1. Introduction
1.1 Asthma and self-management
Asthma is among the most common chronic diseases in the pediatric population (Al-Durra et al., 2015; Jones et al., 2022; World Health Organization, 2021) and is responsible for high morbidity and mortality (GAR 2022, n.d.; Jones et al., 2022). In Latin America, the prevalence reported in the pediatric population is over 15% (Forno et al., 2015). Symptoms can be controlled through proper self-management, medication adherence, and trigger avoidance (Grady & Gough, 2014; Jones et al., 2022).
1.2 Factors Related to Asthma Self-management
Self-management is influenced by individual and environmental factors (Rush, 2014). The Social-Ecological Model (SE) and Theory of Planned Behavior (TPB) provide insight into these factors (Golden & Earp, 2012; Rush, 2014). The TPB holds that behavior is determined by intention based on beliefs, attitudes, norms, and preferences (Rush, 2014). SE emphasizes the influence of interpersonal (family, friends), organizational (schools, colleges), and societal (public policy, health systems) contexts (Kilanowski, 2017).
Asthma self-management is poorly understood in the pediatric population in low-middle-income countries with high mortality rates (GINA, 2019; Ramdzan et al., 2020; Trikamjee et al., 2022). Most evidence comes from high-income countries and combines the perspectives of parents, healthcare personnel, and children/adolescents. Limited information exists on individual and environmental influences described solely by children/adolescents. The scarce data from vulnerable communities makes it challenging to incorporate appropriate self-management skills adapted to their contexts (Blaakman et al., 2014; Miles et al., 2017). This knowledge gap hinders the development of effective strategies for improving self-management.
This report is part of a project aiming to describe the environmental and individual factors perceived by children, adolescents, parents, and medical staff that influence asthma self-management (GAR 2022, n.d.; Jones et al., 2022). The data collected from children and adolescents are analyzed separately to understand their unique perspectives as individuals experiencing asthma firsthand. A separate analysis of children's perspectives is strategic to give sense to the views of third parties (parents and medical staff) and improve the management support protocols (Ramdzan et al., 2020; Walker & Reznik, 2014). Additionally, data from children's and adolescents' voices have gained recognition in qualitative research (Schelbe et al., 2015; Sun et al., 2023) as this age group is trustable, valid, and relevant sources of information (Pinter & Zandian, 2013; Schelbe et al., 2015). Future reports will present data triangulation from all participants.
Our research question was: What factors influence pediatric asthma self-management from the perspective of patients from a middle-income country? The research aims to identify factors influencing asthma self-management according to the view of children and adolescents living in a middle-income country. In addition, we propose a conceptual framework for asthma self-management. Understanding these influences could guide the design of interventions and strategies to support asthma self-management of children/adolescents in similar contexts.
2. Methods
2.1 Qualitative Approach and Research Paradigm
A study with a phenomenological-interpretive approach using a constructivist paradigm was implemented in 2021 in Cuenca-Ecuador. Phenomenology allows us to understand what individuals have or do not have in common according to their experiences with a particular phenomenon (Creswell & Poth, 2016).
Based on the notion that the meaning of a phenomenon is built from one's own experience and social interaction (Khan, 2014; Mogashoa, 2014), we aimed to understand, interpret and describe the factors involved in asthma self-management through the experiences, practices, beliefs, attitudes, and perceptions of a group of asthmatic children and adolescents.
2.2 Researchers' Characteristics and Reflexivity
The research team had no previous relationship with the participants. A psychologist (MJP), and a pharmacist (CO) with experience in the field and qualitative research, conducted the interviews. A pharmacist (SV) with experience in qualitative interviewing participated as an observer to take notes. A pharmacist (NL) transcribed the interviews. Two independent researchers performed data coding (pharmacists NL and KP); an expert in epidemiology with experience in qualitative research supervised the analysis (AO). Two experts in qualitative research (DV and SA) provided feedback on the different stages of the research. Reflexivity was warranted by continuous meetings among the researchers to discuss and analyze the outcomes considering diverse points of view at each stage.
2.3 Context and Sampling Strategy
The study was conducted in Cuenca, Ecuador's Andean region. The Ecuadorian healthcare system involves public (government-funded) and private healthcare facilities, with specialist physicians and nurses serving in both systems (Lucio et al., 2011). In Ecuador, like other Latin American countries, inequalities in access to health systems exist (Armijos Bravo & Camino Mogro, 2017). In this context, children and adolescents, users of both public and private healthcare systems, were invited to participate. An Immunologist's medical records were used to identify potential participants using purposive sampling The potential participants were children and adolescents (7-17-year-olds) diagnosed with asthma by pulmonologists in the public and private systems. Only patients with internet access and no verbal communication limitations were included.
2.4 Ethical issues
The Ethics Committee of the University of Cuenca approved the study (2018-235E). The Standards for Reporting Qualitative Research (SRQR) were applied to this report (O’Brien et al., 2014). The legal guardians were contacted by telephone, and those interested, received an informed consent form by email to be signed within 48 hours. Later, the children and adolescents were invited to participate by signing an informed assent. We obtained written consent signed by ten parents out of 26 contacted. The research team signed a confidentiality agreement and declared no conflicts of interest. Participants were asked to provide only one name or pseudonym for the interviews. Each interview was assigned a code to avoid including personal data; for example, interview audios were stored using the codes. Zoom meetings were created using institutional accounts, and a login password was assigned. All participants received a $10 shopping voucher at the end of their participation.
2.5 Data collection methods, instruments, and Technologies
Once parents signed the informed consent, data about sex, date of birth, and type of school (public or private) was collected as an indicator of socioeconomic level; in Ecuador, children/adolescents from lower economic levels attend public schools, while those from higher strata usually attend private schools (Murillo & Martínez-Garrido, 2017).
Online individual in-depth interviews were conducted from March to May 2021. A questioning route with open-ended questions was designed based on a literature review on factors associated with pediatric asthma self-management (Annex 1) (Pinart et al., 2014). The content was validated by experts in immunology (CR), epidemiology (AO), pharmacy (SD), qualitative research (SA), and health communication (DV). A pilot was conducted with an adolescent girl.
An observer matrix was created to facilitate notetaking based on the questioning route. Interviews were performed through the Zoom platform. Security settings (login password, waiting room) were set during the sessions, and only the audio files were recorded (Buchanan & Zimmer, 2012; Gray et al., 2020). Participants accessed the session using one preferred name or pseudonym. The interviews lasted approximately 60 minutes. Each session began with a short explanation of activities and general instructions (e.g., turn off the cell phone, move to a comfortable area, and avoid interruptions). The researchers assessed data saturation after each session through team meetings, analyzing the interview team's perspectives, and reviewing notes in the observer matrix.
2.6 Data Processing and Analysis
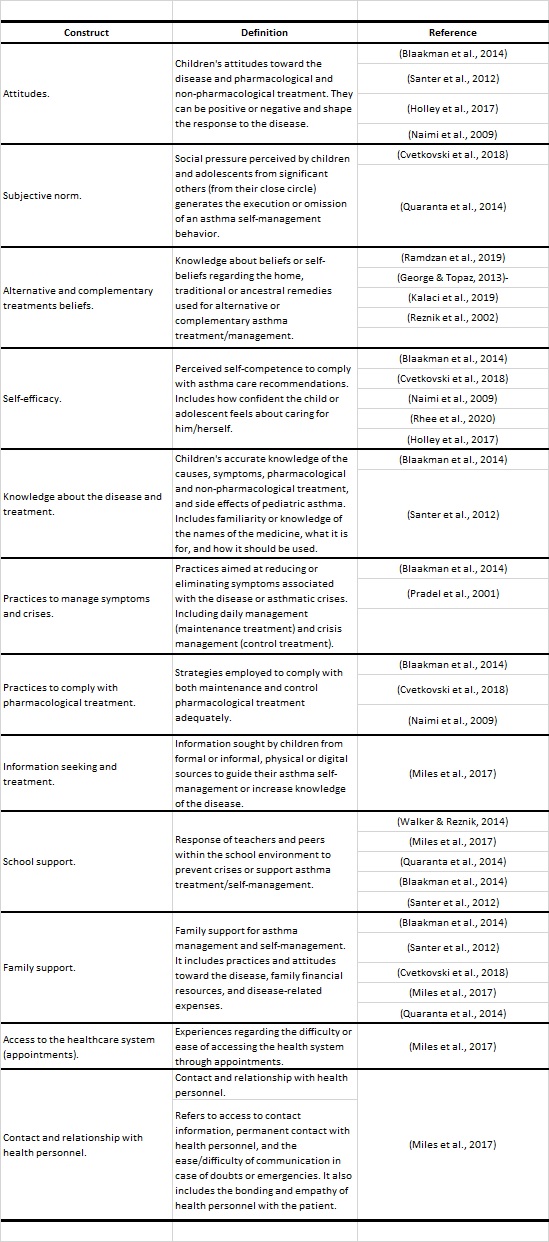
Only the audio recordings were saved and stored. All interviews were assigned with a code. A pharmacist (NL), previously trained, transcribed all the interviews' audio verbally. After familiarization with the transcripts, the research team created a coding tree based on SE theory (Glanz et al., 2008) for environmental factors and TPB (Bosnjak et al., 2020) to account for individual factors. New relevant codes (e.g., socioeconomic level) were included. The codes with detailed definitions were uploaded to NVivo 12 software. Two researchers independently coded the interviews and held comparative meetings. Discrepancies were eliminated in a researcher-triangulation process with the analysis supervisor. Finally, a report was generated for each code, identifying coincidences and discrepancies to generate a final report with a synthesis of each theme. The entire research team reviewed this synthesis until a final report was generated. In the final stage, the researchers interpreted contents and their interrelationships to develop a conceptual framework of the factors that influence asthma self-management according to the perspectives of the pediatric population.
3. Results
Ten children and adolescents were interviewed. Six were female, seven attended private schools, and the most reported comorbidity was allergic rhinitis. Factors influencing asthma self-management can be divided into individual and environmental influences.
3.1 Individual influences
Attitudes
Asthmatic children/adolescents living in an Andean region perceive that their life is different compared to others, mainly because of the limitations in their daily activities, such as active games and hobbies. These differences are a source of dissatisfaction, according to the interviewed participants. Nevertheless, they believe that their disease should be considered "normal." The participants accepted the pharmaceutical treatment; they expressed confidence in it because it relieves their symptoms. However, some adolescents expressed frustration because the disease has no cure and felt that the pharmaceutical treatment routine is tedious, causing forgetfulness.
"I got used to it because I also have classmates with asthma.”
"I wanted to do something that I could not. Sometimes I got angry, so I did it on my own anyway"
"I wanted to recover, I wanted to play, and I did not want to take medicines or anything. I no longer wanted to be sick"
"I was getting bored of doing the same thing all the time, so I did not want to"
Self-efficacy
Confidence in asthma self-management seems different according to children's age. Young children (7-12 years) mentioned that they share the care with their parents, they handle avoiding triggers (i.e., cold), and their parents oversee the pharmaceutical treatment. On the other hand, adolescents (13-17 years) are confident they can care for their disease.
Young children: "I do not think I could care for myself because I do not know how to find pills. I couldn't, I would forget very easily, besides setting the alarm, and my mother helps me a lot in that matter, so maybe not"
Adolescent: "Yes, I could; I could give myself a puff; I would put on warm clothes and take the pills at night"
Subjective norm
Although participants indicated that their life differs from non-asthmatic children's, they did not consider what other children/adolescents think about them because of their disease. Participants show confidence when others, including their peers, know about their condition. On the other hand, regarding medication use, some participants mentioned feeling uncomfortable when explaining the reasons for using it to their peers, so they avoid using their inhalers in front of their friends or classmates.
Knowledge
When inquiring into the causes of pediatric asthma, all the children/adolescents attributed their disease to hereditary factors. No other causal factors were mentioned. Parental beliefs and practices were the primary sources of knowledge about asthma symptoms and triggers. Mothers were the primary source of information regarding asthma causes, symptoms, and management. The mother's influence was more notorious in young children than in adolescents. The most critical triggers identified by the participants were: cold weather, intense physical activity, intake of cold food (e.g., ice cream), and contact with smoke or dust. The children and adolescents were aware of the pharmaceutical treatment benefits. They believe that the medication improved their symptoms. Participants often evoked the medicine's names but did not know the dosage details. Only a few participants could mention the pharmaceutical treatment side effects.
"Because of my daddy. He also had asthma"
"Due to some problem in the genes"
"I asked my mom why I had this cough; then my mom told me it was because of the dust or the cold"
"I could not run much. It was like I was short of breath and had to stop and breathe heavily"
"When I need to take my medicine, I call my mom, and she tells me what to take"
"I usually read the medicine, but I do not know the side effects; I do not remember"
Practices
Most participants reported wearing warm clothes, avoiding agitation by not practicing moderate-vigorous physical activity, having their medicines close by when practicing physical activity, and deep breathing as usual strategies to manage their symptoms and avoid crises.
"I always had the inhaler in my backpack; it always stayed there in case something happened during physical activities. Due to the cold, I always wore a sweater and sometimes a scarf"
"Only when I run, I must calm down a bit"
The participants mentioned some practices to comply with the pharmaceutical treatment.
The most common practices included writing down instructions on a piece of paper posted on the fridge or in the medicine boxes, setting alarms, placing inhalers under the pillow, and receiving phone calls from their caregivers. According to the participants, most practices were driven by their parents. The children/adolescents expressed that their skills regarding managing their disease are often based on trial and error due to the disease's chronicity. Few participants mentioned having regular outpatient visits to control their disease; most seek treatment only when a crisis arises.
"the alarms tell me at what time I have to take medicine. When I forgot, there was a piece of paper with instructions in the refrigerator"
"My mom says that she will call me when I have to take them because she says that I have to take them only when I need them; if I take more, it could hurt me"
"somethings from experience"
"one day, we were on the street before the pandemic. I had a horrible crisis. I even started vomiting. There was a hospital nearby, and they had to take me there"
Beliefs
Most participants indicate they have received suggestions from relatives about traditional practices such as eating animal meat (i.e., black dogs) for asthma treatment. However, some mentioned not agreeing with this practice. The participants agreed that they had observed an improvement when taking infusions, albeit temporarily.
"My mother's uncle did say that he ate, that they fed him with his pet, his dog. I would not do that"
"Only those infusions, which I do not know, Jamaica or something like that. Also, vaporizations, with some herbs, maybe chamomile."
3.2 Environmental Influences:
Family Support
The participants expressed having support from the whole family, but the mother's role is pivotal. They explained that the mother receives the health care instructions, resolves the child's doubts, and ensures pharmacological and non-pharmacological recommendations compliance. Some children/adolescents perceived the family's lack of financial resources as a barrier to accessing medicines and medical appointments in private hospitals. The participants felt the family's income is essential because they require permanent treatment. The latter indicates that the public health system lacks regular availability of medicines and medical appointments.
"I feel like my family helps me with everything; I feel like doctors who help me are like mini-doctors, but without being in a hospital"
"My family sometimes gets paid a little late, they sometimes do not have enough money, and I get complicated with these things... right now, I do not have the asthma spray, I need to buy it, and I do not have money, well my family does not have money"
School Support
Participants perceive a supportive attitude in their classmates; they feel safe and confident in school. In only one case, a child (10 years old) mentioned being bullied due to his disease. Physical education teachers are the central support figure at school regarding disease management, as an asthma attack could occur during their classes. However, the teachers' responses focus on avoiding physical activity and recommending rest.
"the people by my side influenced me. My classmates understood and often helped; they told me: let us know if you need anything. Moreover, the support of classmates and the environment I had at school and the high school"
"When I had to use the spray, they mocked me. So I felt ashamed then and did not use it; I managed without it"
"The teacher did know, for example, if I were feeling bad, he would tell me to go sit, and I stayed there; also, I had the inhaler nearby, so it was ok"
Healthcare system
Participants perceive that getting an appointment with physicians, pharmacists, and laboratory tests in the public health system is complicated. They consider that the medicines availability is good in the private sector; a few shortage periods were mentioned, mainly at the beginning of the COVID-19 pandemic.
"...About the exams, it was very crowded in the public system; I think there were many people, and we waited over an hour for the appointment..."
"... It is hard to get an appointment. My mommy has to go to sleep in the hospital so that they can give her an appointment because she has to wait in line until the doctor is free…."
According to the participants, their health condition was generally solved when attending a health center. However, they have had negative experiences in the public sector, such as hostile attitudes from physicians and not having access to physician contacts for emergencies. Most participants agree that they have more confidence in doctors in the private healthcare system and that accessing care in private versus public healthcare facilities is easier. The relationship with health personnel depends on the temperament and charisma of the staff. Children and adolescents perceived that a solid link with health staff does not exist; they expressed that only a typical doctor-patient relationship is established. The participants agreed that they rarely feel confident to ask questions as the doctor seems angry (particularly in the public system); they even expressed fear of interacting with the healthcare staff.
"I do not ask the doctor because he is slightly angry"
"I did not talk much with him, the doctor, but he explained my medicine if he treated me well"
According to the children/adolescents, the recommendations of the healthcare personnel were practical. However, many terms were unfamiliar to young children (7-12 years). The most valuable advice from the participant's point of view is a practical demonstration of the correct use of inhalers. If they do not understand a recommendation, their parents are responsible for resolving doubts.
"I understand it. Most talks are about vaporizations and pills they give, and that is it"
"Sometimes I do not understand the explanations"
"...while the doctor is telling my mommy what I must do, I am just playing around; I do not pay attention..."
3.3 Conceptual Framework
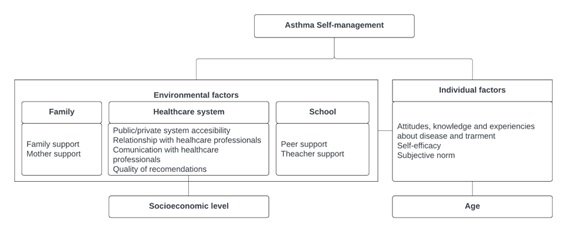
Based on the results, we developed a conceptual framework in which asthma self-management is conceptualized as a function of individual and environmental influences (Figure 1). The framework emphasizes the interaction of factors within and between levels of influence and shows how these factors can directly or indirectly influence asthma self-management. In addition to the factors described previously (e.g., social context, healthcare-related factors, education) (Daines et al., 2020; Farnesi et al., 2019), our results indicated that socioeconomic status strongly influences environmental factors (e.g., healthcare system access), and age influences individual factors (e.g., self-efficacy) for asthma self-management. This multilevel framework is helpful for understanding and explaining the factors that influence asthma self-management in Ecuadorian pediatric patients.
4. Discussion
Our findings demonstrate that the pediatric population identifies individual and environmental influences on asthma self-management. Attitudes, practices, perceptions, and specific experiences in family, school, and healthcare settings were identified as relevant issues.
4.1 Individual Influences
Our participants accept their disease and pharmaceutical treatments. Previous evidence indicates that patients with chronic diseases, such as asthma, accept and incorporate it into their lives (Kintner et al., 2022). Negative attitudes such as fatigue and frustration with prolonged medication use can lead to forgetfulness and lack of interest, especially in adolescents (Daines et al., 2020; Koster et al., 2015). Other negative attitudes are related to the limitations to performing physical activity, one of the main factors associated with poor quality of life in asthmatic patients (Daines et al., 2020; Kornblit et al., 2018).
Concerning self-efficacy, differences between children and adolescents were evident. Usually, children perceive they are incapable of self-managing their disease, and parents play a pivotal role in pediatric asthma self-management (Coyne et al., 2016; Ramdzan et al., 2020). Adolescents, in contrast, feel capable of managing their disease; however, overconfidence has been associated with inadequate self-management, especially in adolescents (Eakin & Rand, 2012). Evidence demonstrates that adequate and complete disease management could be reached in adulthood (22 years) (Farnesi et al., 2019).
Adolescents and young children (to a lesser extent) are aware of their disease symptoms, triggers, and management. Sufficient and accurate knowledge about trigger avoidance has been associated with proper self-management, greater empowerment, and self-efficacy in children and adolescents (Blaakman et al., 2014; Rangachari, 2017). However, based on our results, there are substantial misunderstandings around triggers. For example, the children have not identified essential triggers, and the proper way to avoid them is unknown. The last could be due to a lack of education regarding asthma and its management which concern most patients (Miles et al., 2017). Education to optimize asthma self-management is essential (Eakin & Rand, 2012).
Young children are not accurately aware of their treatment and need parents, especially mothers, for drug administration. Adolescents demonstrated a more significant knowledge regarding medication. As the child grows, they become more familiar with their drugs. However, evidence shows that even at 15 years, only three-quarters of adolescents can manage their treatment independently (Ramdzan et al., 2019).
Participants mentioned the ancestral belief that black dog meat consumption had been recognized as a potential treatment. The belief comes from the wisdom of the Saraguros, a Quichua nationality of Ecuador (Contribuciones a la historia ambiental de América Latina. Memorias del X Simposio SOLCHA, 2022).
Although this belief is deeply spread, many participants reject it, considering it unpleasant and ineffective. Participants, such as medicinal infusions, are complementary to medical recommendations. This practice has also been reported in European children (Kalaci et al., 2019) and North American adolescents (George & Topaz, 2013). Evidence demonstrates that it is essential to consider children's beliefs to improve treatment adherence and prevent crises (Miles et al., 2017).
One of the biggest non-adherence problems is difficulty introducing the medication-taking routine into daily life (Eakin & Rand, 2012). Written action plans, setting alarms, and parental support are key strategies to improve medication adherence (Koster et al., 2015; Miles et al., 2017) in children and adolescents (Koster et al., 2015).
During childhood, parents are the primary information source about asthma and its management; hence it is crucial to provide sufficient and accurate information to them (Srour-Alphonse et al., 2021). In the case of adolescents, parental support can be bothersome, and adolescents prefer to seek information independently (Blaakman et al., 2014; Ramdzan et al., 2020). Future interventions for asthma self-management should consider the patients' developmental stage (Blaakman et al., 2014).
Participants mentioned not giving importance to what other people think about their disease. Consistently, a study concluded that peer and teacher opinions are not considered relevant to asthma self-management practices (Quaranta et al., 2014). Children and adolescents reported positive experiences with their peers at school, although some felt discomfort when explaining the reasons for using the inhaler. The pediatric population often experiences discomfort about the disease in front of their peers, generating non-compliance with self-management practices (Holley et al., 2017).
4.2 Environmental Influences
Like other studies, participants agreed that family members are essential facilitators of asthma management; however, mothers are responsible for compliance with pharmacological and non-pharmacological treatment and medical controls. The last could represent a barrier, as ideally, children should progressively acquire responsibilities for self-management until they become fully independent (Miles et al., 2017).
Participants recognized the lack of economic resources as a barrier to medicine acquisition and adherence. Evidence shows that children from families of low socioeconomic status present poor disease control associated with inadequate treatment adherence (Solé et al., 2017; Thakur et al., 2014).
Physical education teachers were identified as the most important figures at school in supporting disease management, consistent with previous studies. However, teachers' responses often seem insufficient or erroneous (e.g., asking them to sit down, relax, and drink water), hampering proper asthma self-management. Future studies should consider the physical education teacher's significant role in promoting correct self-management habits (Walker & Reznik, 2014).
Participants identified potential facilitators in the health system, such as access to the physician's cell phone number, affinity with health personnel, and receiving clear and helpful recommendations. However, negative experiences were also reported, especially in the public system (e.g., difficulties in accessing medical appointments and healthcare personnel hostile attitudes). Previous studies reported how problems with access to medical care and poor inter-professional communication could affect self-management (Holley et al., 2017; Miles et al., 2017).
4.3 Conceptual framework
The conceptual framework developed in this study emphasizes the importance of considering children’s and adolescents' perspectives when designing interventions to improve asthma self-management (Miles et al., 2017; Rolke et al., 2022). Existing evidence has focused mainly on the combined experiences of patients, parents, and the community (Daines et al., 2020; Farnesi et al., 2019; Miles et al., 2017; Rolke et al., 2022). However, few studies have developed a conceptual framework based solely on the children's perspectives.
Evidence suggests that several individual and environmental factors affect asthma self-management (Miles et al., 2017; Rolke et al., 2022), but the role of socioeconomic status and age in these factors has not been mentioned. Our results highlight the influence of socioeconomic status and age on other factors of asthma self-management from the perspective of the pediatric population only. In addition, most of the evidence regarding asthma self-management comes from developed countries, and no studies identified socioeconomic status as a cross-sectional factor influencing pediatric asthma self-management (Daines et al., 2020; Farnesi et al., 2019; Miles et al., 2017; Rolke et al., 2022).
4.4 Strengths and limitations
The strengths of this study include its focus on an underrepresented population-children and adolescents with asthma in the Andean urban area of Cuenca, Ecuador. The findings have relevance for similar cultural, socioeconomic, and environmental populations, particularly in Latin America and other low and middle-income countries. The research team consisted of multidisciplinary experts, allowing diverse perspectives and enriching outcomes. Furthermore, this study reports the point of view of children and adolescents regarding various contexts (family, school, and health systems). This allowed for a more extensive understanding of pediatric asthma self-management. However, a limitation is the restriction of interpretation to a few theoretical models, which may influence perceptions of the phenomena. Nonetheless, the chosen models are widely recommended for studying qualitative aspects of asthma and other chronic disease self-management.
4.5 Implications for Research and Practice
Future studies should investigate parental practices that contribute to effective self-management in children at different ages, considering the influence of social, economic, and cultural environments. Additionally, the study revealed a lack of father involvement in asthma management, highlighting the need to explore social, cultural, and emotional factors that promote or hinder fathers' engagement. Furthermore, understanding the role of schools, including teachers, authorities, and peers, in fostering effective self-management practices should be a focus of future research, particularly in the Ecuadorian context. Regarding the implications for practice, interventions should consider individual and environmental factors shaping children's self-management practices. Healthcare professionals should deliver patient-centered education to enhance children's ability to manage their asthma effectively.
5. Conclusion
Our analysis highlights the need to empower the pediatric population in asthma self-management. E aspects to consider are improving patients' knowledge and practices by involving family, school, and health professionals. It is imperative to educate children and adults (family and school) about asthma and how to manage it to debunk myths and overcome erroneous beliefs and practices. The individual and environmental factors influencing asthma self-management should be considered essential to successful management programs within the healthcare system.