Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.3 Lisboa jun. 2019
https://doi.org/10.1159/000494674
REVIEW ARTICLE
Preoperative Enteral Nutrition and Surgical Outcomes in Adults with Crohn’s Disease: A Systematic Review
Nutrição entérica pré-operatória e resultados pósoperatórios em adultos com doença de Crohn: revisão sistemática
Anabela Rochaa,b, Inês Bessac, Paula Lagod, Marisa D. Santosa,b, Júlio Leitee,f, Fernando Castro-Poçasb,d
aGeneral Surgery Service – Digestive Unit, Hospital de Santo António, Centro Hospitalar do Porto, Porto, Portugal; bInstituto de Ciências Biomédicas Abel Salazar (ICBAS), Universidade do Porto, Porto, Portugal; cGeneral Surgery Service – Colorectal Unit, Hospital de São Sebastião, Centro Hospitalar de Entre-o-Douro-e-Vouga, Santa Maria da Feira, Portugal; dGastroenterology Service, Hospital de Santo António, Centro Hospitalar do Porto, Porto, Portugal; eSurgery Service, Hospital Universitário de Coimbra, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal; fFaculdade de Medicina, Universidade de Coimbra, Coimbra, Portugal
* Corresponding author.
ABSTRACT
Background and Aim: Enteral nutrition (EN) is applicable to adult Crohn’s disease (CD) in treating malnutrition and in inducing remission – here as a less effective alternative than corticosteroids. The purpose of this review is to determine whether preoperative EN impacts postoperative complications of adult CD, either by means of nutritional or therapeutic effects. Summary: A systematic review of English written full-text research articles published between January 1990 and November 2017, including adult patients undergoing abdominal surgery for complicated CD after EN, was performed. Four studies out of 22 were selected, all of which institutional, retrospective, case-control cohorts, one classified as “good quality” and three as “poor quality,” as rated by the Newcastle-Ottawa Scale. The application of inclusion and exclusion criteria resulted in a non-intentional absence of studies referring to supplemental EN among those reviewed. The reduced number of heterogeneous eligible studies impeded meta-analysis. In all studies, exclusive EN (EEN) was used and well tolerated, allowing to defer or even avoid surgery altogether, improving patients’ global state. The two studies with the greatest number of patients found preoperative EEN to be an independent factor against infectious and non-infectious complications in 219 patients and against anastomotic leaks or abscesses in 38 patients. Also, in univariate analysis, EEN was found to increase preoperative immunosuppressant-free intervals and to protect against anastomotic dehiscences, intra-abdominal abscesses, surgical wound infections, ileus, stomas, and reoperations in the largest study; in another study it was related to fewer intra-abdominal septic complications. Key Messages: All reviewed studies are retrospective and, consequently, of limited relevance. Nonetheless, all of them call the attention of the scientific community to the potential benefits of preoperative EEN on postoperative outcomes in adult CD, calling for prospective multi-institutional studies and randomized controlled trials.
Keywords: Crohn’s disease, Enteral nutrition, Adults, Surgery, Preoperative, Postoperative, Morbidity, Complications
RESUMO
Introdução e objetivo: No adulto com doença de Crohn (DC) a nutrição entérica (NE) é aplicável como terapêutica da desnutrição ou como alternativa, menos eficaz, aos corticoides, para indução de remissão. O objetivo desta revisão é determinar se a NE pré-operatória tem impacto nas complicações pós-operatórias, seja pelo efeito nutricional seja pelo terapêutico. Sumário: Foi realizada uma revisão sistemática dos artigos de investigação que incluíssem doentes adultos submetidos a cirurgia abdominal por DC complicada, após NE, redigidos em inglês e publicados entre janeiro de 1990 e novembro de 2017. De 22 estudos foram selecionados quatro institucionais e retrospetivos de coorte, um de “fraca qualidade” e três de “pobre qualidade” pela “Newcastle-Ottawa Scale”. Nos estudos revistos foi utilizada NE exclusiva (NEE) já que, não intencionalmente, os estudos com NE suplementar reuniram critérios de exclusão. O pequeno número e a heterogeneidade dos estudos elegíveis impossibilitaram uma meta-análise. A NEE foi utilizada e bem tolerada em todos os estudos, e permitiu melhorar o estado global dos doentes e protelar ou mesmo evitar a cirurgia. Nos dois estudos com maior número de doentes, a NEE pré-operatória foi um fator independente contra deiscências de sutura e abcessos em 219 doentes, e contra complicações infeciosas intra-abdominais em 38. Em análise univariada também se verificou que, no maior estudo, a NEE aumentou o intervalo pré-operatório livre de imunossupressores e foi protetora contra deiscências anastomóticas, abscessos intra-abdominais, infeções da ferida operatória, ileus, estomas e reoperações; noutro estudo menores correlacionou-se com menos complicações infeciosas intra-abdominais. Mensagens-chave: Todos os estudos revistos são retrospetivos e, consequentemente, de relevância limitada. No entanto, todos chamam a atenção da comunidade científica para os potenciais benefícios da NEE pré-operatória nos resultados pós-operatórios dos adultos com DC e para a necessidade de estudos prospetivos multi-institucionais e de ensaios clínicos randomizados.
Palavras-Chave: Doença de Crohn, Nutrição entérica, Adultos, Cirurgia, Pré-operatório, Pós-operatório, Morbilidade, Complicações
Introduction
Up to 50% of Crohn’s disease (CD) patients have been classically described to require surgery within 10 years after diagnosis [1]. More recently, according to a population-based cohort study from Denmark, the 9-year cumulative risk of surgery has been reduced from 50% (1979–1986) to 23.3% (2003–2011), along with an increased use of thiopurines and TNFα inhibitors [2]. The same trend was found in a similar study from Sweden – the risk of surgery at 5 years fell from 65.8% (1963–1975) to 34.6% (1991–2005) [3].
Rates of postoperative complications and stoma creation after abdominal surgery are influenced by a number of factors, both clinical and therapeutic, and vary widely across published series [4, 5]. Intra-abdominal septic complications (IASCs) may reach 50%, the risk factors for which the literature mostly reports therapy with corticosteroids (CSTs), malnutrition, intra-abdominal abscesses, low serum albumin levels, and emergent surgery [6–11].
Among medications used in the treatment of CD, CSTs are the one most consensual risk factor for anastomotic complications and, in some series, for global morbidity [4, 6, 9, 10]. As to purine analogues, there is no evidence they might increase the risk of postoperative complications [9, 11, 12]. Differently, TNFα inhibitors increase infectious and global surgical morbidity [11, 13–15].
In what concerns preoperative malnutrition, undernourished CD patients should receive perioperative nutritional support, as in other pathologies of the digestive tract, even if this requires postponing surgery. The enteric route is preferred, whereas parenteral nutrition (PN) is only indicated when the digestive tract is insufficient or unavailable [16–19]. Whenever the digestive tract does not provide enough calories – in patients who tolerate enteral nutrition (EN) but in insufficient quantities – the use of total or supplementary PN becomes inevitable [16]; operating undernourished patients, with consequent increases in postoperative complications and stomas, is to be avoided. Interestingly, there are some early pioneer studies that have found potential advantages in the application of EN to malnourished patients, in whom they seem to produce better surgical results [20, 21].
Concerning therapy with CSTs, exclusive EN (EEN) has largely substituted prednisolone as first-line remission-inducing therapy for moderate to severe disease flares in children [22, 23]. In striking opposition, the former remain the mainstay of therapy for these situations in adults, in whom they seem more effective over EEN [24–26]. In this age group, the therapeutic value of EN in CD is controversial outside the bounds of malnutrition. It may therefore be advised as remission-inducing therapy in case of refusal or intolerance to CSTs, in mild extensive small bowel disease (here as primary or as adjuvant therapy), and as adjuvant therapy in the undernourished which maintain inflammatory stenosis, despite maximized adequate pharmacological therapy [24, 27–29]. The grade of evidence concerning the superiority of CSTs over EEN in adult patients is, however, of very low quality [24].
The mechanisms by which EEN induces remission of CD are not well established [29]. A number of studies suggest that EN promotes the balancing of mucosal cytokines – by decreasing those which are pro-inflammatory [30, 31], restores mucosal integrity and its barrier function [24, 30, 32], decreases adjacent mesenteric fat inflammation [33, 34], and alters the composition of the intestinal microbiome [35, 36]. It is possible that bowel rest and interruption of exposure to alimentary and some bacterial allergens may be contributing mechanisms [29].
Aim
To determine whether preoperative EN impacts postoperative complications of adult CD, either by means of nutritional or therapeutic effects.
Methods
A systematic review of research articles including the use of preoperative EN in adults with CD submitted to abdominal surgery, from January 1990 to November 2017, was conducted.
An initial search was carried out through PubMed-MEDLINE, ScienceDirect, and Google Scholar. Medical subject headings (MeSH) applied were the following:
− for PubMed-MEDLINE, “Crohn’s disease” AND “surgery” AND “postoperative” AND “complications” AND “adults” AND “preoperative” AND “enteral nutrition” AND “not review”; filters applied were “full text,” “English,” and “humans”;
− for ScienceDirect, “Crohn’s disease” and “enteral nutrition” (Title, abstract, keywords);
− for Google Scholar, “Crohn’s disease and preoperative enteral nutrition and adults.”
Two further searches were conducted:
− upon references of all articles selected as eligible, as result of the initial search;
− of “similar articles” of the two most recent studies of those already selected as eligible.
Methodology respected Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) recommendations [37].
Screening and testing for eligibility were performed upon English written abstracts. A grid was constructed to assess articles for eligibility and select them for inclusion, according to specific inclusion and exclusion criteria.
Inclusion criteria:
− Original clinical research articles wherein preoperative EN was administered to adult CD patients operated on for intestinal complications, as long as EN impact on postoperative complications is discriminated.
− English full-text articles published in peer-reviewed journals, including those published online ahead of print, within the time frame considered.
− Retrospective and prospective studies, whether cohort, case series, case control, or randomized controlled trials, regardless of aims and number of patients.
− Studies concerning adults – patients considered adults by the authors of the study were similarly assumed.
− All formulas, means of administration, and regimens of EN – exclusive or supplemental, as complement to PN or a conventional diet.
− Data referring to each type of nutritional regimen is accordingly discriminated and treated separately from that respecting patients and impact on postoperative morbidity.
− Paucity or even absence of data regarding repercussions of EN on patients’ preoperative state will not be criterion for exclusion.
Exclusion criteria:
− Review articles (both systematic and non-systematic), case reports, comments, letters, and book chapters.
− Abstracts of conferences, oral presentations, and posters presented in meetings.
− Papers concerning children or adolescents or whose authors belonged to pediatric institutions.
− Patient overlap among articles – the article containing the most patients was selected.
− Articles or results referring to the analysis of postoperative recurrence of CD.
− Absence of separate data concerning CD patients as opposed to those with ulcerative, undetermined, and unclassified colitis.
The quality of the studies was rated by awarding stars in each domain following the guidelines of the Newcastle-Ottawa Scale (NOS) [38].
Two authors (A.R. and I.B.) undertook the bibliographic search, independently screened the articles for eligibility, and assessed them thoroughly for inclusion. Discussion took place until consensus was reached whenever accordance was not met initially. Three authors (A.R., I.B., and P.L.) reviewed the included articles.
Results
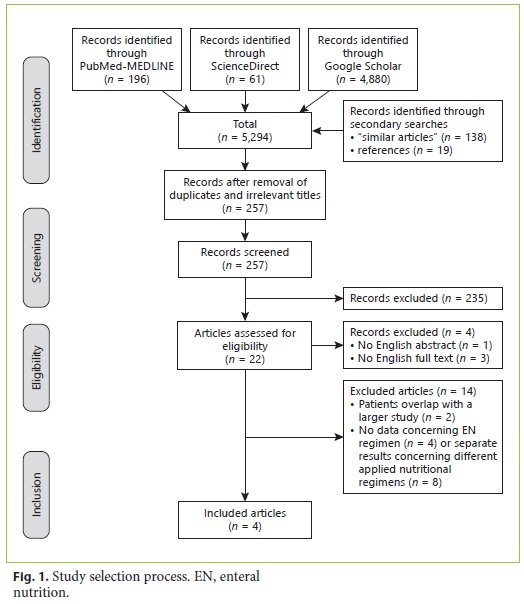
One hundred and ninety-six references were identified in PubMed-MEDLINE, 61 in ScienceDirect, 4,880 in Google Scholar, and 157 through secondary search (Figure 1). After the irrelevant titles and duplicates were removed, 257 records were screened, 22 of which were eligible. Of these, one had no English abstract [39] and three had no English full text [40–42]. The main features of the 14 full-text excluded articles are summarized in Table 1 [43–56] – eight of them had no separate results on different nutritional regimens or on treated patients [44, 47– 50, 52–54] and four had no data on EN regimen [43, 45, 55, 56]; two other articles [46, 51] met the inclusion criteria but overlapped patients with a third study which contained a larger number of patients and was therefore detrimentally included. All studies in which supplemental EN was used with conventional diet or with PN did not meet the inclusion criteria.
The main characteristics of the four articles selected for review [57–60] are summarized in Table 2, Table 3, Table 4, Table 5. Table 2 refers to the general characteristics, aims, methods, indications for and information concerning preoperative EEN regimen, and main conclusions of the articles under review. Table 3 discriminates the characteristics of operated patient groups, the variables studied in each, studies’ limitations, and the NOS quality assessment – criteria for which, as applied to cohort studies, being presented as online supplementary material (for all online suppl. material, see http://www.karger.com/doi/10.1159/000494674)[38]. In Tables 4 and 5, the impact of preoperative EEN on clinical and surgical outcomes is detailed. No mortality was reported. Relevant data from these trials not expressed in the tables will be detailed below.
Li et al. [57] analyzed risk factors for postoperative complications after classifying 708 surgeries into four groups according to patients’ preoperative management (Table 3). EEN was associated with a longer immunosuppressant-free interval and fewer emergent surgeries, primary stomata, anastomotic leaks, intra-abdominal abscesses, wound infections, ileus, and reoperations on univariate analysis (Tables 4, 5). The authors identified EEN as an independent protective factor against postoperative complications (both infectious and non-infectious). Preoperative immunosuppressive therapy, perforation or abscess, emergent surgery, previous surgery for CD, and older age were independent risk factors for infectious complications (Table 5). The first two risk factors and longer operative time were the independent risk factors identified for non-infectious complications. The authors argued that the prospective nature of the database and the cohort nature of this study may have mitigated some of the limitations and biases inherent to retrospective studies.
Heerasing et al. [58] retrospectively revised 51 patients treated with preoperative EEN after nutritional assessment. Thirteen patients (25%) ended up not requiring surgery. For each of the 38 operated EEN patients, two matched non-EEN controls were sought (Table 2). The latter were found to have higher basal body mass index (BMI), lower basal C-reactive protein (CRP) values and lower prevalence of treatment with antibiotics (Table 3). EEN was found to be an independent factor against anastomotic leaks and/or abscesses and led to significantly lower global postoperative morbidity and shorter operative times (Tables 4, 5). Patients with IASCs had signifi cantly longer lengths of hospital stay and a higher readmission rate. The authors point out some limitations to this study such as missing data on medical records and incomplete matching of disease severity. Also, they did not clarify the reasons why control-matched patients did not receive nutritional support – it may even have been due to the baseline differences in BMI and/or serum CRP levels, but this was not mentioned.
Beaupel et al. [59] compared two groups of patients, 21 “low-risk” versus 35 “high-risk” for postoperative complications, distinct regarding CD behavior, severity and complications, nutritional state, and CST treatment (Tables 2, Table 3). As the rate of postoperative complications, for which no protective or risk factors were identified, was not statistically different between the two groups (Table 5), the authors admitted this indicated that TGF-β2enriched EEN was beneficial for high-risk CD patients (Table 2).
In the study published by Zhu et al. [60], 54 of 83 CD patients were treated with EEN for abdominal abscesses not amenable to percutaneous drainage, either until abscess resolution or until surgery (from 7 to 1,000 days). The remaining 29 patients did not tolerate or comply with EEN and had a significantly higher cumulative 1-year surgical rate than EEN patients. EEN led to a higher rate of abscess resolution and was an independent protective factor against surgery. Previous abdominal surgery and abscess diameter > 3 cm were independent risk factors for surgery. Patients’ nutritional status was not mentioned. Forty-six EEN-treated and 28 EEN-untreated patients required surgery, the former having significantly fewer postoperative IASCs (Tables 2, 5). The authors noted limitations to the study beyond its retrospective nature and reduced number of patients: some of the latter suspended EEN and/or restarted immunosuppressants after abscess resolution, for unclarified periods of time.
In all studies, preoperative EEN was well tolerated by adults with complicated CD and a patent intestinal route – 338 out of 1,024 operated patients received preoperative EEN. Compared to their respective controls, patients under preoperative EEN achieved significantly lower levels of preoperative inflammatory markers in three of the reviewed studies [58–60], in two of which with concomitant increases in serum albumin values [59, 60]. The two studies with the greatest number of patients found preoperative EEN to be an independent factor against postoperative infectious and non-infectious complications [57] and against anastomotic leaks or abscesses [58].
However, quality grading for risk of bias according to NOS criteria [38] (Table 3) qualifies only one of the studies as “fair quality” [58] – the only one to match compared patient groups. The remaining studies were considered “poor quality,” essentially for not scoring in the comparability domain (see online suppl. material).
Discussion
All reviewed articles were institutional retrospective cohort studies with heterogeneous methods and inclusion criteria. Patients received preoperative EEN with different indications and regimens and for different periods of time. Those belonging to control groups were also heterogeneous between studies and even within the same study, namely regarding baseline nutritional state and CD activity, behavior, and medication. The type of postoperative complications analyzed also varied between studies. Meta-analysis was not done due to the small number of studies with varying designs, posing issues over the estimation of the between-study variance [61].
A non-intentional absence of studies referring to supplemental EN among those reviewed resulted from those which were eligible and referring to supplemental EN meeting exclusion criteria [44, 45, 47–50, 52–56].
From the reviewed articles, two were from China [57, 60], one of them being the study with the largest number of patients [57]. This latter study contains more patients than the sum of all three other reviewed papers, possibly raising transferability issues to other institutions and countries, namely, the Western ones. Although EN is not indicated as treatment for CD in adults by Chinese guidelines [62], eight of the excluded studies originated from China. The article by Li et al. [57] was produced by the same institution as that of seven [46–48, 50–52, 54] of the previous 8 studies, the latter being well known for its publications regarding this topic [31, 34, 63]. One of the excluded articles is Japanese [45]. The Japanese consensus indicates EN for remission induction and maintenance in adult CD [64] but, for the most part, studies from Japan focus on the possible impact of this nutrition on the reduction of postoperative relapse and remission maintenance – both as monotherapy and as an adjunct to pharmacotherapy [65–67].
Both reviewed Western studies made use of orally administered polymeric EEN [58, 59]. In both cases, an enriched formula with transforming growth factor beta-2 (TGF-β2) was used, the advantages of which have been studied for this pathology but not yet proved [17, 24, 68]. In the West, the administration of nutritional support by means of a nasogastric tube is poorly accepted by adults [24]. However, tolerance and acceptance towards the oral route has grown with improvements in the quality and variety of flavors of the polymeric formulations [24, 27].
In all studies, preoperative EEN was well tolerated by adults with complicated CD and a patent intestinal route, even in the presence of active inflammation and abdominal abscesses, leading to the possibility of postponing and even preventing surgery [58, 60]. A preoperative lag allowed for amelioration of patient conditions – reducing the inflammatory environment [58–60], increasing serum albumin [59, 60], weaning or suspending CST therapy [57, 59], and treating abscesses [59, 60] – as opposed to patients operated on immediately [58, 59]. These properties have also been attributed to nutritional support, both enteral and parenteral, by other authors [44, 47, 48, 50, 52–54, 69–72]. Also, in one of the reviewed studies [59], going straight to surgery (non-EEN patients) was an independent risk factor for anastomotic leaks and/or intra-abdominal abscesses.
The authors of one of the reviewed studies [60] refer that EEN led to a significant improvement in nutritional status based solely on a significant rise in serum albumin. Three articles specify BMI values [57–59], one of which also referring to weight loss above 10% [59] and another referring to basal and preoperative weights [58]. Nevertheless, in truth, none of the papers explains the methodology used for nutritional assessment. Standing alone, these anthropometric and laboratory parameters are not indicators of nutritional status in the presence of an active inflammatory syndrome, seeing they are highly influenced by variation in and retention of fluids [16, 49]. Preoperative serum albumin levels may reflect variations in a patient’s inflammatory status and/or nutritional state and, therefore, for one or both reasons, values below 3 g/ dL are a risk factor for postoperative complications in abdominal surgery [4, 5, 7, 11, 16]. The inflammatory environment elicited by the disease and surgery actively contributes to a descent in serum albumin and perioperative undernutrition, the control of the former being determinant in the improvement of the latter two [63, 73, 74]. In so being, nutritional support may be an essential weapon against the systemic inflammatory response syndrome and in promoting the restoration of the intestinal mucosal barrier, of immunological balance and tissue scarring, thereby leading to fewer postoperative complications and a faster recovery of the patient [16, 73, 74].
Two studies found preoperative EEN to be an independent factor against infectious and non-infectious complications [57] and against anastomotic leaks or abscesses [58]. However, only the study involving 780 surgeries [57] found EEN to lead to a significantly lower occurrence of postoperative emergent surgery, primary stomata, anastomotic leaks, and reoperations, as opposed to groups under immunosuppression alone. Although anastomotic dehiscence rates among the EEN and immunosuppressant-free groups were low (4.1 and 3%, respec tively), stoma rates were notably higher (17.8 and 22%, respectively) [57]. In the other three studies [58–60], stoma rates were similar between EEN and control groups but, in one of them, they were in fact very high (43.5 and 46.4%, respectively) [60].
It is noteworthy that no study reported on ostomies resulting from anastomotic dehiscence, on temporary ostomies that became permanent, or on ostomy closure morbidity. Yet, one of the main concerns of CD patients is that surgery may result in the need for an ostomy bag [75], which can lead to fear or even refusal of operations. Therefore, the possibility that preoperative EEN may lead to a lower stoma rate – whether primary or resulting from postoperative complications – is one of the most important aspects to consider in the surgery of these patients.
Despite the fact that all reviewed studies are retrospective and, consequently, of limited relevance, there is no doubt EEN was well tolerated and the preferred nutritional support, in the absence of intestinal obstruction, in the presence of complicated disease. In addition to its nutritional value, however, it is necessary to ascertain whether in fact this nutritional support conduces to mitigation of postoperative complications, reductions in stoma rates, decreased disease activity, removal of harmful drugs, and avoidance of emergent surgery.
The studies do collectively, nonetheless, call the attention of the scientific community to the potential benefits of preoperative EEN on postoperative outcomes in adult CD. They also carry enough impact to call for multi-institutional studies and randomized controlled trials. The design of this kind of trials, however, is a painstaking endeavor, since a great number of variables – relating to patients, disease, medication, surgical indications, and technique – must be considered. Also, ethical issues concerning randomization of malnourished CD patients towards receiving or not receiving nutritional support before surgery may limit the feasibility of such studies.
The determination of the properties of preoperative EEN is of importance since, as of now, this strategy has been very little or not at all used in most referral centers worldwide, outside the bounds of nutritional support. Only then will the contribution of preoperative EN on postoperative morbidity and stoma rates of adult CD be defined.
Conclusions
In summary, preoperative EEN in adult CD surgery can be a valid option in specific situations – to improve nutritional status in the absence of intestinal obstruction, as an adjuvant to the treatment of existing abscesses and/ or fistulas, and to attempt CST suspension.
However, none of the reviewed studies clarifies the possible existence of a cause-effect relationship between preoperative EEN and surgical morbidity in adult CD, their conclusions being far from definite. The few existing studies either carry obvious biases, varying risks of systematic errors, or questionable transferability of conclusions to other institutions. Prospective studies are required to establish whether or not preoperative EEN can in fact improve surgical outcomes in these patients.
References
1 Bernell O, Lapidus A, Hellers G. Risk factors for surgery and postoperative recurrence in Crohn’s disease. Ann Surg. 2000 Jan;231(1):38–45.
2 Rungoe C, Langholz E, Andersson M, Basit S, Nielsen NM, Wohlfahrt J, et al. Changes in medical treatment and surgery rates in inflammatory bowel disease: a nationwide cohort study 1979-2011. Gut. 2014 Oct;63(10):1607–16. [ Links ]
3 Zhulina Y, Udumyan R, Tysk C, Montgomery S, Halfvarson J. The changing face of Crohn’s disease: a population-based study of the natural history of Crohn’s disease in Örebro, Sweden 1963-2005. Scand J Gastroenterol. 2016 Mar;51(3):304–13.
4 Huang W, Tang Y, Nong L, Sun Y. Risk factors for postoperative intra-abdominal septic complications after surgery in Crohn’s disease: A meta-analysis of observational studies. J Crohn’s Colitis. 2015 Mar;9(3):293–301.
5 Patel KV, Darakhshan AA, Griffin N, Williams AB, Sanderson JD, Irving PM. Patient optimization for surgery relating to Crohn’s disease. Nat Rev Gastroenterol Hepatol. 2016 Dec;13(12):707–19.
6 Alves A, Panis Y, Bouhnik Y, Pocard M, Vicaut E, Valleur P. Risk factors for intra-abdominal septic complications after a first ileocecal resection for Crohn’s disease: a multivariate analysis in 161 consecutive patients. Dis Colon Rectum. 2007 Mar;50(3):331–6.
7 Yamamoto T, Allan RN, Keighley MR. Risk factors for intra-abdominal sepsis after surgery in Crohn’s disease. Dis Colon Rectum. 2000 Aug;43(8):1141–5.
8 Tzivanakis A, Singh JC, Guy RJ, Travis SP, Mortensen NJ, George BD. Influence of risk factors on the safety of ileocolic anastomosis in Crohn’s disease surgery. Dis Colon Rectum. 2012 May;55(5):558–62.
9 Aberra FN, Lewis JD, Hass D, Rombeau JL, Osborne B, Lichtenstein GR. Corticosteroids and immunomodulators: postoperative infectious complication risk in inflammatory bowel disease patients. Gastroenterology. 2003 Aug;125(2):320–7. [ Links ]
10 Gionchetti P, Dignass A, Danese S, Magro Dias FJ, Rogler G, Lakatos PL, et al.; ECCO. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 2: Surgical management and special situations. J Crohn’s Colitis. 2017 Feb;11(2):135–49.
11 Morar PS, Hodgkinson JD, Thalayasingam S, Koysombat K, Purcell M, Hart AL, et al. Determining Predictors for Intra-abdominal Septic Complications Following Ileocolonic Resection for Crohn’s Disease-Considerations in Pre-operative and Peri-operative Optimisation Techniques to Improve Outcome. J Crohn’s Colitis. 2015 Jun;9(6):483–91.
12 Yamamoto T, Spinelli A, Suzuki Y, SaadHossne R, Teixeira FV, de Albuquerque IC, et al. Risk factors for complications after ileocolonic resection for Crohn’s disease with a major focus on the impact of preoperative immunosuppressive and biologic therapy: A retrospective international multicentre study. United European Gastroenterol J. 2016 Dec;4(6):784–93.
13 Narula N, Charleton D, Marshall JK. Metaanalysis: peri-operative anti-TNFα treatment and post-operative complications in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2013 Jun;37(11):1057–64. [ Links ]
14 Billioud V, Ford AC, Tedesco ED, Colombel JF, Roblin X, Peyrin-Biroulet L. Preoperative use of anti-TNF therapy and postoperative complications in inflammatory bowel diseases: a meta-analysis. J Crohn’s Colitis. 2013 Dec;7(11):853–67.
15 Bemelman WA, Warusavitarne J, Sampietro GM, Serclova Z, Zmora O, Luglio G, et al. ECCO-ESCP Consensus on Surgery for Crohn’s Disease. J Crohns Colitis. 2018 Jan;12(1):1–16.
16 Weimann A, Braga M, Carli F, Higashiguchi T, Hübner M, Klek S, et al. ESPEN guideline: clinical nutrition in surgery. Clin Nutr. 2017 Jun;36(3):623–50. [ Links ]
17 Forbes A, Escher J, Hébuterne X, Kłęk S, Krznaric Z, Schneider S, et al. ESPEN guideline: clinical nutrition in inflammatory bowel disease. Clin Nutr. 2017 Apr; 36(2):321–47. [ Links ]
18 Grass F, Pache B, Martin D, Hahnloser D, Demartines N, Hübner M. Preoperative Nutritional Conditioning of Crohn’s PatientsSystematic Review of Current Evidence and Practice. Nutrients. 2017 Jun;9(6):562.
19 Schwartz E. Perioperative Parenteral Nutrition in Adults With Inflammatory Bowel Disease: A Review of the Literature. Nutr Clin Pract. 2016 Apr;31(2):159–70. [ Links ]
20 Voitk AJ, Echave V, Feller JH, Brown RA, Gurd FN. Experience with elemental diet in the treatment of inflammatory bowel disease. Is this primary therapy? Arch Surg. 1973 Aug;107(2):329–33. [ Links ]
21 Gassull MA, Abad A, Cabré E, González-Huix F, Giné JJ, Dolz C. Enteral nutrition in inflammatory bowel disease. Gut. 1986 Nov; 27 Suppl 1:76-80. [ Links ]
22 Ruemmele FM, Veres G, Kolho KL, Griffiths A, Levine A, Escher JC, et al.; European Crohn’s and Colitis Organisation; European Society of Pediatric Gastroenterology, Hepatology and Nutrition. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J Crohn’s Colitis. 2014 Oct; (10):1179–207.
23 Connors J, Basseri S, Grant A, Giffin N, Mahdi G, Noble A, et al. Exclusive Enteral Nutrition Therapy in Paediatric Crohn’s Disease Results in Long-term Avoidance of Corticosteroids: Results of a Propensity-score Matched Cohort Analysis. J Crohn’s Colitis. 2017 Sep;11(9):1063–70.
24 Zachos M, Tondeur M, Griffiths AM, Griffiths Anne M. Enteral nutritional therapy for induction of remission in Crohn’s disease. In: Zachos M, editor. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2007. https://doi.org/10.1002/14651858.CD000542.pub2.
25 Lee J, Allen R, Ashley S, Becker S, Cummins P, Gbadamosi A, et al.; Gastroenterology Specialist Group of the British Dietetic Association. British Dietetic Association evidencebased guidelines for the dietary management of Crohn’s disease in adults. J Hum Nutr Diet. 2014 Jun;27(3):207–18.
26 Hou JK, Lee D, Lewis J. Diet and inflammatory bowel disease: review of patient-targeted recommendations. Clin Gastroenterol Hepatol. 2014 Oct;12(10):1592–600. [ Links ]
27 Wall CL, Day AS, Gearry RB. Use of exclusive enteral nutrition in adults with Crohn’s disease: a review. World J Gastroenterol. 2013 Nov;19(43):7652–60.
28 Gomollón F, Dignass A, Annese V, Tilg H, Van Assche G, Lindsay JO, et al.; ECCO. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 1: Diagnosis and medical management. J Crohn’s Colitis. 2017 Jan;11(1):3–25.
29 Levine A, Wine E. Effects of enteral nutrition on Crohn’s disease: clues to the impact of diet on disease pathogenesis. Inflamm Bowel Dis. 2013 May;19(6):1322–9.
30 Yamamoto T, Nakahigashi M, Umegae S, Kitagawa T, Matsumoto K. Impact of elemental diet on mucosal inflammation in patients with active Crohn’s disease: cytokine production and endoscopic and histological findings. Inflamm Bowel Dis. 2005 Jun;11(6):580–8.
31 Tao QS, Ren JA, Yu BJ, Wang XB, Li JS. Early therapeutic benefit of enteral nutrition in active Crohn disease. Nutr Res. 2007;27(2):92–6. [ Links ]
32 Grover Z, Burgess C, Muir R, Reilly C, Lewindon PJ. Early Mucosal Healing with Exclusive Enteral Nutrition is Associated with Improved Outcomes in Newly Diagnosed Children with Luminal Crohn’s disease. J Crohn’s Colitis. 2016 Oct;10(10):1159–64.
33 Feng Y, Li Y, Mei S, Zhang L, Gong J, Gu L, et al. Exclusive enteral nutrition ameliorates mesenteric adipose tissue alterations in patients with active Crohn’s disease. Clin Nutr. 2014 Oct;33(5):850–8.
34 Li Y, Zhu W, Gong J, Zuo L, Zhang W, Gu L, et al. Influence of exclusive enteral nutrition therapy on visceral fat in patients with Crohn’s disease. Inflamm Bowel Dis. 2014 Sep;20(9):1568–74.
35 MacLellan A, Moore-Connors J, Grant S, Cahill L, Langille MG, Van Limbergen J. The impact of exclusive enteral nutrition (EEN) on the gut microbiome in Crohn’s disease: A review. Nutrients. 2017 May;9(5):E0447.
36 Leach ST, Mitchell HM, Eng WR, Zhang L, Day AS. Sustained modulation of intestinal bacteria by exclusive enteral nutrition used to treat children with Crohn’s disease. Aliment Pharmacol Ther. 2008 Sep;28(6):724–33.
37 Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 Jul;6(7):e1000097. [ Links ]
38 Wells GA, Shea B, O’Connell O, Peterson J, Welch V, Losos MT. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis.http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Published 2004. Accessed August 26, 2018.
39 Kubota Y, Kawaguchi Y, Takenoue T, Saito S, Takegami K. [Parenteral and enteral nutrition for surgical treatment of Crohn’s disease]. Nihon Rinsho. 2001 May;59 Suppl 5:504–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11439586.
40 Barbe L, Carbonnel F, Carrat F, Beaugerie L, Sezeur A, Gallot D, et al. [Effects of preoperative artificial nutrition in intestinal resections for Crohn disease]. Gastroenterol Clin Biol. 1996;20(10):852–7. Available from:http://www.ncbi.nlm.nih.gov/pubmed/8991147. [ Links ]
41 Niu LY, Gong JF, Wei XW, Zhu WM, Li N, Li JS. [Effects of perioperative combined nutritional support in Crohn disease]. Zhonghua Wai Ke Za Zhi. 2009 Feb;47(4):275–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19570390. [ Links ]
42 Xie Y, Zhu WM, Li NL, Li JS. [Enteral nutritional therapy in Crohn disease complicated with incomplete intestinal obstruction]. Chinese. Zhonghua Wei Chang Wai Ke Za Zhi. 2010;13(12):891–4. [ Links ]
43 Smedh K, Andersson M, Johansson H, Hagberg T. Preoperative management is more important than choice of sutured or stapled anastomosis in Crohn’s disease. Eur J Surg. 2002;168(3):154–7.
44 Zerbib P, Koriche D, Truant S, Bouras AF, Vernier-Massouille G, Seguy D, et al. Pre-operative management is associated with low rate of post-operative morbidity in penetrating Crohn’s disease. Aliment Pharmacol Ther. 2010 Aug;32(3):459–65.
45 Kanazawa A, Yamana T, Okamoto K, Sahara R. Risk factors for postoperative intra-abdominal septic complications after bowel resection in patients with Crohn’s disease. Dis Colon Rectum. 2012 Sep;55(9):957–62.
46 Li G, Ren J, Wang G, Hu D, Gu G, Liu S, et al. Preoperative exclusive enteral nutrition reduces the postoperative septic complications of fistulizing Crohn’s disease. Eur J Clin Nutr. 2014 Apr;68(4):441–6.
47 Zhu W, Guo Z, Zuo L, Gong J, Li Y, Gu L, et al. CONSORT: Different End-Points of Preoperative Nutrition and Outcome of Bowel Resection of Crohn Disease: A Randomized Clinical Trial. Medicine (Baltimore). 2015 Jul;94(29):e1175. [ Links ]
48 Zhang T, Yang J, Ding C, Li Y, Gu L, Wei Y, et al. Preoperative Intra-abdominal Sepsis, Not Penetrating Behavior Itself, Is Associated With Worse Postoperative Outcome After Bowel Resection for Crohn Disease: A Retrospective Cohort Study. Medicine (Baltimore). 2015 Nov;94(45):e1987. [ Links ]
49 Zhang M, Gao X, Chen Y, Zhi M, Chen H, Tang J, et al. Body Mass Index Is a Marker of Nutrition Preparation Sufficiency Before Surgery for Crohn’s Disease From the Perspective of Intra-Abdominal Septic Complications. Medicine (Baltimore). 2015;94(35):e1455.
50 Guo Z, Guo D, Gong J, et al. Preoperative Nutritional Therapy Reduces the Risk of Anastomotic Leakage in Patients with Crohn’s Disease Requiring Resections. Gastroenterol Res Pract. 2016;2016(Article ID 5017856):5017856.
51 Wang H, Zuo L, Zhao J, Dong J, Li Y, Gu L, et al. Impact of Preoperative Exclusive Enteral Nutrition on Postoperative Complications and Recurrence After Bowel Resection in Patients with Active Crohn’s Disease. World J Surg. 2016 Aug;40(8):1993–2000.
52 Guo K, Ren J, Li G, Hu Q, Wu X, Wang Z, et al. Risk factors of surgical site infections in patients with Crohn’s disease complicated with gastrointestinal fistula. Int J Colorectal Dis. 2017 May;32(5):635–43.
53 Dreznik Y, Horesh N, Gutman M, Gravetz A, Amiel I, Jacobi H, et al. Preoperative Nutritional Optimization for Crohn’s Disease Patients Can Improve Surgical Outcome. Dig Surg. 2018;35(5):442–7.
54 Liu S, Miao J, Wang G, Wang M, Wu X, Guo K, et al. Risk factors for postoperative surgical site infections in patients with Crohn’s disease receiving definitive bowel resection. Sci Rep. 2017 Aug;7(1):9828.
55 Fumery M, Seksik P, Auzolle C, Munoz-Bongrand N, Gornet JM, Boschetti G, et al.; REMIND study group investigators. Postoperative Complications after Ileocecal Resection in Crohn’s Disease: A Prospective Study From the REMIND Group. Am J Gastroenterol. 2017 Feb;112(2):337–45.
56 El-Hussuna A, Pinkney T, Zmora O, et al. Risk factors for unfavourable postoperative outcome in patients with Crohn’s disease undergoing right hemicolectomy or ileocaecal resection. An international audit by ESCP and S-ECCO. Color Dis. 2018;20(3):219–27.
57 Li Y, Zuo L, Zhu W, Gong J, Zhang W, Gu L, et al. Role of exclusive enteral nutrition in the preoperative optimization of patients with Crohn’s disease following immunosuppressive therapy. Medicine (Baltimore). 2015 Feb;94(5):e478.
58 Heerasing N, Thompson B, Hendy P, Heap GA, Walker G, Bethune R, et al. Exclusive enteral nutrition provides an effective bridge to safer interval elective surgery for adults with Crohn’s disease. Aliment Pharmacol Ther. 2017 Mar;45(5):660–9.
59 Beaupel N, Brouquet A, Abdalla S, Carbonnel F, Penna C, Benoist S. Preoperative oral polymeric diet enriched with transforming growth factor-beta 2 (Modulen) could decrease postoperative morbidity after surgery for complicated ileocolonic Crohn’s disease. Scand J Gastroenterol. 2017 Jan;52(1):5–10.
60 Zhu Y, Xu L, Liu W, Qi W, Cao Q, Zhou W. Safety and Efficacy of Exclusive Enteral Nutrition for Percutaneously Undrainable Abdominal Abscesses in Crohn’s Disease. Gastroenterol Res Pract. 2017;2017:6360319.
61 Borenstein M, Hedges LV, Higgins JP, Rothstein HR. When Does it Make Sense to Perform a Meta-Analysis? Introduction to MetaAnalysis. Chichester, UK: John Wiley & Sons, Ltd; 2009. pp. 357–64. [ Links ]
62 Ouyang Q, Hu PJ, Qian JM, Zheng JJ, Hu RWCHINESE COOPERATIVE GROUP FOR THE STUDY ON IBD; CHINESE SOCIETY OF GASTROENTEROLOGY. Consensus on the management of inflammatory bowel disease in China in 2007. J Dig Dis. 2008 Feb;9(1):52–62. [ Links ]
63 Zhao J, Dong JN, Gong JF, Wang HG, Li Y, Zhang L, et al. Impact of enteral nutrition on energy metabolism in patients with Crohn’s disease. World J Gastroenterol. 2015 Jan;21(4):1299–304.
64 Ueno F, Matsui T, Matsumoto T, Matsuoka K, Watanabe M, Hibi T; Guidelines Project Group of the Research Group of Intractable Inflammatory Bowel Disease subsidized by the Ministry of Health, Labour and Welfare of Japan and the Guidelines Committee of the Japanese Society of Gastroenterology. Evidence-based clinical practice guidelines for Crohn’s disease, integrated with formal consensus of experts in Japan. J Gastroenterol. 2013 Jan;48(1):31–72.
65 Yamamoto T, Shiraki M, Nakahigashi M, Umegae S, Matsumoto K. Enteral nutrition to suppress postoperative Crohn’s disease recurrence: a five-year prospective cohort study. Int J Colorectal Dis. 2013 Mar;28(3):335–40.
66 Takagi S, Utsunomiya K, Kuriyama S, Yokoyama H, Takahashi S, Iwabuchi M, et al. Effectiveness of an half elemental diet’ as maintenance therapy for Crohn’s disease: A randomized-controlled trial. Aliment Pharmacol Ther. 2006 Nov;24(9):1333–40.
67 Hanai H, Iida T, Takeuchi K, Arai H, Arai O, Abe J, et al. Nutritional therapy versus 6-mercaptopurine as maintenance therapy in patients with Crohn’s disease. Dig Liver Dis. 2012 Aug;44(8):649–54.
68 Hartman C, Berkowitz D, Weiss B, Shaoul R, Levine A, Adiv OE, et al. Nutritional supplementation with polymeric diet enriched with transforming growth factor-beta 2 for children with Crohn’s disease. Isr Med Assoc J. 2008 Jul;10(7):503–7. Available from: https://www.ima.org.il/FilesUpload/IMAJ/0/44/22242.pdf.
69 Hu D, Ren J, Wang G, Li G, Liu S, Yan D, et al. Exclusive enteral nutritional therapy can relieve inflammatory bowel stricture in Crohn’s disease. J Clin Gastroenterol. 2014 Oct;48(9):790–5.
70 Müller-Wille R, Iesalnieks I, Dornia C, Ott C, Jung EM, Friedrich C, et al. Influence of percutaneous abscess drainage on severe postoperative septic complications in patients with Crohn’s disease. Int J Colorectal Dis. 2011 Jun;26(6):769–74.
71 He X, Lin X, Lian L, Huang J, Yao Q, Chen Z, et al. Preoperative Percutaneous Drainage of Spontaneous Intra-Abdominal Abscess in Patients With Crohn’s Disease: A Meta-Analysis. J Clin Gastroenterol. 2015 Oct;49(9):e82–90.
72 Yan D, Ren J, Wang G, Liu S, Li J. Predictors of response to enteral nutrition in abdominal enterocutaneous fistula patients with Crohn’s disease. Eur J Clin Nutr. 2014 Aug;68(8):959–63.
73 Soeters PB, Schols AM. Advances in understanding and assessing malnutrition. Curr Opin Clin Nutr Metab Care. 2009 Sep;12(5):487–94. [ Links ]
74 Soeters P, Bozzetti F, Cynober L, Forbes A, Shenkin A, Sobotka L. Defining malnutrition: A plea to rethink. Clin Nutr. 2017 Jun;36(3):896–901. [ Links ]
75 Stjernman H, Tysk C, Almer S, Ström M, Hjortswang H. Worries and concerns in a large unselected cohort of patients with Crohn’s disease. Scand J Gastroenterol. 2010 Jun;45(6):696–706.
Disclosure Statement
The authors declare no conflicts of interest.
* Corresponding author.
Anabela Rocha
Hospital de Santo António, Centro Hospitalar do Porto
Largo Prof. Abel Salazar
PT–4099-001 Porto (Portugal)
E-Mail anabela.rocha2@gmail.com
Received: April 29, 2018; Accepted after revision: October 16, 2018
Acknowledgements
The authors thank Isabel Fonseca for her counsel on statistical methodology.
Author Contributions
A. Rocha conceived and designed the study. A. Rocha and I. Bessa undertook the bibliographic research and, independently, screened the articles. A. Rocha, I. Bessa, and P. Lago selected for eligibility, determined inclusion, and reviewed the articles included. A. Rocha and I. Bessa drafted the manuscript. P. Lago, M.D. Santos, J. Leite, and F. Castro-Poças revised the draft and approved the final manuscript.














