Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Portuguesa de Enfermagem de Reabilitação
versión impresa ISSN 2184-965Xversión On-line ISSN 2184-3023
RPER vol.6 no.1 Silvalde jun. 2023 Epub 30-Jun-2023
https://doi.org/10.33194/rper.2023.309
Literature review
Effects of early progressive mobilization programs in critically ill patients: a systematic review of the literature
1Universidade da Beira Interior, Covilhã, Portugal
2Unidade Local de Saúde do Baixo Alentejo, Portugal
3Instituto Politécnico de Bragança, Bragança, Portugal
Objective:
To know the effect of early progressive mobilization programs on the critically ill patients’ outcomes.
Methods:
Systematic review using MEDLINE, CINAHL, CENTRAL, PEDro, Clinical Trials.gov, WHO International Clinical Trials Registry Platform and EU Clinical Trials Register databases.
Results:
Of the total 813 publications identified, 18 met the inclusion criteria and were included in this review. These programs were found to be related to: reduced ventilation time, reduced intensive care length of stay, reduced likelihood of readmission and increased functionality at discharge from intensive care. There seems to be a trend towards a reduction of infections and a higher probability of discharge to home. No negative outcomes were found.
Conclusions:
In addition to being safe, early progressive mobilization programs may bring important benefits to critically ill patients, thus reinforcing the importance of intervention in this area.
DESCRIPTORS: Intensive Care Units; Critical Illness; Rehabilitation; Early Ambulation; Quality Improvement
Objetivo:
Conhecer o efeito dos programas de mobilização progressiva precoce nos resultados do doente crítico.
Métodos:
Revisão sistemática, com recurso às bases de dados MEDLINE, CINAHL, CENTRAL, PEDro, Clinical Trials.gov, WHO International Clinical Trials Registry Platform e EU Clinical Trials Register.
Resultados:
Do total de 813 publicações identificadas, 18 cumpriam os critérios de inclusão e foram incluídas nesta revisão. Verificou-se que estes programas estão relacionados com: redução do tempo de ventilação, redução do tempo de internamento em cuidados intensivos, menor probabilidade de readmissão e maior funcionalidade à alta dos cuidados intensivos. Parece verificar-se uma tendência para redução das infeções e maior probabilidade de alta para o domicílio. Não foram encontrados desfechos negativos.
Conclusões:
Os programas de mobilização progressiva precoce, além de seguros, parecem trazer benefícios importantes ao doente crítico, reforçando a importância de intervir nesta área.
DESCRITORES: Unidade de Terapia Intensiva; Estado Terminal; Reabilitação; Deambulação Precoce; Melhoria de Qualidade
Objetivo:
Conocer el efecto de los programas de movilización progresiva precoz en los resultados de los pacientes críticos.
Métodos:
Revisión sistemática utilizando las bases de datos MEDLINE, CINAHL, CENTRAL, PEDro, Clinical Trials.gov, WHO International Clinical Trials Registry Platform y EU Clinical Trials Register.
Resultados:
Del total de 813 publicaciones identificadas, 18 cumplieron los criterios de inclusión y se incluyeron en esta revisión. Se comprobó que estos programas estaban relacionados con: reducción del tiempo de ventilación, reducción de la duración de la estancia en cuidados intensivos, reducción de la probabilidad de reingreso y aumento de la funcionalidad al alta de cuidados intensivos. Parece haber una tendencia a la reducción de las infecciones y una mayor probabilidad de alta a domicilio. No se encontraron resultados negativos.
Conclusiones:
Además de ser seguros, los programas de movilización progresiva precoz parecen aportar importantes beneficios a los pacientes críticos, lo que refuerza la importancia de la intervención en este ámbito.
DESCRIPTORES: Unidades de Cuidados Intensivos; Enfermedad Crítica; Rehabilitación; Ambulación Precoz; Mejoramiento de la Calidad
INTRODUCTION
Prolonged immobility in bed is often related to critical illness and admission to an Intensive Care Unit (ICU). If in a person without critical illness, immobility has harmful consequences at various levels1, in critically ill patients, these effects are potentiated by factors such as: multiorgan failure, mechanical ventilation, drugs (corticosteroids and muscle blockers), inflammatory cytokines and high catabolism, contributing to the development of generalized muscle weakness, which conditions the patient's recovery and discharge2. In addition to physical weakness, prolonged ICU stay is also associated with states of psychosocial weakness, compromising the future quality of life and hindering the social and professional reintegration of these patients, constituting the so-called post-intensive care syndrome3-5. By definition, this syndrome refers to the impairment, new or worsening, of the physical, cognitive or mental condition, which occurs after critical illness and persists after discharge from the intensive care unit6.
In this sense, Bundle ABCDEF was developed, which includes the following intervention bundles: pain assessment, prevention and treatment (A); coordination of awakening with spontaneous ventilation training (B); choice of sedation and analgesia (C); evaluation, prevention and treatment of delirium (D); early mobilization and rehabilitation (E); and family involvement and empowerment (F) 7,8.
Although all bundles are important, in the context of rehabilitation nursing, mobilization and early rehabilitation are of particular interest. In this regard, the European Respiratory Society and the European Society of Intensive Care Medicine tell us that active or passive mobilization and muscle training should be instituted early and that techniques such as positioning, passive mobilization and muscle stretching should be used to preserve joint mobility and skeletal muscle length in patients unable to move spontaneously9. The German Society of Anesthesiology and Intensive Care adds that, in principle, early mobilization should be performed in all patients treated in intensive care, to whom exclusion criteria do not apply and that treatment should begin no later than 72 hours after admission to intensive care and be performed twice a day with a duration of at least 20 minutes. It also recommends that mobilization be gradual and suggests the development of a specific algorithm for a unit or hospital10.
Despite the apparent benefits of early mobilization, a meta-analysis carried out in 201511 concluded that although early rehabilitation allows more patients to be discharged from the hospital independently, it does not offer proven benefits in the duration of mechanical ventilation, in the length of stay in the ICU or in the length of hospitalization, in the improvement of functionality, muscle strength or quality of life. Likewise, another systematic review, published in 201812, mentions that there is not enough evidence of the effect of early mobilization on functionality, muscle strength, quality of life or the occurrence of adverse events. In opposition, another systematic review reinforced the benefits of an early mobilization program in respiratory and peripheral muscle strength, in the reduction of mechanical ventilation time and length of stay in patients mobilized early13.
Two other systematic reviews with meta-analysis, published in 2019, observed that patients mobilized early showed a reduction in hospital stay, increased muscle strength14, increased number of days free of ventilation, increased independent walking distance to hospital discharge and increased probability of discharge to home15. Although there are no significant differences in hospital mortality, mortality and adverse effects slightly increase in cases of early mobilization14,15. There were also no differences in terms of quality of life14.
As confirmed, this is still an open topic with inconsistent results for most outcomes. The cited reviews included different forms of mobilization (cycle ergometer, transcutaneous electrical neurostimulation and early rise, for example) which could have an influence on their results. Despite protocols or early progressive mobilization programs being more and more a reality 16,17, and in previous research to this review, there is no synthesis of its possible benefits in the literature. In addition, the existing reviews are mainly focused on randomized studies, which are more robust but fewer in number, excluding a significant number of studies of less scientific relevance, such as analyzing quality improvement programs, but which gather a set of information that cannot be neglected.
Thus this review is necessary, which aims to: know the effect of early progressive mobilization programs on criticallly ill patients outcomes. The starting point for this investigation was: What is the effect of early progressive mobilization program, on critically ill patient outcomes, compared to the usual treatment. These mobilization programs or protocols should have several phases, tailored to the patient's condition, and should aim to progress to out-of-bed mobilization and active ambulation. Results were compared with groups with no intervention or under usual care, including their usual physical therapy regimen.
This review is the first to specifically address this type of program. In addition, by including several research designs, namely results from the implementation of quality improvement projects, it allows to gather many studies that do not integrate the previous reviews on the subject. By encompassing an important number of variables, or health outcomes, it constitutes an important synthesis of current knowledge on the subject.
This systematic review of the literature followed the Cochrane principles(18), in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA)(19) and is registered in the international prospective register of systematic reviews (www. crd.york.ac.uk/prospero) with number CRD42020162101.
METHODOLOGY
Research strategy and selection of studies
The research strategy obeyed the key concepts defined by the following PICO model(18):
Population - Adult patients, aged 18 or older, admitted to the ICU, regardless of disease or severity;
Intervention - Early progressive mobilization programs (or protocols) aimed at out-of-bed mobilization and active ambulation, regardless of provider. These programs must have several phases adjusted to the patient's condition;
Comparator - No intervention or usual care (includes usual physiotherapy regimen);
Outcomes - Mortality, duration of mechanical ventilation, ICU length of stay, number of readmissions, length of hospital stay (primary outputs), functionality at ICU discharge, muscle strength at ICU discharge, proportion of discharges to home, incidence of infections in the ICU, incidence of pressure ulcers in the ICU, incidence of thromboembolic events in the ICU (secondary outcomes).
The research was carried out, on January 20, 2022, in the databases PubMed (MEDLINE), Cumulative Index of Nursing and Allied Health (CINAHL), Cochrane Central Register of Controlled Trials (CENTRAL), Physiotherapy Evidence Database (PEDro), Clinical Trials.gov, WHO International Clinical Trials Registry Platform and EU Clinical Trials Register.
Table 1 Research strategy
| Database | Expression | Results | |
|---|---|---|---|
| MEDLINE | #1 | (“Early Ambulation”[Mesh]) OR (“walking”[Mesh]) OR (“mobili*”[Title/Abstract]) | 270 997 |
| #2 | ("Intensive Care Units"[Mesh]) OR ("Critical Care"[Mesh]) OR ("Critical Illness"[Mesh]) | 140 507 | |
| #3 | #1 AND #2 | 1 139 | |
| CINAHL (via EbscoHost) | #1 | MW Early Ambulation OR MW walking OR AB mobili* | 51 182 |
| #2 | MW Intensive Care Units OR MW Critical Care OR MW Critical Illness | 88 816 | |
| #3 | #1 AND #2 | 863 | |
| CENTRAL (via EbscoHost) | #1 | MW Early Ambulation OR MW walking OR AB mobili* | 18 266 |
| #2 | MW Intensive Care Units OR MW Critical Care OR MW Critical Illness | 5 243 | |
| #3 | #1 AND #2 | 84 | |
| PEDro | Critical care AND mobility | 14 | |
| Clinical Trials.gov | #1 | Early Ambulation OR walking OR mobility | 18 135 |
| #2 | Intensive Care Units OR Critical Care OR Critical Illness | 7 775 | |
| #3 | #1 AND #2 | 411 | |
| WHO International Clinical Trials Registry Platform | #1 | (Early Ambulation) OR (walking) OR (mobili*) | 7 349 |
| #2 | (Intensive Care Units) OR (Critical Care) OR (Critical Illness) | 7 076 | |
| #3 | #1 AND #2 | 129 | |
| EU Clinical Trials Register | #1 | (Early Ambulation) OR (walking) OR (mobili*) | 757 |
| #2 | (Intensive Care Units) OR (Critical Care) OR (Critical Illness) | 222 | |
| #3 | #1 AND #2 | 8 | |
The terms “early ambulation”, “walking” or “mobility” were searched, combined with “intensive care units”, “critical care” or “critical illness”, according to the strategy presented in table 1.
In order to gather as much information as possible, this review, in addition to including randomized studies, also included quasi-experimental, case-control and cohort studies (including quality improvement programs with before and after design) published in English, Spanish and Portuguese. An analysis period of 15 years prior to the research was defined, including studies published between 2004 and 2019, in order to include articles that may have been the basis of current recommendations for early mobilization.
Clinical cases, systematic reviews, review articles and any studies that analyzed the effect of mobilization programs in conjunction with other interventions (e.g. ABCDE bundle) were excluded. After eliminating duplicate articles through the Mendeley program, two independent reviewers used the Rayyan application to analyze the title and abstract of the articles. The same reviewers subsequently analyzed the full text of articles that passed the first review phase to decide whether they met the defined criteria. The data relating to the studies to be included in the review were extracted into an Excel that also served as the basis for the risk of bias analysis of each one of them. Disagreements were resolved by discussion between reviewers.
RESULTS
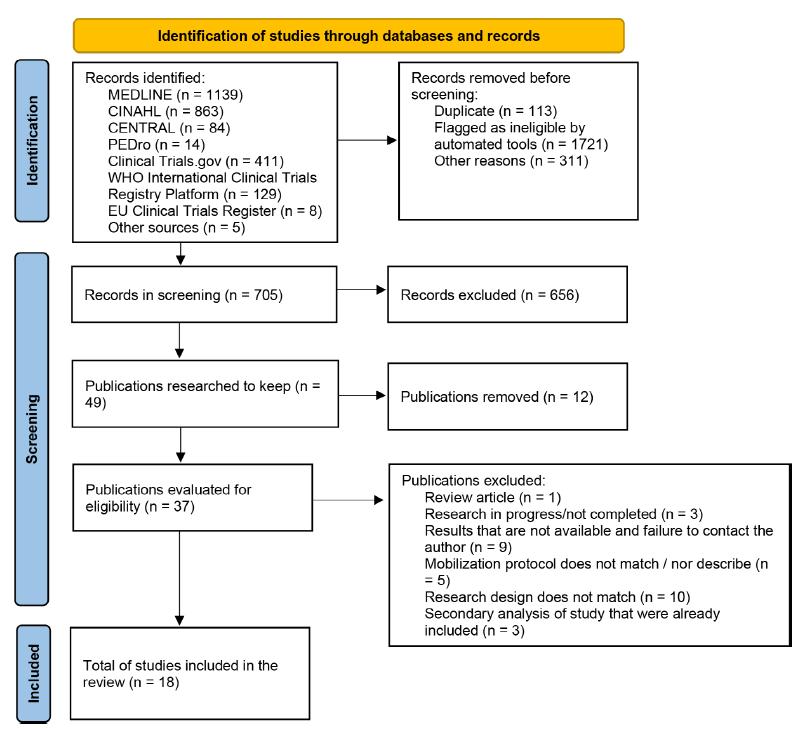
The search strategy resulted in 813 publications, 49 of which were selected for full-text analysis, of which 18 were included in this review (Figure 1).
Characteristics of the studies
Of the 18 studies included in the review (20-37) (Table 1), 3 are randomized controlled trials (RCTs) and 15 are observational studies. Many of these observational studies are related to quality improvement programs and use a design that assesses patients before and after implementation of the early mobilization program. It should be noted that 15 of the 18 studies included in the review result from data collected in the United States of America (USA) and that only one includes data collected in Europe.
Table 1 Characteristics of the studies included in the review
| Author (year) | Country | Type of study | Type of UCI | Sample size |
|---|---|---|---|---|
| Azuh et al (2016) (20) |
USA | Prospective cohort with historical control |
medical ICU | |
| Bahouth et al (2018) (21) |
USA | Quasi-experimental study | neurotrauma ICU | Pre: 27 Post: 29 |
| Booth et al (2016)(22) |
Prospective cohort with historical control |
Neurocritical ICU | Pre:184 Post:159 |
|
| Clark et al (2013) (23) |
USA | Retrospective cohort | ICU for trauma and burns | Pre: 1044 Post:1132 |
| Crane (2017) (24) |
USA | Quasi-experimental study | Medical-surgical ICU | Pre: 115 Post: 29 |
| Dickinson et al (2013) (25) | USA | Retrospective cohort | Surgical ICU | Pre: 555 Post: 557 |
| Floyd et al (2016) (26) |
USA | Retrospective cohort | cardiothoracic ICU | Pre: 30 Post: 30 |
| Fraser et al (2015) (27) |
USA | Retrospective cohort | 3 ICU (medical, surgical and coronary) | Pre: 66 Post: 66 |
| Hodgson et al (2016) (28) | Australia and New Zealand | RCT | 5 ICU (surgical and trauma medicine) | Int: 29 Ctrl: 21 |
| Klein et al (2015) (29) |
USA | Quasi-experimental study | Neurocritical ICU | Pre: 260 Post: 337 |
| Lai et al (2017) (30) |
Taiwan | Retrospective cohort | medical ICU | Pre: 63 Post: 90 |
| Liu et al (2019) (31) |
Japan | Retrospective cohort | Medical-surgical ICU | Pre: 204 Post: 187 |
| Mah et al (2013) (32) |
USA | Prospective cohort with historical control |
Surgical ICU | Pre: 31 Post: 28 |
| Morris et al (2008) (33) | EUA | Prospective cohort | 7 medical ICUs from the same IC service | Int: 165 Ctrl: 165 |
| Ronnebaum et al (2012) (34) |
USA | Retrospective cohort | Medical surgical ICU | Pre: 15 Post: 13 |
| Schaller et al (2016) (35) | Austria, Germany and USA | RCT | Surgical UCI | Int: 104 Ctrl: 96 |
| Schweickert et al (2009) (36) | USA | RCT | medical ICU | Int: 49 Ctrl: 55 |
| Winkelman et al (2012)(37) | USA | Quasi-experimental study | Medical ICU and surgical ICU | Pre: 20 Post: 55 |
USA- The United States of America; RCT - Randomized clinical trial; Int - Intervention group; Ctrl - Control Group; Pre - Pre-intervention group (control); Post - Post-intervention group (intervention); ICU - Intensive Care Unit
Quality and risk of bias
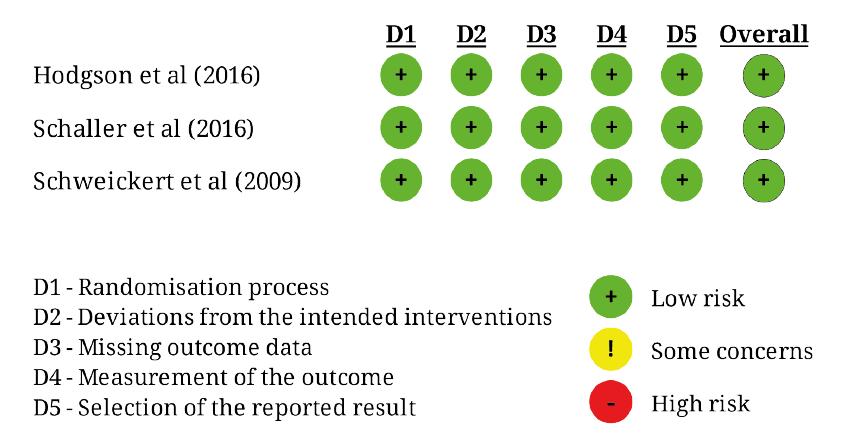
The evaluation of the methodological quality and the risk of bias of the studies included in the review was independently performed by two researchers, using the criteria of the Newcastle-Ottawa Scale (NOS - Newcastle-Ottawa Scale)38) for cohort studies (Table 3) and Risk of Bias 2 (RoB 2) 39 for randomized trials (Figure 2). Disagreement cases were resolved by discussion between the two evaluators.
Table 2 Assessment of the Newcastle-Ottawa Scale for cohort studies
| Author (year) | Selection | Comparability | Results | TOTAL |
|---|---|---|---|---|
| Azuh et al (2016) (20) | * | ** | ** | 5 |
| Bahouth et al (2018) (21) | ** | ** | ** | 6 |
| Booth et al (2016)(22) | * | ** | ** | 5 |
| Clark et al (2012) (23) | *** | ** | *** | 8 |
| Crane et al (2017) (24) | ** | *** | 5 | |
| Dickinson et al (2013) (25) | *** | ** | *** | 8 |
| Floyd et al (2016) (26) | *** | ** | *** | 8 |
| Fraser et al (2015) (27) | *** | ** | *** | 8 |
| Klein et al (2015) (29) | *** | ** | *** | 8 |
| Lai et al (2017) (30) | ** | ** | ** | 6 |
| Liu et al (2019) (31) | *** | ** | ** | 7 |
| Mah et al (2013) (32) | *** | ** | ** | 7 |
| Morris et al (2008) (33) | ** | ** | ** | 6 |
| Ronnebaum et al (2012) (34) | ** | ** | 4 | |
| Winkelman et al (2012)(37) | ** | ** | ** | 6 |
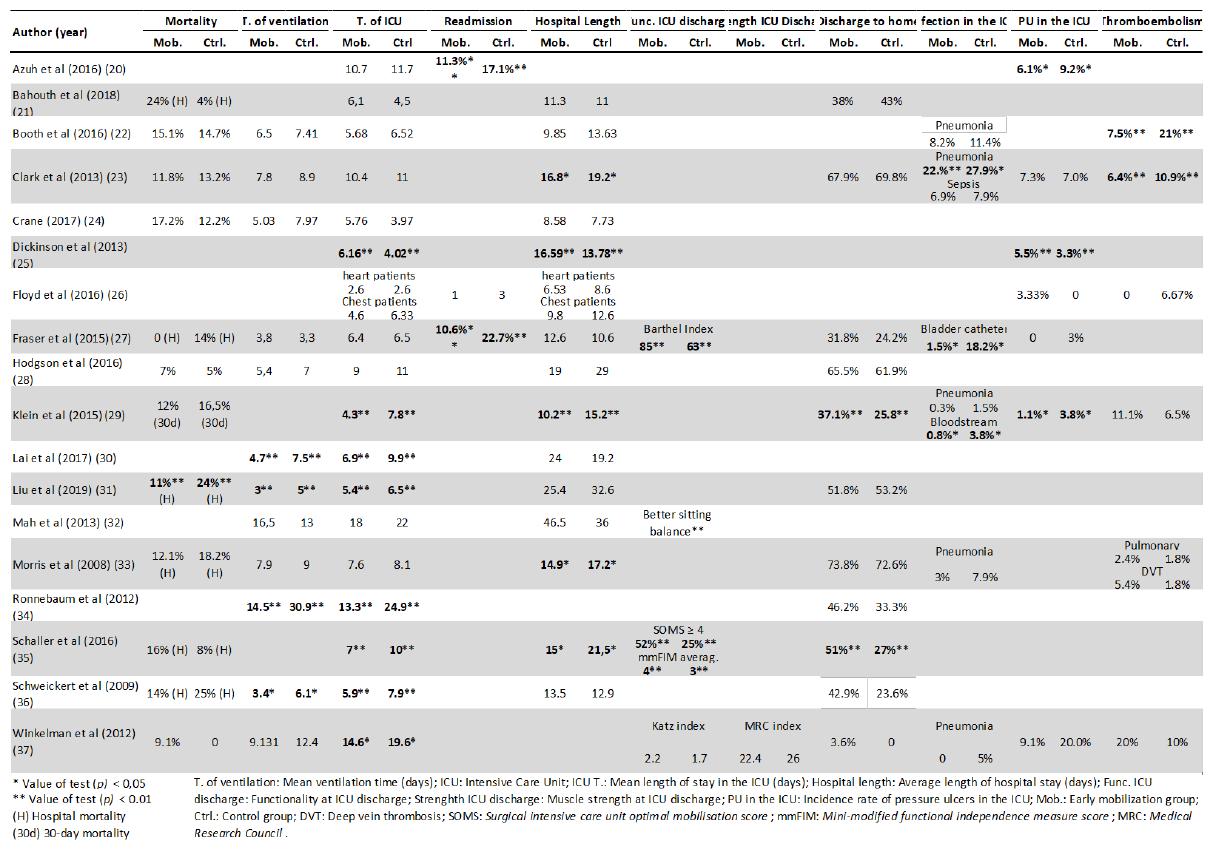
Mortality
Of the studies included in this review, 12 analyzed the topic mortality. Of these, five ones refer to ICU mortality22-24,28,37, six to in-hospital mortality20,27,31,33,35,36 and one presents 30-day mortality results29.
Analyzing Table 4, it can be seen that mortality in the ICU varied between 0 and 17.2%, with no significant differences being verified between the group of patients undergoing the mobilization program and the control group. Still, of the five studies that analyzed mortality in the ICU, four reported slightly higher mortality rates in the mobilization group.
With regard to hospital mortality, it varied between 0 and 25%. Only in an analysis of the results of a quality improvement project through the implementation of a progressive mobilization protocol 31, a significant reduction in hospital mortality was identified in patients submitted to the early mobilization program (11 vs 24%, p < 0 ,01). In three studies21,27,35 hospital mortality was higher in the mobilization group and in another 3 it was higher in the control group31,33,36.
With regard to 30-day mortality29, the mobilization group was 4.5% lower than the control group, although this difference cannot be considered significant (p = 0.12).
In none of the three RCTs under analysis 28,35,36 there are significant differences in mortality between groups.
Ventilation time
There are 12 articles that compare mean ventilation times between patients in an early mobilization program and usual treatment (Table 4). The mean ventilation times reported ranged between 331 and 30.934 days, with no significant increase in ventilation time associated with the development of early progressive mobilization programs being verified in any of the studies analyzed. On the other hand, in 10 of the analyzed studies, there was a reduction in ventilation time in the early progressive mobilization group, in relation to the control group, with statistically significant difference in four of them30,31,34,36.
The two randomized studies that analyzed this outcome28,36 both show a reduction in ventilation time in the early mobilization group, but only in one36 was this difference statistically significant.
ICU length of stay
The ICU length of stay presented by the different studies is quite heterogeneous, varying between 3.9724 and 24.934 days.
In 1520,22,23,26-37 of the 18 studies analyzed (Table 4) there was a reduction in the length of stay in the group of patients included in the mobilization program, in relation to the control group. Of these, in seven studies this difference is statistically significant29-31,34-37. On the other hand, in three studies21,24,25) the group of patients included in the mobilization program had a longer hospital stay than the control group, although only in one25 were these differences statistically significant.
In all three RCTs under analysis28,35,36 there was a reduction in the length of stay in the early mobilization group, compared to the control group, with this difference being statistically significant in one of the studies35.
Readmission in ICU
The definition of readmission varies in the different studies analyzed, one of them refers to hospital readmission of critically ill patients20, while the other two refer to readmission in the ICU within 30 days after discharge from that unit26,27. Despite this difference in concepts, in the three studies analyzed there is a reduction in the number of readmissions in the early mobilization group, with significant differences reported by two of them20,27.
Length of hospital stay
The average length of hospital stay was quite heterogeneous in the different studies under analysis, varying between 6.526 and 46.5 days32.
When the differences between groups were observed, it was also verified that the results are also heterogeneous. On the one hand, nine studies describe a reduction in the length of hospital stay in the early mobilization group22,23,26,28-31,33,35 and of these, four show significant differences in relation to the control group 23,29,33,35. On the other hand, six studies21,24,25,27,36 report an increase in the length of hospital stay in the early mobilization group, although only one study25 reports statistically significant difference.
Focusing the analysis on randomized studies28,35,36, the evidence remains inconsistent. Only one of the studies35 reports a significant reduction in hospitalization time in patients mobilized early.
ICU high functionality
Functionality upon discharge from the ICU, in addition to not being a frequently analyzed outcome, was measured in different ways in the various investigations that included it.
When evaluating the functionality through the Barthel index27, significantly better results were verified in the group of patients mobilized early (85 vs 63 points, with p<0.001). It was also found that more patients in the early mobilization group improved their sitting balance, from a first assessment to discharge (75% vs 36.7%, with p=0.008)32.
In the study that evaluated functionality through the Katz index37, there was also better functionality at discharge in the early mobilization group, however the differences were not statistically significant.
Regarding the only RCT that evaluated this outcome35, it was found that significantly more patients in the intervention group achieved the ability to walk, which corresponds to a score on the SOMS scale (Surgical intensive care unit Optimal Mobilization Score) equal to or greater than a 4 (52% vs 25%, with p<0.001) and that, on average, the levels of functionality at discharge, assessed by the mmFIM scale (mini-modified functional independence measure score) were significantly higher in patients included in the mobilization group early, a difference also observed by the authors at the time of hospital discharge.
In common, all studies identify functional improvements in the early mobilization group, in relation to the control.
Muscle strength at ICU discharge
Only one of the studies included in this review37 evaluated muscle strength at ICU discharge. For this purpose, the MRC Index was used from the bilateral evaluation of four muscle groups, in which strength was scored from 0 to 5, with a final score variable between 0 and 40. The average score did not show significant differences between the groups. of early mobilization (22.4 points) and the control (26 points), with p=0.643.
Discharge to home
Of the 11 studies included in the analysis, only one37 analyzed the destination for discharge from the ICU and not the destination for hospital discharge like the other investigations. Comparing the intervention groups with the respective controls, we found that in most studies the number of patients discharged home is greater in the early mobilization group, with two studies29,35 reporting significant differences.
Incidence of ICU-acquired infections
The articles included in this review, all of them using non-randomized groups, analyze possible effects of early mobilization on the incidence of the following infections: pneumonia22,23,33, ventilator-associated pneumonia29,37, urinary catheter-associated infection 27, bloodstream infection29 and sepsis23. In all areas analyzed, the early mobilization group had a lower rate of infection compared to the control group, with significant differences in the incidence of pneumonia23, urinary catheter-associated infection27 and bloodstream infections29.
Incidence of pressure ulcers
The incidence of pressure ulcers (PU) was an outcome evaluated in seven of the investigations included in this review, all of them non-randomized. Of these, four studies20,27,29,37 report a reduction in the incidence of PU in the early mobilization group, and two of them20,29 identify significant differences in relation to the control group. In addition, an article27 mentions a significant reduction in “quality outcomes” (which include: falls, ventilator-associated events, PU and urinary catheter-associated infections).
Otherwise, three studies23,25,26 refer to an increase in the incidence of PU in the group of patients mobilized early, and one of them25 identifies a significant increase in relation to patients in the control group.
Incidence of thromboembolic phenomena
Of the studies included in this review, six analyzed the incidence of thromboembolic phenomena, all of them non-randomized. Some studies analyzed thromboembolic events as a whole22,37, others analyzed the incidence of deep venous thrombosis and pulmonary embolism separately26,33, and other studies analyzed only the incidence of deep venous thrombosis23,29. From the analysis of the results, three studies that report a non-significant increase in thromboembolic events29,33,37 and three that report a reduction22,23,26. In two cases22,23 there were statistically significant differences, both favoring the early mobilization group.
DISCUSSION
If in the beginning of this review the benefits of early mobilization programs for critically ill patients were not clear, we have found in this article that programs can contribute to reducing ventilation time; reduction in the ICU length of stay; greater functionality at ICU discharge, regardless of the assessment instrument used. Although further research is needed, there also seems to be a trend towards increased likelihood of discharge to home, reduced readmissions and reduced ICU-acquired infections, namely urinary catheter-associated infections and bloodstream infections. No negative outcomes were found, which supports the idea that it is a safe practice, as long as it is adequate to the condition of each patient and the existing recommendations40.
Regarding ventilation time, the results of this review are in line with other reviews, which, although including different forms of mobilization and only RCTs, reached identical conclusions11,41. Also, a meta-analysis conducted by Wang, in 202042, including different mobilization strategies and only RCT, shows a significant reduction in ventilation time in patients mobilized early.
The ICU length of stay is also an outcome included in other reviews, which tend to identify reductions without statistical significance11,15,41,43,44. Once again Wang42, including a larger number of studies in his meta-analysis, manages to show an important reduction in the length of stay in the ICU in patients mobilized early.
With regard to functionality, two reviews consulted 11,12 cite only one study36 demonstrating significant improvements in the early mobilization group, but at hospital discharge and not at ICU discharge, as advocated in this review. Only the meta-analysis by Wang42 analyzed this outcome, reporting a significant increase in the Barthel index in the early mobilization group.
Two RCT reviews, both with meta-analysis, support the increase in home discharges in patients mobilized early41,45. Readmission was not considered in any other review consulted.
With regard to infections acquired in the ICU, the meta-analysis by Wang42 once again supports the results of this review, showing a significant reduction in the risk of ventilator-associated pneumonia in the group of patients undergoing early mobilization.
In this review, some contradictory results were detected between the included studies, namely with regard to the effect of early progressive mobilization programs on the incidence of thromboembolic phenomena, PU and also their effects in terms of mortality and length of hospital stay. In comparison, the review with meta-analysis conducted by Wang42 shows a significant reduction in the risk of deep venous thrombosis, in the incidence of PU and in the length of hospital stay, in patients mobilized early. With regard to mortality, it also does not identify significant differences between the groups. Still regarding the length of hospital stay, although in a meta-analysis involving patients after cardiac surgery44 no significant differences were detected between the early mobilization group and the usual treatment, another meta-analysis14 reports a significant reduction in this outcome in patients who start mobilization in the first week of ICU stay, reinforcing the importance of early mobilization.
Although the effect of early progressive mobilization programs on the muscle strength of patients at ICU discharge is not clear in this review, given that only one of the included studies reported this outcome, in the available literature, regarding early mobilization, its benefit in reducing generalized muscle weakness acquired in the ICU, especially in patients with longer hospital stays, usually associated with a significant incidence of this problem41,42. This is another outcome, which was not considered in this review and strictly related to early mobilization and the incidence of delirium, with mobilization considered a factor that contributed to the prevention of the occurrence of this phenomenon46.
In view of these results, it is clear that there is a need to change mentality and assume mobilization as a priority in the care of critically ill patients. There will certainly be more or less barriers in each service 47-49, but nurses and in particular rehabilitation nursing specialists, as experts in this area, must develop or streamline early mobilization protocols. In the international literature, the mobility champion is referred to as someone who performs these functions50,51. Looking at the national reality, at the availability and competence of rehabilitation nurses in the ICUs52,53, they should assume themselves as champions of mobility in their units.
Study limitations
This study had several limitations. First, the low proportion of randomized studies included in the analysis compared to observational studies. A significant number of historically controlled studies were included, and the results could be due to factors other than just the mobilization program. We also found discrepancies in the level of care provided to patients in the different control groups, which may give greater or lesser emphasis to the benefits of the program under analysis.
Contributions to the area
When it is compared with other previous reviews, this research, in addition to presenting an update of knowledge, is innovative for it concretely analyzes the effect of early progressive mobilization programs. Previous reviews refer to early mobilization more broadly, including different forms of early mobilization or rehabilitation.
As it’s evident in this article, early progressive mobilization programs are safe for patients, with no negative outcome resulting from their application.
The benefits found reinforce the importance of investing in this type of program and permanently change the paradigm of mobilization vs. immobilization of critically ill patients, where the rehabilitation nurse plays an important role. It is advisable to associate them with a wider range of interventions, such as the well-known ABCDEF bundle.
CONCLUSION
This review demonstrates the benefits of isolated early progressive mobilization programs in terms of reducing ventilation time and length of stay in intensive care. Patients included in these programs are also more functional at discharge and less likely to be readmitted. Allied to these benefits, no negative outcomes were found, reinforcing that this is a safe and beneficial practice.
In the complex care plan for critically ill patients, early mobilization should be included, preferably through a multidisciplinary program or protocol, consisting of several steps appropriate to their condition.
It is equally important to support this practice with results, which, in addition to making known what is done in each service, contribute to improving knowledge on this important topic.
REFERENCES
1 Ordem Enfermeiros. Guia orientador de boas práticas: Cuidados à pessoa com alterações da mobilidade - posicionamentos, transferências e treino de deambulação [Internet]. Ordem dos Enfermeiros; 2013. Disponível em: https://www.ordemenfermeiros.pt/media/8897/gobp_mobilidade_vf_site.pdf [ Links ]
2 Machado J, Castro M, Ceniccola G, Giacomassi I, Isola A, Silva Jr J, et al. Bundles do combate à fraqueza adquirida na unidade de terapia intensiva. BRASPEN J. 2021;36(2):131-75. [ Links ]
3 Voiriot G, Oualha M, Pierre A, Salmon-Gandonnière C, Gaudet A, Jouan Y, et al. Chronic critical illness and post-intensive care syndrome: from pathophysiology to clinical challenges. Annals of Intensive Care. 2022;12(1):1-14. Disponível em: https://doi.org/10.1186/s13613-022-01038-0 [ Links ]
4 Davidson J, Harvey M, Achuller J, Black G. Post-intensive care syndrome: what it is and how to help prevent it. Am Nurse Today. 2013;8(5):32-8. [ Links ]
5 Svenningsen H, Langhorn L, Ågård AS, Dreyer P. Post-ICU symptoms, consequences, and follow-up: an integrative review. Nurs Crit Care. 2017;22(4):212-20. Disponível em: https://doi.org/10.1111/nicc.12165 [ Links ]
6 Rawal G, Yadav S, Kumar R. Post-intensive care syndrome: an overview. J Transl Int Med. 2017;5(2):90-2. Disponível em: https://doi.org/10.1515/jtim-2016-0016 [ Links ]
7 Marra A, Ely EW, Pandharipande PP, Patel MB. The ABCDEF Bundle in critical care. Crit Care Clin. 2017;33(2):225-43. Disponível em: https://doi.org/10.1016/j.ccc.2016.12.005 [ Links ]
8 Pandharipande P, Banerjee A, McGrane S, EW E, Pandharipande P, Banerjee A, et al. Liberation and animation for ventilated ICU patients: the ABCDE bundle for the back-end of critical care. Crit Care. 2010;14(3):157. Disponível em: https://doi.org/10.1186/cc8999 [ Links ]
9 Gosselink R, Bott J, Johnson M, Dean E, Nava S, Norrenberg M, et al. Physiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill Patients. Intensive Care Medicine. 2008; 34(7):1188-99. Disponível em: https://doi.org/10.1007/s00134-008-1026-7 [ Links ]
10 Bein T, Bischoff M, Brückner U, Gebhardt K, Henzler D, Hermes C, et al. S2e guideline: positioning and early mobilisation in prophylaxis or therapy of pulmonary disorders : Revision 2015: S2e guideline of the German Society of Anaesthesiology and Intensive Care Medicine (DGAI). Anaesthesist]. 2015;64 Suppl 1:1-26. Disponível em: https://doi.org/10.1007/s00101-015-0071-1 [ Links ]
11 Castro-Avila AC, Serón P, Fan E, Gaete M, Mickan S. Effect of early rehabilitation during intensive care unit stay on functional status: Systematic review and meta-Analysis. PLoS One. 2015;10(7):e0130722. Disponível em: https://doi.org/10.1371/journal.pone.0130722 [ Links ]
12 Doiron KA, Hoffmann TC, Beller EM. Early intervention (mobilization or active exercise) for critically ill adults in the intensive care unit. Cochrane Database Syst Rev. 2018;3(3):CD010754. Disponível em: https://doi.org/10.1002/14651858.CD010754.pub2 [ Links ]
13 da Silva Pissolato J, Fleck CS. Mobilização precoce na unidade de terapia intensiva adulta. Fisioterapia Brasil. 2018;19(3):377-84. Disponível em: https://doi.org/10.33233/fb.v19i3.690 [ Links ]
14 Okada Y, Unoki T, Matsuishi Y, Egawa Y, Hayashida K, Inoue S. Early versus delayed mobilization for in-hospital mortality and health-related quality of life among critically ill patients: A systematic review and meta-analysis. J Intensive Care. 2019;7(1). Disponível em: https://doi.org/10.1186/s40560-019-0413-1 [ Links ]
15 Zhang L, Hu W, Cai Z, Liu J, Wu J, Deng Y, et al. Early mobilization of critically ill patients in the intensive care unit: A systematic review and meta-analysis. PLoS One. 2019;14(10). Disponível em: https://doi.org/10.1371/journal.pone.0223185 [ Links ]
16 Meyer MJ, Stanislaus AB, Lee J, Waak K, Ryan C, Saxena R, et al. Surgical Intensive Care Unit Optimal Mobilisation Score (SOMS) trial: a protocol for an international, multicentre, randomised controlled trial focused on goal-directed early mobilisation of surgical ICU patients. BMJ Open. 2013;3(8):e003262. Disponível em: http://dx.doi.org/10.1136/bmjopen-2013-003262 [ Links ]
17 Berry A, Beattie K, Bennett J, Cross CW, Cushway S, Hassan A, et al. Intensive Care NSW-Physical activity and movement-A guideline for critically ill adults: a Guideline for Critically Ill Adults [Internet]. Chatswood: Agency for Clinical Innovation; 2017 (Citado em: 2023 Abril 1). Disponível em: https://aci.health.nsw.gov.au/__data/assets/pdf_file/0005/239783/ACI-Physical-activity-movement-guideline-critically-ill-adults.pdf [ Links ]
18 Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (atualizado em 2022 Fev). Cochrane, 2022. Disponível em: www.training.cochrane.org/handbook [ Links ]
19 Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ (Online). 2009;339:b2535. Disponível em: https://doi.org/10.1136/bmj.b2535 [ Links ]
20 Azuh O, Gammon H, Burmeister C, Frega D, Nerenz D, DiGiovine B, et al. Benefits of early active mobility in the medical intensive care unit: A pilot study. American Journal of Medicine. 2016;129(8):866-871.e1. Disponível em: http://dx.doi.org/10.1016/j.amjmed.2016.03.032 [ Links ]
21 Bahouth MN, Power MC, Zink EK, Kozeniewski K, Kumble S, Deluzio S, et al. Safety and feasibility of a neuroscience critical care program to mobilize patients with primary intracerebral hemorrhage. Arch Phys Med Rehabil. 2018;99(6):1220-5. Disponível em: https://doi.org/10.1016/j.apmr.2018.01.034 [ Links ]
22 Booth K, Rivet J, Flici R, Harvey E, Hamill M, Hundley D, et al. Progressive mobility protocol reduces venous thromboembolism rate in trauma intensive care patients: A quality improvement project. J Trauma Nurs. 2016;23(5):284-9. Disponível em: https://doi.org/10.1097/JTN.0000000000000234 [ Links ]
23 Clark DE, Lowman JD, Griffin RL, Matthews HM, Reiff DA. Effectiveness of an early mobilization protocol in a trauma and burns intensive care unit: A retrospective cohort study. Phys Ther. 2013;93(2):186-96. Disponível em: https://doi.org/10.2522/ptj.20110417 [ Links ]
24 Crane AN. Implementing an early mobility protocol for patients in the Intensive care unit [Internet]. Dissertation - Doctor Nursing Practice. Brandman University Irvine, California. Disponível em: http://hdl.handle.net/10755/20635 [ Links ]
25 Dickinson S, Tschannen D, Shever LL. Can the use of an early mobility program reduce the incidence of pressure ulcers in a surgical critical care unit? Crit Care Nurs Q. 2013 Jan;36(1):127-40. Disponível em: https://doi.org/10.1097/CNQ.0b013e31827538a1 [ Links ]
26 Floyd S, Craig SW, Topley D, Tullmann D. Evaluation of a progressive mobility protocol in postoperative cardiothoracic surgical patients. Dimens Crit Care Nurs. 2016;35(5):277-82. Disponível em: https://doi.org/10.1097/DCC.0000000000000197 [ Links ]
27 Fraser D, Spiva L, Forman W, Hallen C. Implementation of an early mobility program in an ICU. Am J Nurs. 2015;115(12):49-58. Disponível em: https://doi.org/10.1097/01.NAJ.0000475292.27985.fc [ Links ]
28 Hodgson CL, Bailey M, Bellomo R, Berney S, Buhr H, Denehy L, et al. A binational multicenter pilot feasibility randomized controlled trial of early goal-directed mobilization in the ICU. Crit Care Med. 2016;44(6):1145-52. Disponível em: https://doi.org/10.1097/CCM.0000000000001643 [ Links ]
29 Klein K, Mulkey M, Bena JFJF, Albert NM. Clinical and psychological effects of early mobilization in patients treated in a neurologic ICU: a comparative study. Crit Care Med. 2015;43(4):865-73. Disponível em: https://doi.org/10.1097/CCM.0000000000000787 [ Links ]
30 Lai CC, Chou W, Chan KS, Cheng KC, Yuan KS, Chao CM, et al. Early mobilization reduces duration of mechanical ventilation and intensive care unit stay in patients with acute respiratory failure. Arch Phys Med Rehabil. 2017;98(5):931-9. Disponível em: https://doi.org/10.1016/j.apmr.2016.11.007 [ Links ]
31 Liu K, Ogura T, Takahashi K, Nakamura M, Ohtake H, Fujiduka K, et al. A progressive early mobilization program is significantly associated with clinical and economic improvement: A single-center quality comparison study. Crit Care Med. 2019;47(9):e744-52. Disponível em: https://doi.org/10.1097/CCM.0000000000003850 [ Links ]
32 Mah JW, Staff I, Fichandler D, Butler KL. Resource-efficient mobilization programs in the intensive care unit: Who stands to win? Am J Surg. 2013 Oct;206(4):488-93. Disponível em: https://doi.org/10.1016/j.amjsurg.2013.03.001 [ Links ]
33 Morris PE, Goad A, Thompson C, Taylor K, Harry B, Passmore L, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(8):2238-43. Disponível em: https://doi.org/10.1097/CCM.0b013e318180b90e [ Links ]
34 Ronnebaum J, Weir J, Ronnebaum JA, Weir JP, Hilsabeck TA. Earlier mobilization decreases the length of stay in the intensive care unit. Journal of Acute Care Physical Therapy 3(2):204-210. [ Links ]
35 Schaller SJ, Anstey M, Blobner M, Edrich T, Grabitz SD, Gradwohl-Matis I, et al. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. The Lancet. 2016;388(10052):1377-88. Disponível em: https://doi.org/10.1016/S0140-6736(16)31637-3 [ Links ]
36 Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 2009;373(9678):1874-1882. Disponível em: https://doi.org/10.1016/S0140-6736(09)60658-9 [ Links ]
37 Winkelman C, Johnson KD, Hejal R, Gordon NH, Rowbottom J, Daly J, et al. Examining the positive effects of exercise in intubated adults in ICU: a prospective repeated measures clinical study. Intensive Crit Care Nurs. 2012;28(6):307-18. Disponível em: https://doi.org/10.1016/j.iccn.2012.02.007 [ Links ]
38 Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses [Internet]. [citado 2023 Abril 1]. Disponível em: https://www.ohri.ca//programs/clinical_epidemiology/oxford.asp [ Links ]
39 Higins J, Savovic J, Page M, Elbers R, Sterne J. Assessing risk of bias in a randomized trial. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (atualizado em 2022 Fev). Cochrane, 2022. Disponível em: https://training.cochrane.org/handbook/current/chapter-08 [ Links ]
40 Hodgson CL, Stiller K, Needham DM, Tipping CJ, Harrold M, Baldwin CE, et al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Crit Care. 2014;18(6):658. Disponível em: https://doi.org/10.1186/s13054-014-0658-y [ Links ]
41 Anekwe DE, Biswas S, Bussières A, Spahija J. Early rehabilitation reduces the likelihood of developing intensive care unit-acquired weakness: a systematic review and meta-analysis. Physiotherapy. 2020;107:1-10. Disponível em: https://doi.org/10.1016/j.physio.2019.12.004 [ Links ]
42 Wang J, Ren D, Liu Y, Wang Y, Zhang B, Xiao Q. Effects of early mobilization on the prognosis of critically ill patients: A systematic review and meta-analysis. Int J Nurs Stud. 2020;110:103708. Disponível em: https://doi.org/10.1016/j.ijnurstu.2020.103708 [ Links ]
43 Zayed Y, Kheiri B, Barbarawi M, Chahine A, Rashdan L, Chintalapati S, et al. Effects of neuromuscular electrical stimulation in critically ill patients: A systematic review and meta-analysis of randomised controlled trials. Aust Crit Care. 2019 33(2):203-210. Disponível em: https://doi.org/10.1016/j.aucc.2019.04.003 [ Links ]
44 Chen B, Xie G, Lin Y, Chen L, Lin Z, You X, et al. A systematic review and meta-analysis of the effects of early mobilization therapy in patients after cardiac surgery. Medicine. 2021;100(15):e25314. Disponível em: https://doi.org/10.1097/MD.0000000000018843 [ Links ]
45 Zang K, Chen B, Wang M, Chen D, Hui L, Guo S, et al. The effect of early mobilization in critically ill patients: A meta-analysis. Nurs Crit Care. 2020;25(6):360-367. Disponível em: https://doi.org/10.1111/nicc.12455 [ Links ]
46 Mart MF, Williams Roberson S, Salas B, Pandharipande PP, Ely EW. Prevention and management of delirium in the intensive care unit. Semin Respir Crit Care Med. 2021;42(1):112-26. Disponível em: https://doi.org/10.1055/s-0040-1710572 [ Links ]
47 Dirkes SM, Kozlowski C. Early mobility in the intensive care unit: Evidence, barriers, and future directions. Crit Care Nurse. 2019;39(3):33-42. Disponível em: https://doi.org/10.4037/ccn2019654 [ Links ]
48 Harrold ME, Salisbury LG, Webb SA, Allison GT, Australia and Scotland ICU Physiotherapy Collaboration. Early mobilisation in intensive care units in Australia and Scotland: a prospective, observational cohort study examining mobilisation practises and barriers. Crit Care. 2015;19(1):336. Disponível em: https://doi.org/10.1186/s13054-015-1033-3 [ Links ]
49 Leditschke A, Green M, Irvine J, Bissett B, Mitchell IA. What are the barriers to mobilizing intensive care patients? Cardiopulm Phys Ther J. 2012;23(1):26-9. [ Links ]
50 Esteban AR, Espejo J, Estrera-Portal R, Plummer BJ. Unit-based early progressive mobility champion. Crit Care Nurse. 2014;34(2):e7-e7. [ Links ]
51 Bruce R. Integrating a mobility champion in the intensive care unit. Dimens Crit Care Nurs. 2018;37(4):201-209. Disponível em: https://doi.org/10.1097/DCC.0000000000000306 [ Links ]
52 Mendes R, Nunes L, Pinho JA, Gonçalves R. Organização dos cuidados de reabilitação nas unidades de cuidados intensivos portuguesas. Rev Bras Ter Intensiva. 2018;30(1):57-63. Disponível em: https://doi.org/10.5935/0103-507X.20180011 [ Links ]
53 Mendes R, Nunes M. A importância da enfermagem de reabilitação nas unidades de cuidados intensivos portuguesas. Rev Port Enf Reab. 2018;1(2):8-13. Disponível em: https://doi.org/10.33194/rper.2018.v1.n2.01.4406 [ Links ]
Received: January 26, 2023; Accepted: June 19, 2023; Published: June 30, 2023











 texto en
texto en