common ones are secondary to reflux esophagitis, post-variceal sclerotherapy, corrosive esophageal injury, drug-induced esophagitis, radiation esophagitis, submucosal dissection (hematoma), Crohn’s disease, systemic lupus erythematosus, Mallory-Weiss syndrome, malignant tumors, and infectious causes like candidiasis, HSV, CMV, or tuberculosis [1, 10–13]. Rare cases of esophageal mucosal bridge formation secondary to injury by naso-enteric tube have been reported [14]. Though mucosal bridge and coexistent esophageal carcinoma have been reported, their cause-effect relationship is yet to be established.
We, hereby present a case of multiple esophageal mucosal bridges in an elderly female presenting with recent onset dysphagia, in whom no underlying precipitating factor was present.
Case Report
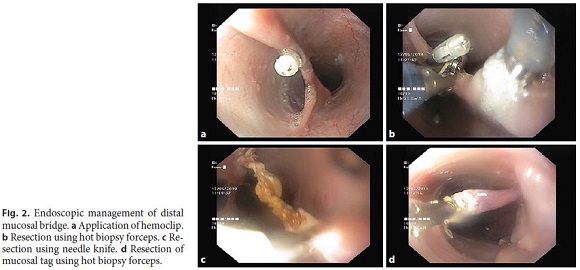
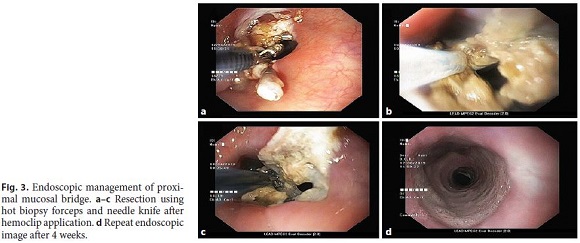
An 88-year-old female presented with progressive dysphagia predominantly for solids, lasting for 3 months. It was associated with intermittent regurgitation, non-productive cough, and dyspnea on exertion for 2 months. The patient had no retrosternal burning, abdominal pain, bloating, or eructation at present or in the past. Bowel habits were normal, and the patient denied any history of anorexia or weight loss. There was no past history of corrosive ingestion, radiation exposure, alcohol abuse, any surgical or endoscopic intervention. Routine laboratory investigations were normal; HIV (ELISA) was negative. CT of the thorax with oral contrast showed a smooth circumferential thickening of the esophagus, measuring 6.1 mm just above the arching of the azygos vein over the right main bronchus with a length of 2.3 cm, with a small suspicious filling defect in the proximal esophagus at the level of T2 vertebra, suspicious of a mucosal polyp. Upper gastrointestinal endoscopy documented an esophageal mucosal bridge at 20 cm from the incisors, with a long septum of 1.8 cm (Fig. 1a). Another mucosal bridge was observed at 25 cm with a mucosal tag seen just proximal to it; the rest of the esophagus and stomach were normal (Fig. 1b). Endoscopic resection was considered as the patient was symptomatic. The distal lesion was targeted first. Hemostatic clips (Olympus Quick Clip ProTM) were first placed at either end of the bridge, to prevent bleeding from the resection (Fig. 2a). A hot biopsy forceps (Olympus EndoJaw Hot with oval fenestrated alligator cups) was used for resection of the bridge with intermittent short bursts of electrocautery current using Endocut® Q mode (ERBE Elektromedizin GmbH) Fig. 2b). Fusion® needle knife (Cook Medical Inc., Winston-Salem, NC, USA) was also used for resection of the bridge (Fig. 2c). The mucosal tag just proximal to the distal bridge was resected with hot biopsy forceps and was sent for histopathological examination (Fig. 2d). The proximal mucosal bridge, similar to the distal one, was resected in two sittings because of the long septum. At first, hemostatic clips were applied at both ends (Fig. 3a), and resection was done using both hot biopsy forceps (Fig. 3b, c) and needle knife (Fig. 3d). The procedure was tolerated well, and there were no post-procedure complications. Though the patient complained of mild throat discomfort in the immediate post-procedure period, it subsided within 3 days. Normal stratified squamous epithelium without any inflammatory cells was reported on histopathology. After 4 weeks, the patient was asymptomatic, and follow-up endoscopy revealed normal-appearing esophageal mucosa.

Discussion
Esophageal mucosal bridge has been reported in the literature, but epidemiologic data are not available as it is rare and occasionally asymptomatic. It has been frequently reported as an incidental finding on endoscopy [4]. The pathogenesis of mucosal bridge in the esophagus is not well established. Esophageal inflammation has been incriminated for various reasons [15]. It is a sequela to the healing process of the esophageal mucosal lesion. In inflammatory bowel disease, mucosal bridges in the colon are formed when inflammatory pseudopolyps attach their ulcerated ends and the overlying mucosa gets reepithelialized [16]. Similarly, when the walls of inflamed esophagus come into contact with each other, the underlying granulation tissue of each wall develops adhesions, leading to the formation of mucosal bridges [17].
Another theory proposes ulceration as the root cause. Normally, the esophagus remains collapsed in the anterior- posterior diameter, so that the anterior and posterior walls become apposed. Thus, healing of an ulcer by reepithelialization of the mucosal undersurface leads to the subsequent formation of a mucosal tube attached at each end to the non-ulcerated bowel wall [18].
Our patient did not have any of the risk factors that have been mentioned in the literature so far. So, considering the age of our patient, an idiopathic cause was assumed. Moreover, to the best of our knowledge, this is the first reported case of multiple esophageal bridges in the same patient, who was managed successfully by endoscopic resection. Other congenital disorders like esophageal duplication can be either cystic, tubular, or diverticular type. Cystic type, the most common one, is identified more commonly in asymptomatic patients, manifesting as a mediastinal mass in radiographs or submucosal lesion on endoscopy. Tubular type is usually located within the esophageal wall, parallels the lumen, and communicates with the true lumen at either or both ends of the tube. But they present in infancy with chest pain or dysphagia, and reconstructive surgery is required for symptomatic patients [19].
Symptoms in cases of an esophageal mucosal bridge can be variable, ranging from a long asymptomatic period to a symptomatic phase leading to dysphagia, chest pain, odynophagia, intermittent episodes of bleeding, and weight loss [20]. Our patient had classical symptoms of mechanical dysphagia without any history of anorexia and weight loss.
Treatment modality has evolved dramatically in the recent past. Endoscopic intervention has become the first-line treatment in this group of patients. Argon plasma coagulation is safe and efficacious in several cases [21]. Electrosurgical intervention using hot biopsy forceps and needle knife after prior application of hemoclips at both ends of the bridge has also been used successfully in many cases [20, 22]. No data exist regarding the safety or superiority of one method over the other. We performed endoscopic resection using hemoclips, hot biopsy forceps, and needle knife successfully in our patient without any adverse effects. Thus, esophageal mucosal bridge, though rarely reported, must be considered in the differential diagnosis of mechanical dysphagia, and endoscopic therapy is an attractive option for its management.
References
1 Obrador A, Gayà J. Antral mucosal bridge. Gastrointest Endosc. 1986 Jun;32(3):215–7.
2 Mai M, Watanabe K. Multiple mucosal bridge formations in the stomach, report of a case. Endoscopy. 1985 Jan;17(1):40–1.
3 Papazian A, Capron JP, Ducroix JP, Dupas JL, Quenum C, Besson P. Mucosal bridges of the upper esophagus after radiotherapy for Hodgkin’s disease. Gastroenterology. 1983 May;84(5 Pt 1):1028–31.
4 Saha AK, Kundu AK. Mucosal bridge in oesophagus. J Assoc Physicians India. 2014 Aug;62(8):704–5.
5 Buts JP, Otte JB, Fiasse L, Claus D, Maesen Y. Endoscopic treatment of an unusual form of congenital esophageal stenosis. Acta Endosc. 1980;10:407–12.
6 Mihas AA, Slaughter RL, Goldman LN, Hirschowitz BI. Double lumen esophagus due to reflux esophagitis with fibrous septum formation. Gastroenterology 1976 Jul;71(1):136–7.
7 Papazian A, Capron JP, Sevenet F. Mucosal bridges of the distal esophagus related to reflux esophagitis. Gastrointest Endosc. 1984 Jun;30(3):217–8.
8 Sunkara T, Then EO, Yarlagadda KS, Jhaveri M, Gaduputi V. An Innocent Esophageal Mucosal Bridge: Case Report and Literature Review. J Investig Med High Impact Case Rep. 2018 Mar;6:2324709618767204. [ Links ]
9 Takubo K. Pathology of the Oesophagus: An Atlas and Textbook 2008. 2nd ed. Hongkong: Springer, chapter 8, p. 98–108.
10 Kume K, Yoshikawa I. Mucosal bridge due to reflux oesophagitis. Gastroenterology Insights. 2009;1(1 e4):14. [ Links ]
11 Itano T, Tomoda J, Harada H, Uesaka K, Kagawa S, Sugihara T, et al. [A case of systemic lupus erythematosus with esophageal mucosal bridge]. Nihon Shokakibyo Gakkai Zasshi. 1986 Dec;83(12):2598–601. Japanese.
12 Shikiya K, Kinjo N, Akamine K, Kohchi A, Higa M, Ohshiro J, et al. [A case of midesophageal diverticulum with mucosal bridge caused by tuberculosis of the apex of the right lung]. Nihon Shokakibyo Gakkai Zasshi. 1991 Mar;88(3):724–9.
13 Gottfried EB, Goldberg HJ. Mucosal bridge of the distal esophagus after esophageal variceal sclerotherapy. Gastrointest Endosc. 1985 Aug;31(4):267–9.
14 Buchman AL, Waring JP. Mucosal bridge formation in the esophagus caused by injury from a nasoenteric feeding tube. JPEN J Parenter Enteral Nutr. 1994 May-Jun;18(3):278–9.
15 Chang FY, Lai KH, Lee SD, Tsai YT. Asymptomatic mucosal bridge of the upper esophagus. Gastrointest Endosc. 1989 Sep-Oct;35(5):472–3.
16 Fefferman DS, Farrell RJ. Endoscopy in inflammatory bowel disease: indications, surveillance, and use in clinical practice. Clin Gastroenterol Hepatol. 2005 Jan;3(1):11–24.
17 Vazifdar KF, Wagle SD, Dhir V. Multiple mucosal bridges of esophagus: an unusual cause of dysphagia. Indian J Gastroenterol. 1996 Oct;15(4):152. [ Links ]
18 Waye JD. Endoscopy in inflammatory bowel disease. Clin Gastroenterol. 1980 May;9(2):279–96.
19 Berrocal T, Torres I, Gutiérrez J, Prieto C, del Hoyo ML, Lamas M. Congenital anomalies of the upper gastrointestinal tract. Radiographics. 1999 Jul-Aug;19(4):855–72.
20 Ranketi S, Mwachiro M, Topazian M, Burgert S. Endoscopic treatment of cervical esophageal transluminal bridge. Gastrointest Endosc. 2017 Sep;86(3):561–2.
21 Mukherjee M, Oh J, Khdair A, Grosman I. Esophageal mucosal bridges associated with idiopathic esophageal ulcer treated with argon plasma coagulation. Gastrointest Endosc. 2008 Aug;68(2):387–9.
22 Perisetti A, Banerjee D, Tharian B. Endoscopic resection of esophageal mucosal bridge. Gastroenterology. 2018 Jun;154(8):2033–4.
Statement of Ethics
Informed consent for publication of case details was obtained from the patient and her relatives.
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding Sources
The authors have no funding sources to declare.
* Corresponding author.
Dr. Prasanta Debnath
T.N.M.C. and B.Y.L. Nair Charitable Hospital
Room No. 717, 7th Floor, OPD Building, Dr. A.L. Nair Road
Mumbai Central, Mumbai, Maharashtra 400008 (India)
E-Mail prasantad89@gmail.com
Received: June 20, 2019; Accepted after revision: November 26, 2019
Author Contributions
Dr. Prasanta Debnath: case report design and writing of the paper. Dr. Suhas Udgirkar: manuscript editing. Dr. Pravin Rathi: supervisor. Dr. Shubham Jain: keeping records. Dr. Sujit Nair: case report design. Dr. Vinay Pawar: manuscript editing. Dr. Qais Contractor: case report design and manuscript editing.














