Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Portuguesa de Enfermagem de Reabilitação
Print version ISSN 2184-965XOn-line version ISSN 2184-3023
RPER vol.6 no.1 Silvalde June 2023 Epub June 30, 2023
https://doi.org/10.33194/rper.2023.313
Literature review
The impact of gait rehabilitation programs on length of hospital stay - Scoping Review
1Centro Hospitalar do Porto, Porto, Portugal
Introduction:
Prolonged hospitalization and lack of activity during hospitalization are associated with functional decline, greater complications and increased health care costs. Gait programs are strategies to promote mobility levels that can reverse these outcomes. This study aims to map the literature on the impact of gait programs on the length of hospital stay.
Methodology:
Scoping review based on the Joanna Briggs Institute model. The formulation of the research question was based on the acronym PCC - population: inpatients; concept: gait programs with impact on length of stay; context: hospital. The search was conducted in the PubMed, Scielo and PsyInfo databases, being limited to articles written in Portuguese and English, published between 2017 and 2022.
Results:
From the 53 studies identified, 24 were included in the review. We found gait programs in different hospital inpatient settings, included in multimodal intervention protocols, in global exercise programs that include gait and in exclusive gait programs. It was found that walking programs have an impact on clinical and non-clinical indicators, reflected in the length of hospital stay. One-third of the articles reviewed concluded that walking programs reduce hospital stay between 1 to 3 days.
Conclusion:
Gait programs are inexpensive strategies, feasible in a hospital setting, that improve mobility levels, functionality, and may be associated with shorter hospital stays.
DESCRIPTORS: Gait; hospitals; length of stay
Introdução:
O internamento prolongado e a falta de atividade durante a hospitalização estão associados a um declínio funcional, maiores complicações e a um aumento dos custos em saúde. Os programas de marcha são estratégias promotoras de níveis de mobilidade que permitem inverter estes resultados. Com este estudo pretende-se mapear a literatura sobre o impacto de programas de marcha no tempo de internamento hospitalar.
Método:
Revisão do tipo scoping baseada no modelo do Instituto Joanna Briggs. A formulação da questão de investigação baseou-se no acrónimo PCC - população: pessoas internadas; conceito: programas de marcha, com impacto no tempo de internamento; contexto: hospital. A pesquisa foi realizada nas bases de dados PubMed, Scielo e PsyInfo, limitando-se a artigos redigidos em português e inglês, no intervalo temporal 2017 a 2022.
Resultados:
Dos 53 estudos identificados, 24 incluíram-se na revisão. Foram encontrados programas de marcha em diferentes contextos de internamento hospitalar, inseridos em protocolos de intervenção multimodal, em programas de exercícios globais que incluem a marcha e em programas exclusivos de marcha. Verificou-se que programas de marcha têm impacto em indicadores clínicos e não clínicos, refletindo-se no tempo de internamento. Um terço dos artigos analisados concluem que os programas de marcha reduzem a estadia hospitalar entre 1 a 3 dias.
Conclusão:
Os programas de marcha são estratégias pouco dispendiosas, exequíveis em ambiente hospitalar, que melhoram níveis de mobilidade, funcionalidade e podem estar associados a menor tempo de internamento.
DESCRITORES: Marcha; hospitais; tempo de internamento
Introducción:
La hospitalización prolongada y la falta de actividad durante la misma se asocian a deterioro funcional, mayores complicaciones y aumento de los costes sanitarios. Los programas de marcha son estrategias que promueven niveles de movilidad que permiten revertir estos resultados. Este estudio pretende hacer un mapeo de la literatura sobre el impacto de los programas de marcha en la duración de la estancia hospitalaria.
Metodología:
Revisión de alcance basada en el modelo del Instituto Joanna Briggs. La formulación de la pregunta de investigación se basó en el acrónimo PCC - población: pacientes hospitalizados; concepto: programas de marcha con impacto en la duración de la estancia hospitalaria; contexto: hospital. La búsqueda se realizó en las bases de datos PubMed, Scielo y PsyInfo, limitándose a artículos escritos en portugués e inglés, en el intervalo de tiempo 2017 a 2022.
Resultados:
De los 53 estudios identificados, 24 se incluyeron en la revisión. Se encontraron programas de marcha en diferentes ámbitos de hospitalización, incluidos en protocolos de intervención multimodal, en programas globales de ejercicio que incluyen la marcha y en programas exclusivos de marcha. Se encontró que los programas de marcha tienen un impacto en los indicadores clínicos y no clínicos, reflejados en la duración de la estancia hospitalaria. Un tercio de los artículos analizados concluyó que los programas de marcha reducen la estancia hospitalaria entre 1 e 3 días.
Conclusión:
Los programas de marcha son estrategias baratas, viables en entornos hospitalarios, que mejoran los niveles de movilidad y funcionalidad y pueden asociarse a estancias hospitalarias más cortas.
DESCRIPTORES: Marcha; hospitales; tiempo de internación
Introduction
The last few years have brought numerous challenges to health in Portugal, in terms of changing the country's demographic and epidemiological profile, the generalization of population access to quality health care, a strong technological evolution, but also in terms of efficiency and control of public expenditure. This balance, associated with the worsening of the economic and social situation, determines an additional effort to guarantee the efficiency and effectiveness of the health system1.
The length of stay has an impact on hospital management due to the high costs associated with each episode in the various specialties and also due to the incidence of adverse events, which compromise patient safety, such as the risk of infection, falls or other problems unrelated to the main diagnosis (2. The average length of stay in hospitals is often used as an indicator of efficiency, as in identical circumstances, a shorter stay will reduce the cost per discharge, making it possible to ensure continuity of care using less expensive post-hospital settings (3.
Prolonged hospitalization and lack of activity during hospitalization are associated with a functional decline in more vulnerable people4. Just five days of bed rest can cause a loss of muscle mass of around 1 kg, contributing to the appearance of the disuse syndrome5. Eight or more days of hospitalization are associated with a significant loss of muscle mass and a loss of strength of approximately 7.5 newtons in both sexes6. In people with walking ability, the periods of activity in a hospital environment are also very reduced. It is estimated that the median frequency of walking in hospitalized patients is 5.5 minutes per day, being similar between independent and help-dependent people7. Elderly people who are able to walk upon admission, when admitted to a medical service, can spend 17 hours a day in bed8. In addition to immobility, there is a cumulative effect of hospitalization, illness, comorbidities and frailty.
There is evidence that rehabilitation care is effective in reducing mortality and morbidity, preventing complications, improving functional capacity and quality of life9-11. However, the economic impact of this care is still not very visible. Thus, the objective of this review is to map the literature on the impact of walking programs on the length of hospital stay. Throughout this study, it is intended to answer the research question “Which gait programs have an impact on the length of hospital stay?”
Methodology
A scoping-type review was prepared considering the guidelines defined by the Joanna Briggs Institute (JBI) for this type of scientific literature review12. The option for this methodological strategy is based on the need to carry out a preliminary analysis, for a study to be carried out, which will seek to know the economic impact of a gait rehabilitation program developed by nurses in an University Hospital.
The formulation of the research question was based on the acronym PCC (Population, Concept and Context). Thus, as a population, all hospitalized people were considered. The concept includes gait programs, with an impact on the length of stay, with the context being the hospital.
In accordance with the JBI recommendations, the development and implementation of the research strategy took place in three stages, having been carried out in October 2022, in the PubMed, Scielo and PsyInfo databases, limited to articles written in Portuguese and English, published between 2017 and 2022. The Boolean phrase - “(walking or gait or locomotion) and (length of stay) and hospital” was created from the combination of descriptors/medical subject headings (MeSH) and was used in all databases previously described data. An article was also added outside this data search, which is important for the purposes of the study. Walking, according to the International Council of Nursing, is defined as “mobilizing: movement of the body from one place to another, moving the legs step by step; ability to support body weight and walk with an effective gait, with speeds ranging from slow to moderate or fast; going up or down stairs and ramps”13. By descriptors in health sciences, gait is the way or style of walking, locomotion is the movement or ability to move from one side to the other, and walking is the intentional locomotion to get somewhere14. Due to the semantic similarity, throughout the text, all these terms are used as synonyms.
With regard to the type of sources, quantitative, qualitative and mixed studies that respond to the research question were considered. Book chapters and opinion articles were excluded from the review.
The selection of articles was a rigorous and systematic process. Using EndNote software, duplicate studies were eliminated. The Rayyan software enabled a new step of removing repeated data. With this program, two researchers independently and blindly selected articles by title and abstract. Consensus meetings served to reach agreement among researchers on which articles met inclusion criteria. In a second step, the selected articles were fully read and their suitability for the study was confirmed. The reason for exclusion was methodically recorded.
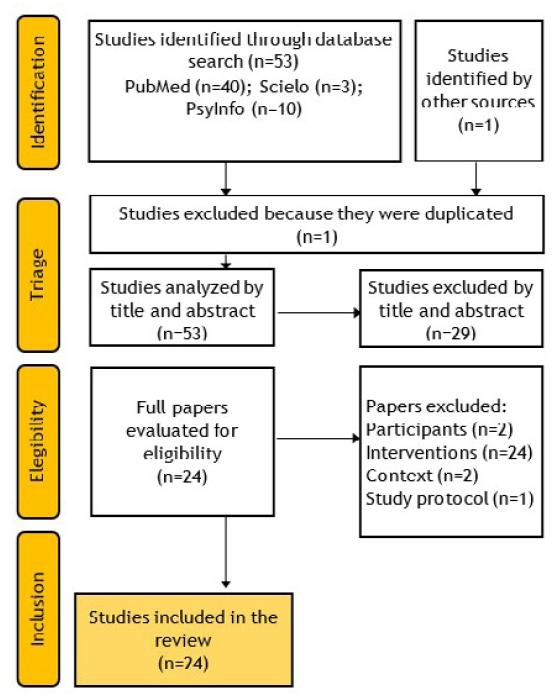
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) model served as the basis for organizing the information and the recommendations presented in the PRISMA-ScR (PRISMA Extension for Scoping Reviews) were also followed for the writing of this paper15.
The Prisma® diagram (Figure 1) summarizes the entire process of identification, screening, eligibility and inclusion of articles. A data extraction table was prepared, which includes the author of the article, year, location, type of study, objective, participants, intervention, the respective results and conclusions obtained. Subsequently, the data were analyzed and grouped in order to meet the purposes that guided this research. The protocol for this Scoping Review is registered on the Open Science Framework (OSF) platform with the identifier https://doi.org/10.17605/OSF.IO/XWDB6.
Results
The databases search identified 53 scientific papers. After the various selection steps (Figure 1), 24 papers were included in the review. The publications took place between 2017 and 2022, with around 42% of the papers produced in 2020, in the middle of the pandemic. A quarter of the studies come from North America16-24; although there is scientific production from European25-29, Asian30-34, South American35-38, and Oceania39 countries. Regarding typology, 18 of the 24 studies were randomized clinical trials16-21,26-33,36,38-40, two are literature reviews23,37, and four are observational studies22,24,34,35.
The scientific papers were analyzed and grouped in different contexts, according to the care needs and pathologies of 9,540 participants that led to hospitalization. Gait programs have been found in people undergoing colorectal16,18,30, gynecological19,26, urological21, cardiothoracic31,37,38, hip32,33,36 and of column23. In non-surgical patients, programs implemented in acute medical 17,25,27 and neurology 22,29 settings, were also identified. Early walking was a strategy used in the different phases of hospitalization, from intensive care24,28 to rehabilitation units20,34,35,39.
Despite the variability of the programs, all address gait issues, having been grouped into three categories, multimodal intervention programs18,19,22,23,26,30,31,34,35, such as the ERAS protocol, which are characterized by an integrated approach involving different health professionals in a perspective of perioperative optimization, controlling aspects such as pain, risk of thromboembolism, fasting time, gastrointestinal function and early mobilization; exercise programs24,25,28,29,32,36-39 which, in addition to walking, include balance training activities, muscle strength, resistance, among others; and exclusive gait programs, namely assisted gait16,17,27, suspended gait20 walking by objectives33 and under financial incentive21.
Multidisciplinarity is a characteristic that cuts across most of the studies included in this review, with nurses, doctors and physiotherapists being the most highlighted professionals. Despite the results of this research not reporting directly to the rehabilitation nurse, several studies refer to nurses specialized in gait techniques. Different gait programs, in different contexts and moments of care activity, have shown to have an impact on the length of hospital stay. Clinical and economic indicators were also considered in the analysis of the results.
In most studies, the length of stay is similar between the intervention groups and the control groups16-18,21,25,27-29,32,33,38,39; however, one third of the articles analyzed conclude that gait programs reduce overall hospitalization time by between 1 and 3 days19,23,24,26,30,31,36,37. Only two showed an increase in hospitalization time20,35, which is associated with people with more serious health conditions. At the same time, three surveys demonstrated a reduction in the length of stay in intensive care24,37,38. Early walking was shown to be safe, not leading to a higher incidence of clinical complications16,18,23,31,33,36,37, even contributing to its reduction26,30,37. In turn, the mortality rate24,27,28,30,37,39 and hospital readmission18,19,23,26,28 were not influenced. After this intervention, patients were more likely to go home after hospital discharge32. Overall, the direct costs associated with hospitalizations, which included walking programs, were lower30.
A lower risk of falls35 and pressure injuries27, hospital indicators of patient safety and quality of care, were results associated with the implementation of gait programs that reflect gains in body balance32, in muscle strength 22,35,36, mobility24,25 and functional capacity17,23,28,32,35. A greater number of daily steps17 and better gait performance were also observed20,22,27,32,35, a predictor of greater mobility in the living space34. At the psychological level, the effects of this intervention are well documented, improving cognition28, reducing anxiety24,29,32, pain32, depressive states of the person or caregiver24,28,29, translating into greater satisfaction with health care19,26,32.
Table 1 Articles in analysis
| Author | Aim | Intervention | Outcome Measures (GC - Control Group; GI - Intervention Group) |
Conclusions |
|---|---|---|---|---|
| Balvardi et al. 202016 | To estimate the effect of early mobilization on lung function after colorectal surgery | Walking program using professionals exclusively for this purpose | Length of stay - similar in GC and GI. Immediate postoperative pulmonary complications - the mean time to diagnosis was less than 1 day. Postoperative pulmonary complications at 30 days similar in GC and GI. Functional capacity - similar in GC and GI. Respiratory function - similar in GC and GI. Gastrointestinal function - similar in GC and GI. |
Mobilization and walking assistance, with the allocation of extra resources, had a similar effect on lung function, complications, and length of stay after colorectal surgery. |
| Carli et al., 202018 | To compare the effect of a preoperative rehabilitation program with usual postoperative care in colorectal surgery | Preoperative 4-week multimodal rehabilitation program | Length of stay - similar in GC and GI. Readmission to the emergency department - similar in GC and GI. Postoperative complications - similar in GC and GI. Functional capacity - similar in GC and GI. |
A preoperative gait and rehabilitation protocol did not affect outcome measures compared with a postoperative rehabilitation program in colorectal surgery. |
| Chen et al., 202230 | To evaluate the effect of a walking program complemented with respiratory rehabilitation before and after colorectal surgery | Multimodal rehabilitation program (ERAS protocol) complemented with respiratory rehabilitation | Length of stay - decreased in GI by 2 days (p<0.001). Hospital costs - decreased in GI by €4227 (p<0.05). Postoperative complications - decreased in GI. Postoperative mortality - similar in GC and GI. |
The association of breathing exercises with the ERAS multimodal protocol, which includes walking, has an impact on reducing hospital costs and length of stay after colorectal surgery. |
| Ferrari et al., 202026 | To evaluate the impact of the ERAS protocol on the length of stay in gynecological surgery | Multimodal rehabilitation program (ERAS protocol) | Length of stay - decreased in GI by 3.3 days (p < 0.001). Readmission to the emergency department - similar in GC and GI. Postoperative complications - decreased in GI (p=0.027). Satisfaction - increased in GI (p<0.001). |
The ERAS protocol, which includes walking, allows for a significant reduction in hospital stay and postoperative complications in gynecological surgery. |
| Johnson et al., 201919 | To evaluate the impact of the ERAS protocol in gynecological surgery | Multimodal rehabilitation program (ERAS protocol) | Length of stay - one day for 21/25 people in GI vs. 17/25 in GC. Readmission to the emergency department - similar in GC and GI. Satisfaction - 100% of people in the GI evaluated walking as a contribution to their recovery vs. 96% of the GC. |
The ERAS protocol, which includes walking, can minimize complications and accelerate recovery in women undergoing gynecological surgery. |
| Cui et al., 202031 | To evaluate the effect of early mobility integrated into the ERAS protocol in cardiothoracic surgery | Multimodal rehabilitation program (ERAS protocol) with ultra-early gait | Length of stay - decreased by about 1 day in GI (p=0.031). Length of stay in intensive care - similar in GC and GI. Postoperative complications - similar in GC and GI. |
An early mobility program associated with the ERAS protocol, which includes walking, can reduce hospitalization time, complications and accelerate recovery after cardiac revascularization. |
| Oliveira et al., 202037 | To evaluate the efficacy and safety of rehabilitation in people with asymptomatic aortic aneurysms | Review with meta-analysis of 5 randomized studies | Length of stay - decreased in GI in a pre- and post-operative exercise program (MD, -0.69; 95% CI, -1.24 to -0.14). Length of stay in intensive care - decreased in GI in a 6-week exercise program (MD, -1.00; 95% CI, -1.26 to -0.74). Postoperative complications - decreased in GI in a 6-week exercise program (RR, 0.54 95% CI, 0.31-0.93). Mortality rate - similar in GC and GI. Functional capacity - similar in GI and GC in a pre- and postoperative exercise program. Aneurysm rupture - absent. |
An exercise program, which includes walking, makes it possible to prevent postoperative complications and reduce hospitalization time in people with asymptomatic aortic aneurysms. |
| Windmöller et al., 202038 | To evaluate the effectiveness of exercise with cycle ergometer combined with non-invasive ventilation (CPAP) after cardiothoracic surgery | Dynamic exercise program including walking and cycle ergometer combined with CPAP | Length of stay - similar in GC and GI. Length of stay in intensive care - decreased in GI (p=0.050). Functional capacity - similar in GC and GI. Respiratory function - similar in GC and GI. |
An exercise program with walking and cycle ergometer combined with CPAP, in people undergoing cardiac revascularization allows maintaining functional capacity and reducing the length of stay in intensive care, with an impact on the final cost of hospitalization. |
| Marchisio et al., 202036 | To evaluate the effect of an ultra-early and more intensive rehabilitation program after hip surgery | Early mobility exercise program | Length of stay - decreased in GI by 1 day (p=0.002). Postoperative complications - similar in GC and GI. Muscle strength - increased in GI. Pain - similar in GC and GI. |
The early start of a more intensive rehabilitation program, which includes walking, allows for an improvement in functional capacity and a decrease in hospital stay after hip surgery. |
| Pinskiy, Lubovsky & Kalichman, 202132 | To determine the effect of a health education program on exercise in hip surgery | Structured education session on preoperative rehabilitation exercises | Length of stay - similar in GC and GI. Discharge destination for home - increased in GI (p=0.001). Functional capacity - Increased in GI (p<0.05) Walking ability - increased in GI (p=0.005). Balance - increased in GI (p=0.005). Pain - decreased in GI (p=0.041). Postoperative anxiety - decreased in GI (p<0.001). Satisfaction - increased in GI (p=0.003). |
A structured exercise and gait education program preoperatively for total hip arthroplasty promotes faster recovery, decreases pain and anxiety, and promotes greater satisfaction. |
| Su et al., 202133 | To evaluate the safety and efficacy of walking in bone remodeling after hip surgery | Higher intensity walking program | Length of stay - similar in GC and GI. Functional capacity - similar in GC and GI Bone remodeling - similar in GC and GI. |
Higher intensity walking has benefits in bone remodeling after hip surgery, however, without significant impact on functional recovery. |
| Strother, et al. 202121 | To determine the impact of financial incentives on post-radical cystectomy gait | March program under financial incentive | Length of stay - similar in GC and GI. Daily steps - similar in GC and GI. |
Financial incentive had no impact on gait goals in people after radical cystectomy. |
| Braun et al., 201925 | Avaliar o impacto de um programa de marcha de maior intensidade na mobilidade em idosos | Higher intensity walking program | Length of stay - similar in GC and IG. Gait speed - similar in GC and GI. Balance: similar in GC and GI. Resistance: similar in GC and GI. Mobility - similar in GC and IG. |
A higher-intensity walking program had the same effect as usual care in elderly with acute illness. |
| Gazineo et al., 202027 | To evaluate the effects of an assisted walking program in the elders | Assisted Walking Program | Length of stay - similar in GC and GI. Walking ability - improved in GI (p<0.001). Incidence of falls - similar in GC and GI. Pressure injury risk - improved in GI (p<0.001). Mortality - similar in GC and GI. |
An individualized assisted walking intervention improves walking ability in older adults at discharge. |
| Hamilton et al., 201917 | To evaluate the effects of an assisted walking program in the elders | Assisted Walking Program | Length of stay - similar in GC and GI. Fate after discharge - similar in GC and GI. The threshold of 400 daily steps was found to be a predictor of home discharge (p=0.01). Daily steps - increased in GI (p=0.04). Functional capacity - increased in GI (p=0.04). |
An assisted walking program increased the number of daily steps and the functional capacity of the elderly people. |
| Lura et al., 201920 | To evaluate the effectiveness of suspended gait training in post-stroke rehabilitation | Suspension gait training | Length of stay - increased in GI by 5.4 days (p=0.03), associated with a lower level of functional capacity of people upon admission. Gait speed - increased in GI (p=0.02). |
Suspension gait training had a similar effect to conventional gait training in the rehabilitation of people with stroke. |
| Imamura et al., 202135 | To describe demographic, clinical and functional characteristics in post-COVID patients under rehabilitation program | Multimodal rehabilitation program | Length of stay - positive correlation between functional capacity and rehabilitation time in hospital. Walking ability - improved (p<0.01). Functional capacity - improved (p<0.0001). Muscle strength - improved (p<0.01). |
The rehabilitation program that includes walking improved the functional capacity, muscle strength and walking ability of people in the post-acute phase of COVID-19 infection. |
| Nakao et al., 202034 | To determine predictors of mobility in people with stroke | No intervention | Length of stay, female gender, age, cognitive and functional capacity, walking ability, balance and self-efficacy in preventing falls are predictors with a positive association with mobility 2 months after discharge (p<0.001). Motor function (p<0.0001) had a greater influence than cognitive performance on functional capacity. |
Older people, with longer hospital stays, less functional independence and less walking ability, have less mobility. |
| Li et al., 202039 | To evaluate the effectiveness of an app-based exercise program | App-based exercise program | Length of stay - similar in GC and IG. Gait speed - similar in GC and GI. Balance - similar in GC and GI. Resistance - similar in GC and GI. Functional capacity - similar in GC and IG. |
An exercise program that includes walking, through an application, has a similar effect on functional outcomes and length of hospital stay when compared to usual care. |
| Vloothuis, et al., 201929 | To evaluate the effect of an exercise program in digital support mediated by caregivers | Caregiver-mediated digital home exercise program (hospital-based) | Length of stay - similar in GC and GI. Walking ability - similar in GC and GI. Balance - similar in GC and GI. Functional capacity - similar in GC and GI. Anxiety - decreased in GI at 8 and 12 weeks (p=0.023; p=0.009). Caregiver depression - decreased in GI at 8 weeks (p=0.003). |
The program is feasible to be applied with caregivers. Despite having a similar effect on mobility, functional outcomes and length of stay, the intervention had a positive impact on secondary outcome measures such as anxiety and depression. |
| Attabib et al., 202122 | To determine predictors of motor and sphincter function after cauda equina injury | No intervention | Length of stay - early initiation of rehabilitation was associated with a shorter length of stay (p=0.03). Walking ability - early admission to rehabilitation was a predictor of improvement in walking ability (p = 0.0008). Bowel and bladder function - early admission to rehabilitation was a predictor of improved bowel (p=0.005) and bladder (p=0.0013) function. |
Rehabilitation improved walking ability and management of bladder and bowel elimination in people with cauda equina injury. |
| Elsarrag et al., 201923 | To determine the benefits of implementing the ERAS protocol in spine surgery | Multimodal intervention program | Length of stay - decreased in GI. Readmission to the emergency department - similar in CG and IG. Postoperative complications - similar in GC and GI. |
The ERAS protocol, which includes walking, has benefits in terms of functional capacity with an impact on reducing the length of stay in spine surgery. |
| Klein et al., 201824 | To determine the impact of an early mobility program in a neurological intensive care unit | Early mobility exercise program | Length of stay - decreased in GI by 2.66 days (p<0.001). Length of stay in intensive care units - decreased in IG (p<0.001). Discharge destination for home - similar in GC and IG. Mobility - increased in GI (p=0.014). Depression - decreased in GI (p<0.001). Anxiety - decreased in GI (p=0.003). Hostility - decreased in GI (p<0.001). Mortality - similar in GC and GI. |
The early rehabilitation program, which includes walking, increased mobility levels immediately and 12 months after the intervention, with reduced length of stay in intensive care and hospital. |
| Martínez-Velilla et al., 201928 | To evaluate the effect of exercise on functional decline in hospitalized elderly | Resistance, balance and gait exercise program | Length of stay - similar in GC and GI. Readmission to the emergency department - similar in GC and GI. Functional capacity - increased in GI (p<0.001). Incidence of falls - similar in GC and GI. Cognitive capacity - increased in GI (p<0.001). Depression - decreases in GI (p<0.001). Mortality - similar in GC and GI. |
The individualized exercise program, including walking, was shown to be safe and effective in reversing the functional decline associated with acute hospitalization in very elderly patients. |
Discussion
Health resources in an acute context are a precious and expensive asset, so reducing the length of hospital stay is an objective in health economics. Rehabilitation care provided in these settings not only reduces hospitalization time, but also reduces avoidable complications, improving health outcomes for the user and family41.
The ability to walk is an important health indicator, having already been proposed by several authors, since 2009, as the sixth functional vital sign28,42,43. As it was possible to verify in this review, the literature has shown important correlations between walking ability and health outcomes such as mortality, morbidity, complications and quality of life. Walking is a basic activity, necessary for carrying out the various self-care tasks, as it relates to individual levels of independence42,44.
The functional decline associated with hospitalization is a reality, and it is possible through mobility strategies to reverse these results27,28. There are barriers related to the person's health condition, such as pain, medical devices, physical weakness21 and health professionals, who often neglect gait assistance due to other concurrent clinical activities17. A study carried out in a public university hospital in Portugal, with 91 elderly patients admitted to an acute medicine unit, found a functional decline of 63.7% at discharge compared to the previous level of autonomy, measured 2 weeks before hospital admission( 4). Another investigation involving 503 hospitalized elderly patients found an incidence of iatrogenic disability of 11.9%. Of the total cases of disability, 81.7% were considered potentially preventable, with mobility incentive programs and shorter bed rest45. There is additional evidence that hospitalized people who walk in the corridors daily have a lower risk of dependence in activities of daily living and in instrumental activities during and after hospitalization46. The findings bring the possibility of a change from the traditional approach focused on the disease and the affectation, to a new perspective that recognizes the functional status as a clinical vital sign, which can be harmed by hospitalization28.
The gait programs are assumed as a strategy to promote levels of mobility and functional capacity that are easily achievable in a hospital environment, since in some cases they are based on simple interventions, in the domain of self-care and that do not require too expensive resources. Walking is considered one of the most common and accessible ways to exercise47. Specialized intervention in gait is reserved for people with clinical complexity and duly identified deficits48, in which, although the expenses may be higher in an initial phase of the treatment, the investment is recovered in a few months with the reduction of expenses in health41,42. In inpatient areas dedicated to rehabilitation, a positive relationship was established between length of stay and functional recovery20,35. Additionally, early access to rehabilitation care boosted a faster recovery22. Also in Portugal, a mobility program developed by rehabilitation nurses for hospitalized elderly people had a positive impact on balance, gait and functional independence, recognizing the advantage of these professionals' work in an acute context49. Rehabilitation nurses can lead walking programs and contribute to the multidisciplinary team's awareness of maintaining inpatients’ walking ability.
This research highlighted the importance given to gait incorporated in multimodal approaches, as it is difficult in these situations to attribute a direct causal relationship between the benefits obtained and the costs associated with it. This is the case of enhanced recovery after surgery (ERAS), which constitutes a paradigm shift for the optimization of perioperative care, which includes mobility and early gait, and which has been proven to reduce recovery time and post-operative complication rates 50. The role of ERAS in different surgical contexts was possible to assess in this review, verifying a reduction in the length of hospital stay between one and three days26,30,31. Other studies corroborate these data - in neurosurgery, the implementation of a protocol promoting early mobility in patients after spinal surgery resulted in a reduction of nine hours of hospitalization time and was a catalyst for the involvement of patients in their postoperative mobility9. For hepatectomies, in a survey involving 3,739 participants, length of stay was reduced by 2.22 days in the ERAS group and hospital costs were significantly lower compared to the standard care group (p < 0.0001) 51. In bariatric surgery, hospital stay, and costs were significantly lower with the ERAS approach, implying an average saving of 21.25% of the total cost of the procedure52.
In critical care, a plethora of life-sustaining measures associated with critical and unstable clinical conditions make early mobilization intimidating for professionals. Although safe, programs that promote physical activity, including walking, in mechanically ventilated patients are often avoided. Early mobilization in patients under intensive care measures is associated with a reduction in delirium, lower risk of rehospitalization, of infections and a reduction in the length of stay in the unit, with statistical significance53. Similar findings were found in this review, as they demonstrated a reduction in the length of stay in intensive care units24,37,38. In a unit for neurocritical, progressive mobility also resulted in a sustained improvement in the level of physical activity of patients and a reduction in the length of hospital stay54.
A systematic review identified studies that described the relationship between walking ability and health economic indicators. A better gait performance was associated with a shorter hospital stay, lower risk of hospitalization and significantly lower health costs42. In the community, in an elderly population, there was an association of 120 minutes of walking per week with a significant decrease in visits to the emergency department and hospitalization55. A study carried out over 4 years, involving 27,431 people without functional limitations and aged between 40 and 79, concluded that the time spent walking was significantly associated with lower health costs56. A survey focusing on diabetes concluded that in 10 years, the participants' health expenditure was 5.2% and 8.4% lower, for an increase of 3,000 and 5,000 daily steps, respectively47.
In the present review, it was also possible to find, in a hospital environment, the appreciation of walking as a health promotion strategy, guaranteeing the implementation of this activity through financial incentives21, professionals allocated only for this purpose16,17 and health plans of individualized interventions27. Although these programs do not change the length of hospital stay, one study concluded that increasing the walking speed to 0.10 m/s in hospitalized and seriously ill people was associated with better health status, less dependency and fewer days of hospitalization 57.
Although it is difficult to account for the gains associated with walking and establish direct and causal relationships with this intervention, the results found in this review indicate that maintaining the ability to walk can be economically beneficial and reduce the length of hospital stay. For the economic analysis, some limitations were found. The inclusion of multimodal programs in the study did not allow explicitly extracting the results in length of stay, related only to walking. Simultaneously, the use of quantitative evaluation measures, such as speed, distance covered and number of steps, which bring objectivity and consistency to the results, are not always present in the studies, making it difficult to aggregate results. It remains to be mentioned that in this review, the direct effects of the gait programs were translated into clinical and non-clinical indicators, such as the length of hospital stay. It is necessary to recognize that the long-term benefits of mobility programs tend to be overlooked in favor of apparent short-term cost savings. Economic evaluations associated with rehabilitation programs are complex to carry out, since the impact of interventions does not always translate into objectively measurable measures of health status41.
Conclusion
Hospitalization is associated with an increase in health expenses related to the incidence of adverse events, which compromise patient’s safety. At the same time, it is associated with an increase in the functional decline of the most vulnerable people. In turn, the ability to walk is an important health indicator, and is even considered the sixth functional vital sign. Thus, walking programs are assumed as a strategy to promote increased mobility during the hospitalization period. This review made it possible to assess the existence of a multiplicity of programs inserted in different hospitalization contexts, some of them dedicated exclusively to walking and others included in multimodal protocols that translate into immediate results in the improvement of functional decline. This variability of programs does not always allow demonstrating the specific benefit of walking, constituting a limitation of the study. Studies of an economic nature, which support the adoption of these programs are still scarce and economic evaluations in this field do not always reflect the gains obtained by implementing this type of intervention. However, this study suggests that intervention in patient´s gait is associated with the prevention of complications and the improvement of the functional condition, as well as a decrease in hospitalization time and, consequently, a reduction in health costs.
REFERENCES
1 Deloitte. Saúde em análise - Uma visão para o futuro. 2011. [ Links ]
2 Morais Nunes A, Matos A. Internamentos hospitalares no SNS - tendências recentes. Revista Ciências em Saúde. 2018;23:12-7. [ Links ]
3 OECD. Length of hospital stay (indicator) 2022 [Available from: https://data.oecd.org/healthcare/length-of-hospital-stay.htm. [ Links ]
4 Rodrigues C, Mendonça D, Martins MM. Functional trajectories of older acute medical inpatients. Enfermería Clínica (English Edition). 2020;30:260-8. [ Links ]
5 Wall BT, Dirks ML, van Loon LJ. Skeletal muscle atrophy during short-term disuse: implications for age-related sarcopenia. Ageing Res Rev. 2013;12(4):898-906. [ Links ]
6 Alley DE, Koster A, Mackey D, Cawthon P, Ferrucci L, Simonsick EM, et al. Hospitalization and change in body composition and strength in a population-based cohort of older persons. J Am Geriatr Soc. 2010;58(11):2085-91. [ Links ]
7 Callen BL, Mahoney JE, Grieves CB, Wells TJ, Enloe M. Frequency of hallway ambulation by hospitalized older adults on medical units of an academic hospital. Geriatr Nurs. 2004;25(4):212-7. [ Links ]
8 Pedersen MM, Bodilsen AC, Petersen J, Beyer N, Andersen O, Lawson-Smith L, et al. Twenty-four-hour mobility during acute hospitalization in older medical patients. J Gerontol A Biol Sci Med Sci. 2013;68(3):331-7. [ Links ]
9 Rupich K, Missimer E, OʼBrien D, Shafer G, Wilensky EM, Pierce JT, et al. The Benefits of Implementing an Early Mobility Protocol in Postoperative Neurosurgical Spine Patients. Am J Nurs. 2018;118(6):46-53. [ Links ]
10 Mazzei CJ, Yurek JW, Patel JN, Poletick EB, D'Achille RS, Wittig JC. Providing Patient Mobilization With a Mobility Technician Improves Staff Efficiency and Constrains Cost in Primary Total Hip Arthroplasty. JOURNAL OF ARTHROPLASTY.35(8):1973-8. [ Links ]
11 Colégio da Especialidade de Enfermagem de Reabilitação. Padrões de Qualidade dos Cuidados Especializados em Enfermagem de Reabilitação. Lisboa: Ordem dos Enfermeiros; 2018. [ Links ]
12 Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evidence Synthesis. 2020;18(10):2119-26. [ Links ]
13 Concelho Internacional de Enfermagem. ICNP browser - Browser CIPE 2019 [Available from: https://www.icn.ch/what-we-do/projects/ehealth-icnptm/icnp-browser. [ Links ]
14 BIREME / PAHO / WHO. DeCS/MeSH - Descritores em Ciências da Saúde São Paulo (SP)2017 [Available from: https://decs.bvsalud.org/. [ Links ]
15 Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467-73. [ Links ]
16 Balvardi S, Pecorelli N, Castelino T, Niculiseanu P, Alhashemi M, Liberman AS, et al. Impact of Facilitation of Early Mobilization on Postoperative Pulmonary Outcomes After Colorectal Surgery: A Randomized Controlled Trial. Ann Surg. 2021;273(5):868-75. [ Links ]
17 Hamilton AC, Lee N, Stilphen M, Hu B, Schramm S, Frost F, et al. Increasing Mobility via In-hospital Ambulation Protocol Delivered by Mobility Technicians: A Pilot Randomized Controlled Trial. J Hosp Med. 2019;14(5):272-7. [ Links ]
18 Carli F, Bousquet-Dion G, Awasthi R, Elsherbini N, Liberman S, Boutros M, et al. Effect of Multimodal Prehabilitation vs Postoperative Rehabilitation on 30-Day Postoperative Complications for Frail Patients Undergoing Resection of Colorectal Cancer: A Randomized Clinical Trial. JAMA Surg. 2020;155(3):233-42. [ Links ]
19 Johnson K, Razo S, Smith J, Cain A, Soper K. Optimize patient outcomes among females undergoing gynecological surgery: A randomized controlled trial. Appl Nurs Res. 2019;45:39-44. [ Links ]
20 Lura DJ, Venglar MC, van Duijn AJ, Csavina KR. Body weight supported treadmill vs. overground gait training for acute stroke gait rehabilitation. Int J Rehabil Res. 2019;42(3):270-4. [ Links ]
21 Strother M, Koepsell K, Song L, Faerber J, Bernard J, Malkowicz SB, et al. Financial incentives and wearable activity monitors to increase ambulation after cystectomy: A randomized controlled trial. Urol Oncol. 2021;39(7):434.e31-.e38. [ Links ]
22 Attabib N, Kurban D, Cheng CL, Rivers CS, Bailey CS, Christie S, et al. Factors associated with recovery in motor strength, walking ability, and bowel and bladder function after traumatic cauda equina injury. Journal of Neurotrauma. 2021;38(3):322-9. [ Links ]
23 Elsarrag M, Soldozy S, Patel P, Norat P, Sokolowski JD, Park MS, et al. Enhanced recovery after spine surgery: a systematic review. Neurosurgical Focus FOC. 2019;46(4):E3. [ Links ]
24 Klein KE, Bena JF, Mulkey M, Albert NM. Sustainability of a nurse-driven early progressive mobility protocol and patient clinical and psychological health outcomes in a neurological intensive care unit. Intensive and Critical Care Nursing. 2018;45:11-7. [ Links ]
25 Braun T, Grüneberg C, Süßmilch K, Wiessmeier M, Schwenk I, Eggert S, et al. An augmented prescribed exercise program (APEP) to improve mobility of older acute medical patients - a randomized, controlled pilot and feasibility trial. BMC Geriatr. 2019;19(1):240. [ Links ]
26 Ferrari F, Forte S, Sbalzer N, Zizioli V, Mauri M, Maggi C, et al. Validation of an enhanced recovery after surgery protocol in gynecologic surgery: an Italian randomized study. Am J Obstet Gynecol. 2020;223(4):543.e1-.e14. [ Links ]
27 Gazineo D, Godino L, Decaro R, Calogero P, Pinto D, Chiari P, et al. Assisted Walking Program on Walking Ability in In-Hospital Geriatric Patients: A Randomized Trial. J Am Geriatr Soc. 2021;69(3):637-43. [ Links ]
28 Martínez-Velilla N, Casas-Herrero A, Zambom-Ferraresi F, Sáez de Asteasu ML, Lucia A, Galbete A, et al. Effect of Exercise Intervention on Functional Decline in Very Elderly Patients During Acute Hospitalization: A Randomized Clinical Trial. JAMA Intern Med. 2019;179(1):28-36. [ Links ]
29 Vloothuis JDM, Mulder M, Nijland RHM, Goedhart QS, Konijnenbelt M, Mulder H, et al. Caregiver-mediated exercises with e-health support for early supported discharge after stroke (CARE4STROKE): A randomized controlled trial. PLoS One. 2019;14(4):e0214241. [ Links ]
30 Chen J, Peng LH, Min S. Implementation of perioperative breathing exercises and its effect on postoperative pulmonary complications and long-term prognosis in elderly patients undergoing laparoscopic colorectal surgery: A randomized controlled trial. Clin Rehabil. 2022;36(9):1229-43. [ Links ]
31 Cui Z, Li N, Gao C, Fan Y, Zhuang X, Liu J, et al. Precision implementation of early ambulation in elderly patients undergoing off-pump coronary artery bypass graft surgery: a randomized-controlled clinical trial. BMC Geriatr. 2020;20(1):404. [ Links ]
32 Pinskiy M, Lubovsky O, Kalichman L. The effect of a preoperative physical therapy education program on short-term outcomes of patients undergoing elective total hip arthroplasty: A controlled prospective clinical trial. Acta Orthop Traumatol Turc. 2021;55(4):306-10. [ Links ]
33 Su R, Feng W, Liu X, Song Y, Xu Z, Liu JG. Early Rehabilitation and Periprosthetic Bone Environment after Primary Total Hip Arthroplasty: A Randomized Controlled Trial. Orthop Surg. 2021;13(5):1521-31. [ Links ]
34 Nakao M, Izumi S, Yokoshima Y, Matsuba Y, Maeno Y. Prediction of life-space mobility in patients with stroke 2 months after discharge from rehabilitation: A retrospective cohort study. Disability and Rehabilitation: An International, Multidisciplinary Journal. 2020;42(14):2035-42. [ Links ]
35 Imamura M, Mirisola AR, Ribeiro FdQ, De Pretto LR, Alfieri FM, Delgado VR, et al. Rehabilitation of patients after COVID-19 recovery: An experience at the Physical and Rehabilitation Medicine Institute and Lucy Montoro Rehabilitation Institute. Clinics. 2021;76. [ Links ]
36 Marchisio AE, Ribeiro TA, Umpierres CSA, GalvÃo L, Rosito R, Macedo CAS, et al. Accelerated rehabilitation versus conventional rehabilitation in total hip arthroplasty (ARTHA): a randomized double blinded clinical trial. Rev Col Bras Cir. 2020;47:e20202548. [ Links ]
37 Oliveira RdÁ, Nakajima E, Vasconcelos VTd, Riera R, Baptista-Silva JCC. Effectiveness and safety of structured exercise vs. no exercise for asymptomatic aortic aneurysm: systematic review and meta-analysis. Jornal Vascular Brasileiro. 2020;19. [ Links ]
38 Windmöller P, Bodnar ET, Casagrande J, Dallazen F, Schneider J, Berwanger SA, et al. Physical Exercise Combined With CPAP in Subjects Who Underwent Surgical Myocardial Revascularization: A Randomized Clinical Trial. Respir Care. 2020;65(2):150-7. [ Links ]
39 Li I, Bui T, Phan HT, Llado A, King C, Scrivener K. App-based supplemental exercise in rehabilitation, adherence, and effect on outcomes: a randomized controlled trial. Clin Rehabil. 2020;34(8):1083-93. [ Links ]
40 Hill A-M, Ross-Adjie G, McPhail SM, Jacques A, Bulsara M, Cranfield A, et al. Incidence and associated risk factors for falls in older adults postdischarge who undergo elective total hip replacement surgery-A prospective cohort study. The Journals of Gerontology: Series A: Biological Sciences and Medical Sciences. 2021;76(10):1814-20. [ Links ]
41 O’Connor RJ. The economic benefits of rehabilitation for neurological conditions. In: Dietz V, Ward NS, Kennard C, Dietz V, Ward NS, editors. Oxford Textbook of Neurorehabilitation: Oxford University Press; 2020. p. 0. [ Links ]
42 Wohlrab M, Klenk J, Delgado-Ortiz L, Chambers M, Rochester L, Zuchowski M, et al. The value of walking: a systematic review on mobility and healthcare costs. European Review of Aging and Physical Activity. 2022;19(1):31. [ Links ]
43 Middleton A, Fritz SL, Lusardi M. Walking Speed: The Functional Vital Sign. Journal of Aging and Physical Activity. 2015;23(2):314-22. [ Links ]
44 Kim H, Choi W, Lee K, Song C. Virtual dual-task treadmill training using video recording for gait of chronic stroke survivors: a randomized controlled trial. Journal of Physical Therapy Science. 2015;27(12):3693-7. [ Links ]
45 Sourdet S, Lafont C, Rolland Y, Nourhashemi F, Andrieu S, Vellas B. Preventable Iatrogenic Disability in Elderly Patients During Hospitalization. J Am Med Dir Assoc. 2015;16(8):674-81. [ Links ]
46 Zisberg A, Shadmi E, Sinoff G, Gur-Yaish N, Srulovici E, Admi H. Low Mobility During Hospitalization and Functional Decline in Older Adults. Journal of the American Geriatrics Society. 2011;59(2):266-73. [ Links ]
47 Kato M, Goto A, Tanaka T, Sasaki S, Igata A, Noda M. Effects of walking on medical cost: A quantitative evaluation by simulation focusing on diabetes. J Diabetes Investig. 2013;4(6):667-72. [ Links ]
48 Laugesen SKN, Nissen SK, Kellett J, Brabrand M, Cooksley T, Nickel CH. Impaired Mobility, Rather Than Frailty, Should Be a Vital Sign. Chest. 2019;155(4):877-8. [ Links ]
49 Limão RP, Martins RML. Efetividade de programas de enfermagem de reabilitação no equilíbrio, marcha e independência funcional em idosos hospitalizados. Revista de Enfermagem Referência. 2021;5(8):1-10. [ Links ]
50 Pędziwiatr M, Mavrikis J, Witowski J, Adamos A, Major P, Nowakowski M, et al. Current status of enhanced recovery after surgery (ERAS) protocol in gastrointestinal surgery. Med Oncol. 2018;35(6):95. [ Links ]
51 Noba L, Rodgers S, Chandler C, Balfour A, Hariharan D, Yip VS. Enhanced Recovery After Surgery (ERAS) Reduces Hospital Costs and Improve Clinical Outcomes in Liver Surgery: a Systematic Review and Meta-Analysis. J Gastrointest Surg. 2020;24(4):918-32. [ Links ]
52 Higueras A, Gonzalez G, de Lourdes Bolaños M, Redondo MV, Olazabal IM, Ruiz-Tovar J. Economic Impact of the Implementation of an Enhanced Recovery after Surgery (ERAS) Protocol in a Bariatric Patient Undergoing a Roux-En-Y Gastric Bypass. Int J Environ Res Public Health. 2022;19(22). [ Links ]
53 Hunter A, Johnson L, Coustasse A. Reduction of Intensive Care Unit Length of Stay: The Case of Early Mobilization. Health Care Manag (Frederick). 2020;39(3):109-16. [ Links ]
54 Klein KE, Bena JF, Mulkey M, Albert NM. Sustainability of a nurse-driven early progressive mobility protocol and patient clinical and psychological health outcomes in a neurological intensive care unit. INTENSIVE AND CRITICAL CARE NURSING.45:11-7. [ Links ]
55 Perkins AJ, Clark DO. Assessing the association of walking with health services use and costs among socioeconomically disadvantaged older adults. Prev Med. 2001;32(6):492-501. [ Links ]
56 Tsuji I, Takahashi K, Nishino Y, Ohkubo T, Kuriyama S, Watanabe Y, et al. Impact of walking upon medical care expenditure in Japan: the Ohsaki Cohort Study. International Journal of Epidemiology. 2003;32(5):809-14. [ Links ]
57 Purser JL, Weinberger M, Cohen HJ, Pieper CF, Morey MC, Li T, et al. Walking speed predicts health status and hospital costs for frail elderly male veterans. J Rehabil Res Dev. 2005;42(4):535-46. [ Links ]
Declaration of informed consent:Written informed consent to publish this paper was obtained from the participants.
Received: March 02, 2023; Accepted: May 08, 2023; Published: May 30, 2023











 text in
text in