Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Portuguesa de Enfermagem de Reabilitação
versión impresa ISSN 2184-965Xversión On-line ISSN 2184-3023
RPER vol.6 no.1 Silvalde jun. 2023 Epub 30-Jun-2023
https://doi.org/10.33194/rper.2023.265
Original article reporting clinical or basic research
Rehabilitation Nursing Program for people with Impaired Swallowing in the context of Stroke: Exploratory Study
1Centro Hospitalar de Entre o Douro e Vouga
2Escola Superior de Saúde Norte da Cruz Vermelha Portuguesa, Oliveira de Azeméis, Portugal
Introduction: Stroke is the main cause of death in Portugal and one of the main causes of the presence of swallowing disorders. The evaluation and screening of impaired swallowing are recognized as indicators of the quality of health care. Rehabilitation nursing has great importance in the early detection of any commitment to swallowing, as well as in the definition of a rehabilitation program aimed at regaining skills and preventing complications. This study aims to analyze the effects of a program developed by rehabilitation nurses for people with impaired swallowing in the context of stroke.
Results:
218 individuals were evaluated. The population evaluated is predominantly male, the mean age was 73 years old, and the predominant vascular event was ischemic stroke. On admission, 50.5% of participants had swallowing disorders. Of these, 13.5% developed respiratory infection. Initially, 110 people were included in the study. 6 of these died, so the final data refer to 104 people. Statistically significant relationships were established between impaired swallowing and higher National Institute of Health Stroke Scale (NIHSS) scores.
Conclusion:
Most people showed improvement in swallowing ability after the rehabilitation nurse's intervention through a structured rehabilitation program. Impaired swallowing is related to higher scores on the NIHSS, and no relationship has been established with other variables such as stroke typology and location.
Descriptors: Rehabilitation nursing; Stroke; Deglutition disorders; Rehabilitation
Introdução:
O Acidente Vascular Cerebral (AVC) é a principal causa de morte em Portugal e um dos principais responsáveis pela presença de compromisso na deglutição. A avaliação e despiste da deglutição comprometida são reconhecidos como indicadores de qualidade dos cuidados de saúde. A Enfermagem de Reabilitação assume grande importância na deteção precoce do compromisso na deglutição bem como na definição de um programa de reabilitação que vise a reaquisição de capacidades e a prevenção de complicações. Este estudo pretende analisar os efeitos de um programa desenvolvido por enfermeiros de reabilitação na reeducação funcional da pessoa com deglutição comprometida em contexto de AVC.
Resultados:
Foram avaliados 218 indivíduos. A população avaliada é predominantemente do sexo masculino, a média de idade foi de 73 anos e o evento vascular predominante foi o AVC isquémico. À admissão 50,5% dos participantes apresentavam compromisso na deglutição. Destes, 13,5% desenvolveram infeção respiratória. Inicialmente foram incluídos no estudo 110 pessoas. 6 destas faleceram, pelo que os dados finais referem-se a 104 pessoas. Estabeleceram-se relações estatisticamente significativas entre o compromisso na deglutição e pontuações mais elevadas na NIHSS.
Conclusão:
A maioria das pessoas apresentou melhoria na capacidade de deglutição após a intervenção do enfermeiro de reabilitação através de um programa de reabilitação estruturado. O compromisso na deglutição relaciona-se com pontuações mais elevadas na National Institute of Health Stroke Scale (NIHSS), não se tendo estabelecido relação com outras variáveis como a tipologia e localização do AVC.
Descritores: Enfermagem em reabilitação; Acidente Vascular Cerebral; Transtornos da deglutição; Reabilitação
Introducción:
El accidente vascular cerebral es la principal causa de muerte en Portugal y una de las principales causas de presencia de. La evaluación y el tamizaje de la deglución alterada son reconocidos como indicadores de la calidad de la atención en salud. La enfermería en rehabilitatión es de gran importancia en la detección precoz de cualquier compromiso de deglución, así como en la definición de un programa de rehabilitación dirigido a recuperar habilidades y prevenir complicaciones. Este estudio tiene como objetivo analizar los efectos de un programa desarrollado por enfermeras de rehabilitación para personas con problemas de deglución en el contexto de un accidente cerebrovascular.
Resultados:
se evaluaron 218 individuos. La población evaluada es predominantemente masculina, la edad media fue de 73 años y el evento vascular predominante fue el ictus isquémico. Al ingreso, el 50,5% de los participantes presentaba compromiso de deglución. De estos, el 13,5% desarrolló infección respiratoria. Inicialmente, se incluyeron 110 personas en el estudio. De estos, 6 fallecieron, por lo que los datos finales se refieren a 104 personas. Se establecieron relaciones estadísticamente significativas entre la deglución alterada y puntuaciones National Institute of Health Stroke Scale (NIHSS) más altas.
Conclusión:
La mayoría de las personas mostró una mejora en la capacidad de deglución después de la intervención de la enfermera de rehabilitación a través de un programa de rehabilitación estructurado. La alteración de la deglución se relaciona con puntuaciones más altas en el NIHSS, y no se ha establecido relación con otras variables como tipología y localización del ictus.
Descriptores: Enfermería en rehabilitación; Accidente Vascular Cerebral; Trastornos de deglución; Rehabilitación
INTRODUCTION
Cerebral Vascular Accident (CVA) can be defined as the rapid development of clinical signs of focal (or global) disturbances in brain function, with symptoms lasting longer than 24 hours or leading to death, with no apparent cause other than the of vascular origin1.
Stroke is one of the main causes of morbidity and mortality worldwide, which results in dysfunctions, whether motor, cognitive-behavioral or emotional. These sequelae are associated with multiple medical complications that lead to prolonged periods of hospitalization and significant economic burden on health systems2.
Swallowing is, according to the International Classification for Nursing Practice (CIPE®) version 2015, the physiological process of “(...) the passage of liquids and fragmented foods, by the movement of the tongue and muscles, from the mouth to the stomach through the oropharynx and esophagus”3.
The complexity of swallowing comes from the involvement of the 6 pairs of cranial nerves in the coordination of more than 20 pairs of muscles4.
Initially described from a three-phase model: oral, pharyngeal and esophageal, the swallowing process was later divided into four phases (oral preparatory phase, oral phase, pharyngeal phase and esophageal phase) according to several studies developed in the meantime. , allowing the biomechanical description and movement of the food bolus during swallowing5.
The causes of impaired swallowing can be varied. However, when it is motivated by neurological disorders, it is called neurogenic dysphagia5.
Impaired swallowing, often referred to as dysphagia, is characterized by difficulty in swallowing saliva, liquids or solids. In the term “compromised swallowing”, among several dysfunctions in the swallowing process, oropharyngeal dysphagia is included6.
The problem of people with impaired swallowing has aroused interest in health regulators. In approaching this issue, experts have used the International Classification of Functioning, Disability and Health7.
Impaired swallowing is presented by the Order of Nurses through the focus “swallowing”, resorting to diagnoses and interventions aimed at its approach. It was based on these that the presented rehabilitation program was constructed3,8.
This commitment, in addition to impairing people's quality of life and nutritional status, could also lead to serious complications such as dehydration, malnutrition, pneumonia, asphyxia and even death. It is understandable, therefore, that this problem is associated with an increase in the number of hospitalization days of around 40% (%)9.
Focusing on the person with stroke, the prevalence of impaired swallowing in the acute phase is very frequent, and can go up to 78%. Pneumonia, in these cases, is one of the main causes of morbidity, and it is important to give special importance to the fact that a person with a stroke and impaired swallowing has a triple risk of developing pneumonia compared to people with a stroke without this disorder9.
In the acute phase of the stroke, impaired swallowing is clinically diagnosed in 40 to 70% of cases in the first three days and bronchial aspiration of saliva, food and/or liquids varies from 20 to 45% in the first five days10.
Although most people with stroke regain the ability to swallow spontaneously, it remains in some people after six months of evolution (11-50%)11. Thus, the assessment, diagnosis, investigation and treatment of impaired swallowing are focus of attention worthy of primacy by nurses11.
The aims of the clinical evaluation of swallowing are centered on the detection of swallowing impairment, characterization of its severity, determination of its causes, rehabilitation planning and measurement of treatment results12.
This dysfunction can be diagnosed through the clinical evaluation of swallowing or through the instrumental evaluation of swallowing, carried out through the objective analysis of the biodynamics of swallowing, through video-fluoroscopy or video-endoscopy13. The latter are more expensive and not always available.
The assessment of swallowing ability through the use of a valid and reliable instrument must occur before the administration of food, drinks or oral medication, within 4 to 24 hours of hospitalization. This assessment can be performed safely by nurses, with different levels of knowledge and experience13. However, no instrument for clinical assessment of swallowing ability is completely sensitive in determining this dysfunction, due to the heterogeneity of precursory causes of swallowing disorders4.
With a view to early detection of swallowing disorders, clinical evaluation and screening should be carried out primarily as a form of screening, considering the sensitivity of the tests and the possibility of finding false negatives and false positives14.
In short, swallowing assessments can be instrumental and/or clinical. Video-fluoroscopy is currently the exam of choice in the study of swallowing, as it allows an objective assessment of the biomechanics of this process. However, as it is inaccessible in some health units and is associated with high economic costs, it cannot be performed whenever a person is suspected of having impaired swallowing. Consequently, in order to identify such commitment and classify its severity, instruments were developed and validated for its evaluation and, in this specific case, with the specific objective of detecting it early in the acute phase of the stroke15.
In the process of rehabilitation of the person with impaired swallowing, the work carried out within an interdisciplinary team is imperative, in which all elements are aware of the problem involving the person, know how to identify the clinical signs and their consequences12.
Specialist Nurses in Rehabilitation Nursing must use specific rehabilitation techniques and intervene in the education of people and their significant family members/informal caregivers, with the aim of improving functions, regaining independence in life activities and minimizing the impact of disabilities installed16. The stroke person with impaired swallowing is no exception.
After evaluating the person and diagnosing the change in swallowing, the planning of Rehabilitation Nursing care follows, where the Specialist Nurse in Rehabilitation Nursing can play a fundamental role as an orchestrating and guiding member, aiming at the re-education of the “swallowing” function”. The specific care needed in the rehabilitation of people with impaired swallowing requires particular knowledge and skills in the area4.
This knowledge and skills include assessing the person's ability to feed and hydrate independently, considering their mobility, muscle strength, control of cutlery from the plate to the mouth, the ability to prepare food and liquids for intake, head control in a sitting position and visual acuity. The entire nursing assessment, contextualization of the problem, antecedents and previous habits help in determining the disability and underlie the nursing diagnoses17.
The core of nursing intervention lies in supporting people in meeting their human needs, in recovering self-care skills and in relearning skills that lead to their fulfillment18.
Dependence on self-care constitutes a basic focus in the planning of Rehabilitation Nursing care. When defining the interventions to be developed, the Specialist Nurse in Rehabilitation Nursing seeks strategies aimed at empowering the person for self-care.18 Particularizing the person with impaired swallowing, the Rehabilitation Nursing program must include interventions that promote the rehabilitation of the motor function, rehabilitation of respiratory function and rehabilitation of self-care eating and drinking in order to ensure adequate nutrition and hydration, favoring the person's autonomy in these activities of daily living.
Based on what was previously described, a rehabilitation program aimed at people with impaired swallowing was defined, including interventions aimed at recovering this function, promoting self-care and reducing complications related to this problem.
Thus, the aim is to analyze the effects of a program developed by rehabilitation nurses for people with impaired swallowing in the context of a stroke.
METHOD
A quantitative, exploratory, descriptive and retrospective study was carried out, based on existing data in the computer system to support the practice of Rehabilitation Nursing (Medtrix®), collected and recorded by the main researchers. The study design, objectives and methods were presented, and authorization was requested from the institutional ethics committee, which issued a positive opinion on its performance.
When approaching stroke victims with impaired swallowing, a rehabilitation program was designed (Table 1)8 to be carried out on weekdays, once a day, from admission to discharge, with adjustments being made at the level of diagnoses and interventions according to the evaluation carried out and with the collaboration of the person. A non-probabilistic convenience sample was used. Based on the results obtained, the plan was adapted in the different stages of the nursing process in order to respond to difficulties, correspond to health gains and facilitate functional readaptation to the condition of dependency.
The use of instruments to objectively measure the ability/disability to perform the various activities of daily living has become fundamental for outlining rehabilitation programs and evaluating their effects.
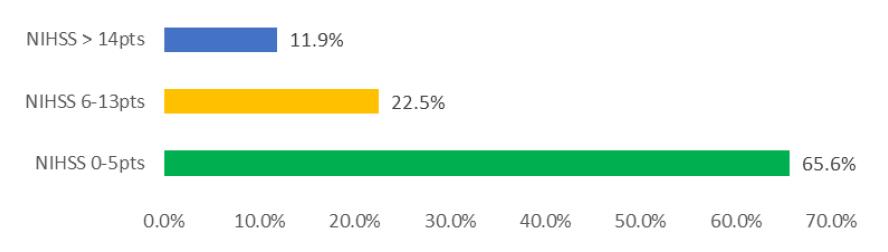
The National Institute of Health Stroke Scale (NIHSS) is a standard, systematically used, validated, simple, quick-to-apply (10 minutes), reliable, safe, quantitative scale used to measure the severity and magnitude of neurological dysfunction after stroke. which can be applied at the person's bedside by any health professional, allowing a common language for exchanging information between them. It was developed by American researchers (University of Cincinnati Stroke Center) as a research instrument, with the Portuguese version being validated(19). For data analysis, three subgroups were identified: NIHSS between 0-5 points (mild neurological impairment), NIHSS between 6 and 13 points (moderate neurological impairment) and NIHSS greater than 14 points (severe neurological impairment)20.
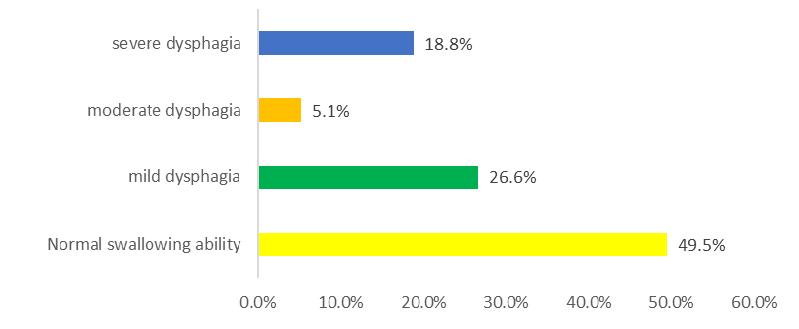
For the screening of impaired swallowing, the Gugging Swallowing Screen (GUSS) - Portuguese version(21) was used. The GUSS determines impairment severity and risk of aspiration in people with acute stroke. Compared to other tests, the GUSS test sequence is unique: the assessment begins with the swallowing of saliva followed by the swallowing of semi-solid, fluid and solid textures. The evaluation is based on a points system. In total, four severity levels can be determined:
0-9 points: severe dysphagia and high risk of aspiration;
10-14 points: moderate dysphagia and moderate risk of aspiration;
15-19 Points: mild dysphagia with mild aspiration;
20 points: normal swallowing ability.
For each severity level, different diet recommendations are provided21.
Table 1 Specific rehabilitation program for people with stroke and impaired swallowing8
| Rehabilitation Nursing Program - Person with Impaired Swallowing | |
|---|---|
| Reeducation of motor function - Orofacial exercises • Lips • Language • Mandible • Larynx • Cheeks - Sensory motor stimulation • Variation of flavors • Change of volume • Thermal and tactile stimulation • Massage |
10’ 10’ |
| Respiratory functional reeducation - Training of respiratory muscles - Techniques to improve ventilation, breathing pattern and ventilatory mechanics - Permeability of the airways - Strengthening the respiratory muscles - Teaching cough and directed cough |
10’ |
| Swallowing compensatory/facilitating strategies (to be applied during feeding and/or swallowing training) | Variable time |
| - Adaptation of food consistency ( Thickener use ( Adapted diet (soft, pasty, minced) | |
| - Postural adaptation ( Cervical flexion ( Cervical rotation to the affected side ( Lateral flexion to the healthy side | |
| - Swallowing facilitating maneuvers | |
| Bidaily oral hygiene | |
Statistical analysis was performed using the IBM SPSS Statistics version 22 program. Concerning the descriptive statistical analysis, frequencies, percentages, means and standard deviations were calculated. For the presentation of the data in graphical terms, the Microsoft Excel program was used.
Comparison of care results was performed using Student's t test for paired samples and to establish relationships between variables, Pearson's correlation coefficient was used. As the sample distribution is not normally distributed comparing the results of the two evaluation moments, it was decided to use the Wilcoxon test to analyze the averages and look for the validation or not of the null hypothesis.
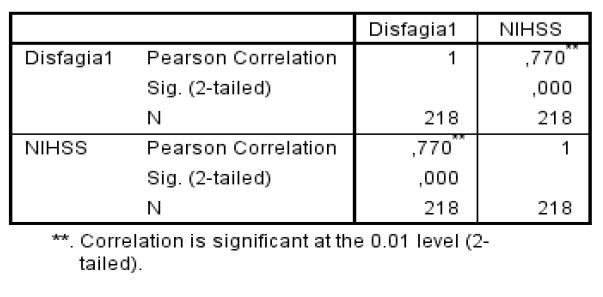
For the interpretation of the intensity of the correlations, the following values were adopted as a reference(22): r = 0.7 - strong correlation; r = 0.3 to 0.7 - moderate correlation; r = 0 to 0.3 - weak correlation. The significance level adopted throughout the study was 5%, thus rejecting the hypothesis that the correlation between the variables is zero at the 5% level when p ≤ 0.051922.
RESULTS
The results presented refer to the period from January 1 to June 30, 2021. During this period, 218 people with a diagnosis of stroke were admitted to the Stroke Unit. All were evaluated by the Specialist Nurse in Rehabilitation Nursing through protocols implemented in the service.
The most prevalent gender was male with 55% of individuals.
The predominant age group was from 71 to 80 years old, the mean was 73 years old, with a standard deviation of 13.9, and about 83% of the individuals were over 61 years old.
Analyzing the distribution of the vascular event, we have the predominance of ischemic stroke with 86.7% of cases.
Within the ischemic events, and according to the clinical classification of the Oxfordshire Community Project (OCSP) the most prevalent were partial anterior circulation infarcts (PACI) with 30%, later we have lacunar infarcts of the anterior circulation (LACI) with 28% of cases, followed by total anterior circulation infarcts (TACI) with 23% and finally with 19% posterior circulation infarcts (POCI).
With regard to bleeding events, the most prevalent were deep hematomas (LACH) with 83% of cases, followed by TACH with 10% and finally PACH with 7%.
With regard to NIHSS, through Graph 1, we can see that most people had NIHSS values between 0 and 5 points, corresponding to mild neurological impairment.
With regard to the assessment of swallowing in the first phase of problem detection and elaboration of Rehabilitation Nursing diagnoses, the results shown in graph 2 were obtained.
Through the analysis of the previous graph, 50.5% of the people admitted were detected by the Specialist Nurse in Rehabilitation Nursing some degree of impairment of the swallowing function.
It is important to add that 13.5% of these (with impaired swallowing) developed a respiratory infection.
Through the inferential analysis between the different variables under study, it was possible to establish a statistically significant relationship between the impairment in swallowing and the score obtained through the NIHSS assessment with a significance level of 0.000, with a strong correlation between the two variables (r =0.770). Thus, the higher the NIHSS score, the greater the swallowing impairment.
Initially, 110 people were included in the rehabilitation program (all those with changes in swallowing capacity). Of these, 6 died, so it was not possible to continue its implementation and, therefore, excluded from this analysis. Thus, the results that follow refer to the evaluation of 104 people. These received Rehabilitation Nursing care aimed at rehabilitation of the “swallowing” function in accordance with the program presented above.
The following graph shows the distribution of people with impaired swallowing, comparing the first moment of evaluation with the moment of discharge.
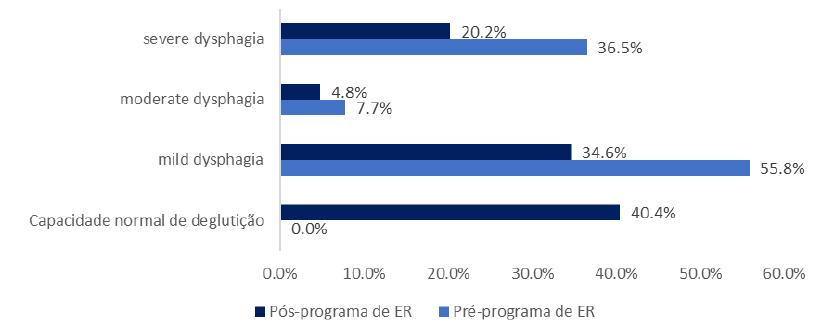
Graph 3 Comparative distribution of participants with impaired swallowing at the beginning of the implementation of the Rehabilitation Nursing program and at the end of it
Through the graph above, we can see that 40.4% of people with impaired swallowing recovered their normal swallowing ability with a reduction in the percentage of other levels of impaired swallowing.
In order to establish a statistically significant relationship between some variables, we resorted to Student's t test. We found that there is a highly significant difference when comparing the first assessment of the swallowing capacity with the moment of discharge, that is, after the intervention of the Specialist Nurse in Rehabilitation Nursing through a structured rehabilitation program. Thus, most of the individuals in the sample showed a positive evolution in their swallowing ability, with a transition in the degree of impairment in swallowing in the GUSS (p=0.000).
Thus, in view of the null hypothesis “There are no differences regarding the swallowing commitment before and after intervention by the Specialist Nurse in Rehabilitation Nursing”, this is rejected. That is, the positive effects of the rehabilitation program designed by the Specialist Nurse in Rehabilitation Nursing for the person with compromised swallowing with improvement or recovery of the swallowing capacity were proven.
DISCUSSION
In this study, which focused on analyzing the effects of a Rehabilitation Nursing program on people with post-stroke compromised swallowing, we obtained qualitative and quantitative information that allowed us to characterize individuals, their evolution in the first days/weeks after a stroke, as well as how to establish statistically significant and relevant correlations for the body of knowledge in Rehabilitation Nursing.
With regard to impaired swallowing in the acute phase of stroke, there is great variability in the incidence of this problem in different studies. All people admitted to the stroke unit were evaluated, with some degree of swallowing impairment being detected in 50.5% of them (similar to some studies), using the same assessment instrument23 or another instrument for clinical assessment of the capacity swallowing24. However, this incidence is slightly higher than that found in another study that used the same assessment instrument and also carried out in people with stroke25, but within the limits presented by other authors10. This evaluation was clinical, since in the acute phase it is the only available possibility, enabling faster responses regarding the functional capacity of swallowing.
Similar to other studies, different degrees of impairment in swallowing were found23,24,25,26.
Impaired swallowing after stroke is associated with greater morbidity, mortality and increased risk of pulmonary complications9,23. In the present study, six people who had been found to have impaired swallowing died and 13.5% developed a respiratory infection.
The presented Rehabilitation Nursing plan was applied to 104 people regardless of their degree of collaboration. Interventions were carried out either actively or passively with the person's collaboration. The results could be more evident if only people with cognitive capacity to collaborate in the rehabilitation program were included. However, as this exclusion criterion was not defined, the results presented include all patients included in the program.
The individuals included were predominantly male (55%), elderly people, with a mean age of 73 years old and the most frequent vascular event was ischemic stroke (86.7%) similar to other studies25,26.
As in other studies, there was no relationship between the type of event and its location23,25,26.
Through inferential analysis, we found that higher scores on the NIHSS are related to greater severity of impaired swallowing. This finding is corroborated by other analyzed studies26,27.
Regarding the evolution of the swallowing capacity throughout the study, we verified a positive evolution. After the implementation of the structured rehabilitation program, there was progress in the degree of swallowing impairment, with a transition in the level of swallowing impairment assessed using the GUSS, and in many people we verified the recovery of swallowing ability (40.4%). This evolution was statistically proven. Other studies also show this improvement after a Rehabilitation Nursing intervention8,28.
The present study provides guidance for the approach of the person with impaired swallowing by the Specialist Nurse in Rehabilitation Nursing.
The assessment of the swallowing capacity in the acute phase of the stroke assumes particular primacy on the part of the Specialist Nurse in Rehabilitation Nursing, since it is incumbent upon him to outline (safely) interventions related to eating/drinking self-care.
CONCLUSION
The focus that moved us to develop this study was the person with impaired swallowing in the acute phase of a cerebrovascular event.
A series of interventions were programmed as part of a rehabilitation program aimed at these people, including all those admitted to the Stroke Unit who benefited from it from admission to discharge, regardless of their degree of collaboration.
We verified that the implementation of the outlined rehabilitation program resulted in gains in the person's ability to swallow.
One of the major difficulties encountered is related to the different degrees of collaboration in the rehabilitation program on the part of the participants. It is up to the nurse to adjust interventions and optimize practices in order to enable evolution even in more complex situations.
Another of the limitations that is important to mention is related to the scarcity of studies carried out by Rehabilitation Nurses that focus on the intervention and rehabilitation of the person with impaired swallowing by this health professional and those that exist have a scarce target of intervention , with a limited sample. Several studies have been carried out with regard to the clinical evaluation of the swallowing capacity, a finding that is not verified with regard to its rehabilitation. In this area, it is also verified that many studies are carried out in the academic field.
Finally, the difficulty in including the informal caregiver during rehabilitation was a limitation, as a result of the current pandemic situation during the course of the study.
Rehabilitation Nursing is an area of specialized Nursing intervention, and the Rehabilitation Nurse seeks to mobilize knowledge with the aim of guiding the person and their caregivers in pursuit of the recovery of functionality, in the maintenance and promotion of well-being and quality of life. life and the recovery of functionality, through the promotion of self-care, the prevention of complications and the maximization of capacities.
With this study, it was possible to demonstrate the importance of Rehabilitation Nursing in the diagnosis of impaired swallowing and in its treatment. This proactive attitude in the early approach of the person with impaired swallowing after a stroke is fundamental for the survival and safety of the person, as it may minimize the risk of associated aspiration, improve functionality and quality of life.
The identification of indicators that are sensitive to Rehabilitation Nursing care, such as those addressed in this study, are crucially important due to the positive impact they have on people and on the health system.
More studies are needed to address this issue, exploring other variables that may justify the swallowing commitment in more detail, namely the specificity of the alterations found in terms of motricity and intraoral sensitivity and their influence on the swallowing ability and/or implementing other strategies that reinforce the people's recovery and minimize complications that may arise from the difficulties they demonstrate, regardless of the function that is compromised.
REFERENCES
1 Organização Mundial da Saúde. Manual STEPS de Acidentes Vascular Cerebrais da OMS: enfoque passo a passo para a vigilância de acidentes vascular cerebrais. Genebra:OMS; 2016. [Internet] [Acesso em 12 feb 2022]. Disponível em: https://www.paho.org/hq/dmdocuments/2009/manualpo.pdf [ Links ]
2 Kumar S, Selim MH, Caplan LR. Medical Complications after Stroke. Lancet Neurology; 2010. 9: 105-118. [Internet]. [Acesso em 12 feb 2022]. Disponível em: https://www.scirp.org/(S(czeh2tfqyw2orz553k1w0r45))/reference/ReferencesPapers.aspx?ReferenceID=1526860 [ Links ]
3 Ordem dos Enfermeiros. Classificação Internacional para a Prática de Enfermagem Versão 2015. Lisboa: Ordem dos Enfermeiros; 2016. [Internet]. [Acesso em 12 feb 2022]. Disponível em: https://futurosenf.files.wordpress.com/2017/04/cipe_2015.pdf [ Links ]
4 Braga R. Avaliação da Função Deglutição. In Marques-Vieira C, Sousa L. Cuidados de Enfermagem de Reabilitação à Pessoa ao Longo da Vida. 1ª ed. 181-188. Loures: Lusodidacta; 2016 [ Links ]
5 Matsuo K, Palmer J. Anatomy and Physiology of Feeding and Swallowing: Normal and Abnormal. Physical Medicine and Rehabilitation Clinics of North America. 2008. 19(4), 691-707. DOI: 10.1016/j.pmr.2008.06.00 [ Links ]
6 Andersen U, Beck A, Kjaersgaard A, Hansen T, Poulsen I. Systematic review and evidence based recommendations on texture modified foods and thickened fluids for adults (≥18 years) with oropharyngeal dysphagia. E-SPEN Journal; 2013. 8(4): 127-134. [Internet]. [Acesso em 15 feb 2022]. Disponível em: https://pubmed.ncbi.nlm.nih.gov/28939270/ [ Links ]
7 Ortega O, Martín A, Clavé P. Diagnosis and Management of Oropharyngeal Dysphagia Among Older Persons, State of the Art. Journal of the American Medical Directors Association; 2017. 18(7): 576-582. [Internet]. [Acesso em 11 feb 2022]. Disponível em: https://pubmed.ncbi.nlm.nih.gov/28412164/ [ Links ]
8 Silva P. Cuidados de enfermagem de reabilitação em doentes com deglutição comprometida: resultados de um programa de intervenção. Évora. 2018. Tese de Mestrado em Enfermagem de Reabilitação. [Internet]. [Acesso em 7 mar 2022] Disponível em: http://hdl.handle.net/10174/23326 [ Links ]
9 Altman K. Understanding Dysphagia: A Rapidly Emerging Problem. Otolaryngologic Clinics of North America; 2013. 46(6): 13-14. DOI: 10.1016/j.otc.2013.09.012 [ Links ]
10 Mourão LM, Almeida SMA, Lemos EO, Vicente LC, Teixeira AL. Frequência e fatores associado à disfagia após acidente vascular cerebral. CoDAS; 2015. 28(1): 66-70. [Internet]. [Acesso em 1 mar 2022] Disponível em: http://www.scielo.br/pdf/codas/v28n1/2317-1782-codas-28-01-00066.pdf [ Links ]
11 Cohen DL, Roffe C, Beavan J, Blackett B, Fairfield CA, Hamdy S, Havard D. Post-stroke dysphagia: A review and design considerations for future trials. Int J Stroke; 2016. 11(4): 399-411. [Internet]. [Acesso em 15 feb 2022]. Disponível em: https://journals.sagepub.com/doi/full/10.1177/1747493016639057 [ Links ]
12 Veríssimo D, Domingos A. Cuidados de enfermagem à pessoa com deglutição comprometida. Projeto de melhoria contínua da qualidade dos cuidados de enfermagem. 2014. [Internet]. [Acesso em 15 feb 2022]. Disponível em: http://www.ordemenfermeiros.pt/projectos/Documents/Projetos_Melhoria_Qualidade_Cuidados_Enfermagem/CHMedioTejo_ProjetoDegluticao.pdf [ Links ]
13 Passos KO, Cardoso FMCA, Scheeren B. Associação entre escalas de avaliação de funcionalidade e severidade da disfagia pós-acidente vascular cerebral. CoDAS; 2017. [Internet]. [Acesso em 15 feb 2022]. Disponível em: https://www.scielo.br/j/codas/a/YCDMjwpz3mHRJM3YqzpY4cP/?lang=pt [ Links ]
14 Umay E, Unlu E, Saylam G, Cakci A, Korkmaz H. Evaluation of Dysphagia in Early Stroke Patients by Bedside, Endoscopic and Electrophysiological Methods. Dysphagia; 2013. 28(3): 395-403 [ Links ]
15 Paixão CT, Silva LD, Camerini FG. Perfil da disfagia após um acidente vascular cerebral: uma revisão integrativa. Revista de Rede da Enfermagem do Noroeste; 2010. 11 (1). [Internet]. [Acesso em 1 mar 2022]. Disponível em: http://www.revistarene.ufc.br/revista/index.php/revista/article/view/362. [ Links ]
16 Regulamento nº 125/2011 de 18 de fevereiro da Ordem dos Enfermeiros. Diário da República. 2ªSérie, 35. (2011). [Internet]. [Acesso em 1 mar 2022]. Disponível em: http://www.aper.pt/Ficheiros/ ompetências%20do%20enfermeiro%20de%20reabilita%C3%A7%C3%A3o.pdf [ Links ]
17 Glenn-Molali N. Alimentação e Deglutição. In C. Hoeman S. P., Enfermagem de Reabilitação: Prevenção, Intervenção e Resultados Esperados. 4ª ed. 295-317. Loures: Lusodidacta; 2011 [ Links ]
18 Petronilho F, Machado M. Teorias de Enfermagem e Autocuidado: Contributos para a Construção do Cuidado de Reabilitação. In Marques-Vieira C, Sousa L, Cuidados de Enfermagem de Reabilitação à Pessoa ao Longo da Vida (1ª ed., pp. 3-14). Loures: Lusodidacta; 2011 [ Links ]
19 Castro P, Mendonça T, Abreu P, Carvalho M, Azevedo E. National Institute of Health Stroke Scale (NIHSS) International initiative - Versão Portuguesa. Sinapse; 2008. 8(1): 67-68. [ Links ]
20 Campos TF, Dantas AA, Melo LP, Oliveira DC: Grau neurológico e funcionalidade de pacientes crónicos com acidente vascular cerebral: implicações para a prática clínica. Arq. Ciên. Saúde. 2014. 21(1). 28-33. [ Links ]
21 Oliveira I de J, Couto GR, Moreira A, Gonçalves C, Marques M, Ferreira PL. A versão portuguesa do gugging swallowing screen: resultados da sua aplicação. Millenium -Journal of Education, Technologies, and Health. 2(16):93-101. [Internet]. [Acesso em 17 mar 2022]. Disponível em: https://revistas.rcaap.pt/millenium/article/view/24585 [ Links ]
22 Upton G, Cook I. A dictionary of statistics. 2nd ed. Oxford: Oxford University Press; 2008. [ Links ]
23 Almeida E. Frequência e fatores relacionados à disfagia orofaríngea após acidente vascular encefálico [Dissertação]. Belo Horizonte: Universidade Federal de Minas Gerais; 2009. [ Links ]
24 Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnostic and pulmonary complications. Stroke; 2005. 36(12):2756-63. [ Links ]
25 Oliveira I - A pessoa com deglutição comprometida após o AVC: da evidência à prática. Dissertação de Doutoramento em Ciências de Enfermagem. Porto. 2022. [Internet]. [Acesso em 10 ago 2022]. Disponível em: https://rper.aper.pt/index.php/rper/issue/view/14/21 [ Links ]
26 Sá N, Oliveira A, Silva A, Brandão S. Consulta de Enfermagem de Reabilitação ao doente pós evento cerebrovascular: Que desvios encontrados ao plano delineado à alta pelo enfermeiro de reabilitação?. Rev Port Enf Reab; 2020. 3(1):5-13. [Internet]. [Acesso em 1 mar 2022]. Disponível em: https://rper.aper.pt/index.php/rper/article/view/108 [ Links ]
27 Itaquy R, Favero S, Ribeiro M, Barea L, Almeida S, Mancopes R. Disfagia e acidente vascular cerebral: relação entre o grau de severidade e o nível de comportamento neurológico. Sociedade Brasileira de Fonoaudiologia; 2011. 23(4): 385-389. [Internet]. [Acesso em 3 mar 2022]. Disponível em: http://www.scielo.br/scielo.php?pid=S2179-64912011000400016&script=sci_arttext. [ Links ]
28 Pinto PS. Avaliação da disfagia numa unidade de AVC. Nursing. 2015. [Internet]. [Acesso em 3 mar 2022]. Disponível em http://www.nursing.pt/avaliacao-da-disfagia-numa-unidade-de-avc/ [ Links ]
Declaration of informed consent:Totally retrospective study based on the analysis of existing data from the computer system to support the practice of Rehabilitation Nursing, collected and recorded by the main researchers.
Received: June 12, 2022; Accepted: December 15, 2022; Published: January 30, 2023











 texto en
texto en