Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Portuguesa de Enfermagem de Reabilitação
Print version ISSN 2184-965XOn-line version ISSN 2184-3023
RPER vol.6 no.1 Silvalde June 2023 Epub June 30, 2023
https://doi.org/10.33194/rper.2023.213
Original article reporting basic or clinical research
Outcomes from the rehabilitation and education program for people with heart failure (REPIC Program)
1Centro Hospitalar de Vila Nova de Gaia/Espinho, EPE, Vila Nova de gaia, Portugal
2Instituto de Ciências Biomédicas Abel Salazar, Porto, Portugal
Introduction:
Despite advances in treatment, heart failure is a chronic disease whose incidence increases with age. Hospitalizations for decompensation remain high, so it is crucial to prioritize strategies for self-management, such as teaching, monitoring and cardiac rehabilitation programs. To this end, this study aimed to verify the impact of the REPIC program on quality of life, level of knowledge and adherence to physical exercise.
Methodology:
Quantitative study with a before-after design of a single group carried out in a sample of 110 people with heart failure, who were submitted to a rehabilitation and health education program during hospitalization and telephonic follow-up, one month, six months and one year after clinical discharge.
Results and Discussion:
Most participants are male (66%), and the age range varies between 30 and 89, with an average of 64.3 years and a standard deviation of 14.4. Data analysis showed a statistically significant improvement in knowledge about the disease, as well as in the perception of quality of life in the dimensions mobility, personal care, usual activities and general level of health (p=0.01). The increase in physical exercise time after the REPIC program was confirmed with a statistically significant result [t (109)=6.03; p=0.019]. The obtained results demonstrate the benefits of health education and telephone nursing follow-up, namely the improvement in the level of knowledge about the disease, in the quality of life and in the adherence to physical exercise.
Conclusion:
The REPIC program made it possible to reinforce the educational process, enhance self-management behaviors, improve quality of life and increase the duration of physical exercise.
DESCRIPTORS: heart failure; self-management; self-care; rehabilitation nurse
Introdução:
Apesar dos avanços no tratamento, a insuficiência cardíaca é uma doença crónica, cuja incidência aumenta com a idade. Os internamentos por descompensação mantêm-se elevados, pelo que é crucial priorizar estratégias para a autogestão, tais como o ensino, o acompanhamento e os programas de reabilitação cardíaca. Face ao exposto, este estudo teve como objetivo verificar o impacto do programa REPIC na qualidade de vida, nível de conhecimentos e adesão ao exercício físico.
Metodologia:
Estudo quantitativo com desenho antes-após de grupo único realizado numa amostra de 110 pessoas com insuficiência cardíaca, sujeitos a um programa de reabilitação e educação para a saúde durante o internamento e com follow-up telefónico, ao final de um mês, seis meses e um ano após a alta clínica.
Resultados e Discussão:
A maioria dos participantes são do sexo masculino (66%) e a amplitude da idade varia entre 30 e 89, com uma média de 64,3 anos e um desvio padrão de 14,4. A análise dos dados evidenciou uma melhoria estatisticamente significativa no conhecimento sobre a doença, bem como na perceção da qualidade de vida nas dimensões mobilidade, cuidados pessoais, atividades habituais e nível geral de saúde (p=0,01). O incremento no tempo de exercício físico após o programa REPIC foi confirmado com resultado estatisticamente significativo [t (109)=6,03; p=0,019]. Os resultados obtidos demonstram os benefícios da educação para a saúde e do acompanhamento telefónico de enfermagem, nomeadamente a melhoria no nível de conhecimentos sobre a doença, na qualidade de vida e na adesão ao exercício físico.
Conclusão:
O programa REPIC permitiu reforçar o processo educativo, potenciar os comportamentos de autogestão, melhorar a qualidade de vida e aumentar a duração do exercício físico.
DESCRITORES: insuficiência cardíaca; autogestão; autocuidado; enfermagem de reabilitação
Introducción:
A pesar de los avances en el tratamiento, la insuficiencia cardíaca es una enfermedad crónica cuya incidencia aumenta con la edad. Las hospitalizaciones por descompensación siguen siendo elevadas, por lo que es fundamental priorizar estrategias de autocuidado, como programas de enseñanza, seguimiento y rehabilitación cardiaca. En vista de lo anterior, este estudio tuvo como objetivo verificar el impacto del programa REPIC en la calidad de vida, el nivel de conocimiento y la adherencia al ejercicio físico.
Metodología:
Estudio cuantitativo con diseño antes-después de un solo grupo realizado en una muestra de 110 personas con insuficiencia cardiaca, sometidas a un programa de rehabilitación y educación para la salud durante la hospitalización y con seguimiento telefónico, al cabo de un mes, seis meses y un año después del alta clínica.
Resultados y Discusión:
La mayoría de los participantes son hombres (66%) y el rango de edad varía entre 30 y 89 años, con una media de 64,3 años y una desviación estándar de 14,4. El análisis de los datos mostró una mejoría estadísticamente significativa en el conocimiento sobre la enfermedad, así como en la percepción de la calidad de vida en las dimensiones movilidad, cuidado personal, actividades habituales y estado general de salud (p=0,01). El aumento del tiempo de ejercicio físico tras el programa REPIC se confirmó con un resultado estadísticamente significativo [t (109)=6,03; p=0,019]. Los resultados obtenidos demuestran los beneficios de la educación sanitaria y el seguimiento telefónico de enfermería, concretamente la mejora en el nivel de conocimiento sobre la enfermedad, en la calidad de vida y en la adherencia al ejercicio físico.
Conclusión:
El programa REPIC permitió reforzar el proceso educativo, potenciar las conductas de autogestión, mejorar la calidad de vida y aumentar la duración del ejercicio físico.
DESCRIPTORES: insuficiencia cardíaca; autogestión; autocuidado; enfermería de rehabilitación
INTRODUCTION
Heart failure (HF) is a chronic disease and a growing public health problem. According to the Portuguese Society of Cardiology, the prevalence of HF in Portugal is estimated around 400,000 individuals. Its incidence increases with age, constituting the first cause of hospitalization after 65 years in industrialized countries. Despite advances in medicine, clients with HF maintain high rates of mortality and rehospitalization, which are associated with high financial costs for the National Health Service1. These data shows a lack of organization of resources in the assistance of people with HF in Portugal at the various levels of care and follow-up, making it urgent to prioritize this disease in health policies.
Nurses play an active role in preventing cardiovascular disease, as evidence demonstrates that multidisciplinary programs coordinated by nurses are more effective than usual care in reducing cardiovascular risk 2. Nurses, in addition to constituting the largest professional group in healthcare, have teaching and communication skills that enhance clients' adherence behaviors 3)(4.
Likewise, the Portuguese Society of Cardiology recognizes, in its recommendations, the role of the specialist nurse in rehabilitation nursing (RN) as a fundamental element of the cardiac rehabilitation (CR) teams, based on the core of specific competences of the same specialty 5. CR programs are intended to respond to the improvement of the health potential of people with heart problems, and are constituted by multidisciplinary teams with complementary support functions that include assessment of cardiovascular risk; health education; early mobilization and physical exercise training 6)(7. Although in the literature it is divided into three phases - inpatient, outpatient and long-term intervention (designated, respectively, as phases 1, 2 and 3), CR must constitute a continuous process throughout the life cycle 4)( 8).
Considering the evidence described in the literature and national and international recommendations, it is crucial to create strategies that allow self-care and self-management of HF, including CR 4)(7)(9)(10)(11) (12)(13.
Rehabilitation and Education Program for Persons with Heart Failure (REPIC Program)
The Rehabilitation and Education Program for Persons with HF (REPIC) is developed through RN intervention, starting with hospitalization and follow-up after discharge. Prior to the implementation of the REPIC program, an initial assessment is carried out, which should include comorbidities, cardiovascular risk factors, physical examination (muscle strength, weight, abdominal perimeter and edema), activity and physical exercise habits and the assessment of knowledge about the disease. The objectives of the REPIC program include:
- Preventing immobility sequelae and/or improve functional capacity;
- Ensuring health education;
- Promoting adherence to physical exercise and self-management of the disease;
- Encouraging shared responsibility and continuity in long-term rehabilitation.
The REPIC program includes the educational process on self-management behaviors of the disease and physical exercise training, as soon as clinical, electrical and hemodynamic stability is ensured (Pestana and Vermelho, 2021). Training sessions begin with a warm-up period (around five minutes), followed by the exercise training period, which can range from 5 to 20 minutes (according to individual tolerance), ending with stretching and gradual reduction of exercise intensity 7. The type of exercise is low intensity, with energy expenditure of up to 4 metabolic equivalents (METS), including bridge, gait, pedal and stairs exercises 2. During the performance of exercise training, expiration is recommended in the concentric phase of the exercises and inspiration in the eccentric phase of the exercises, as a strategy for energy conservation and reduction of respiratory and cardiac effort 14. In order to determine the effort tolerance and prevent complications, the assessment of the subjective perception of effort (Borg) is warranted as well as heart rate; pain; blood pressure; peripheral oxygen saturation and heart rate monitoring 4)(7.
Education about self-management of the disease and the therapeutic regime are fundamental components of the REPIC program, with prior assessment of knowledge about the disease. The information provided considers co-morbidities with the potential to influence information retention (such as dementia, cognitive impairment and/or depression) and includes individualized educational sessions accompanied by informational flyers9. The RN educational intervention for people with HF focuses on general information about the disease; pharmacological treatment; psychosocial aspects; alarm signs and symptoms; control of cardiovascular risk factors; dietary regimen (including salt and fluid intake); vaccination; activity and physical exercise and exual activity9)(15.
METHODOLOGY
Original study based on the quantitative paradigm and, considering the follow-up, of the prospective longitudinal type. Based on manipulation, this is a quasi-experimental study with a single-group before-after design. The option for a quasi-experimental study is related to the existence of sufficient evidence of the benefits of the interventions under study (namely CR programs and nursing follow-up in the person with HF), so establishing a control group would constitute a ethical dilemma.
The guide for quasi-experimental studies (Transparent Reporting of Evaluations with Nonrandomized Designs: TREND) was used as a reference in the planning and execution of this research 16.
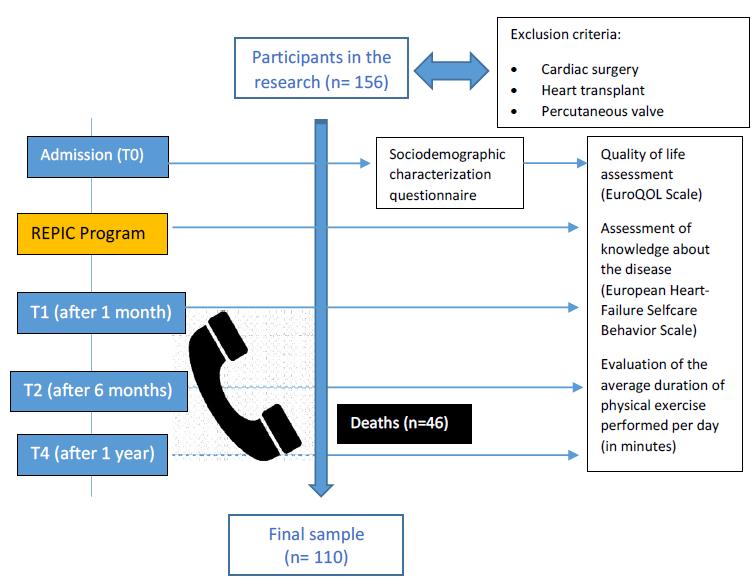
A non-probabilistic convenience sample consisting of 110 participants included in the REPIC program was established. Inclusion criteria were established: patients admitted to the service with HF diagnosis and acceptance to participate in the study. The following exclusion criteria were established: clients undergoing cardiac surgery, heart transplantation or percutaneous valve implantation, as it is intended at this stage to include clients with HF as a clinical diagnosis.
The REPIC program was initiated during hospitalization and included education, physical exercise training and follow-up after discharge. The follow-up was carried out by telephone contact at the end of 1 month, 6 months and 1 year after discharge, with data collection carried out using forms designed for this purpose (see figure 1).
The independent variable is the REPIC program (RN intervention that includes health education, exercise training during hospitalization and follow-up after discharge). Sociodemographic characterization variables include age, sex and cardiovascular risk factors. The variables considered as dependent were operationally defined as follows:
The level of knowledge about the disease: operationally defined by the mean of the set of answers obtained by applying the European Heart Failure Self-care Behavior Scale 17 validated for Portugal 18. It allows assessing the two key behaviors for self-care in heart failure: recognition of signs and symptoms of decompensation and decision-making in the event of such symptoms. It´s a Likert-type scale from 1 to 5, and the highest value reached by the average of the answers will be the one that presents a better self-management behavior regarding the parameters evaluated by the instrument. This scale is composed of 9 questions, with a minimum score of 9 and a maximum of 45, with a cut-off point established at 32;
Quality of life: operationally defined by the average of the set of responses obtained by applying the EuroQOL 5D/3L Scale. This scale includes two distinct evaluation sections. The first part of the instrument includes the assessment of the state of health in 5 dimensions using a Likert-type scale from 1 to 3. Although the scale instruction indicates the reading by using the numerical algorithm of all responses, at the option of the authors, analysis will be made of each dimension of the scale. Thus, the reading was done by analyzing the average value of the responses obtained, and a higher value is associated with better behavior regarding the evaluated parameters. The second part of the Euro QOL includes the visual analogue health scale, graded from 0 to 100 (where a higher value corresponds to a better individual perception of the state of health at the time of the assessment);
Regular physical exercise: operationally defined by the average daily time (in minutes) in performing aerobic physical exercise reported by the participants, including the following types of activity: walking, running, pedaling, cycling and swimming (modalities mentioned by the participants).
The hypotheses established with this research include:
a) There is a positive impact on the level of knowledge of the person with CI with the REPIC program;
b) The REPIC program improves the perception of quality of life in people with HF;
c) There is an increase in the average time spent in the practice of physical exercise by the person with HF before the REPIC program and at the end of 1 year.
To carry out this research, all ethical procedures were ensured, namely obtaining informed consent from the participants, and approval by the institutional ethics committee (Ref. 526/2012).
Inferential and descriptive statistics were used for data analysis to characterize the variables under study. Student's t test for paired samples was used to compare means and assess differences, before and 1 year after the REPIC program. The data obtained were stored and analyzed using the SPSS software (version 27) and the significance level adopted was 5% (p value < 0.05).
RESULTS
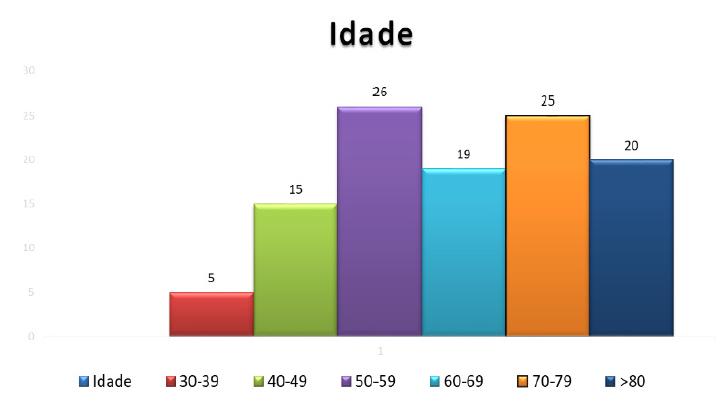
The sociodemographic characterization of the sample reveals that most participants are male (66%) and 34% are female. With regard to age, the range varies between a minimum age of 30 and a maximum of 89, with an average of 64.3 years-old and a standard deviation of 14.4 (figure 2).
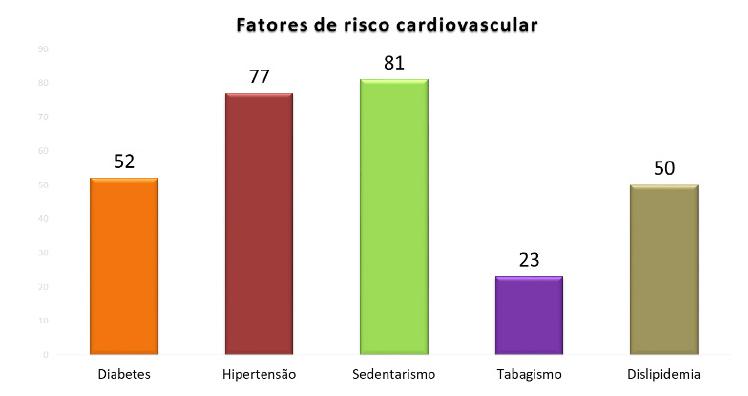
With regard to cardiovascular risk factors, there is a predominance of arterial hypertension and sedentary lifestyle, corresponding to approximately 74% of the sample, followed by diabetes and dyslipidemia (present in about 50% of the participants) and finally smoking , present in 21% of the participants (figure 3).
The evaluation of the impact of the REPIC program regarding the level of knowledge about HF was operationally defined by the responses resulting from the application of the European Heart Failure Self-care Behavior Scale 17. For this purpose, the means of responses obtained between the assessment carried out before the REPIC program and the assessment carried out 1 year later were compared, using Student's t test for paired samples (Table 1).
Table 1 Descriptive data on the level of knowledge about heart failure. (European Heart Failure Self-care Behaviour Scale)
| Parameters assessed | n | Initial assessment | Evaluation at the end of 1 year | P | ||
|---|---|---|---|---|---|---|
| M | Dp | M | Dp | |||
| I weigh myself every day or every 2/2 days | 110 | 1.87 | 1.34 | 4.07 | 1.1 | 0.01 |
| If shortness of breath increases, I contact the doctor/nurse | 110 | 2.06 | 1.4 | 3.44 | 1.13 | 0.01 |
| If the feet/legs swell more, I contact the doctor/nurse | 110 | 1.59 | 1.16 | 3.9 | 0.97 | 0.01 |
| If my weight increases by 2 kg in a week, I contact the doctor/nurse | 110 | 1.26 | 0.76 | 3.71 | 1.14 | 0.01 |
| I limit the amount of fluids I drink each day | 110 | 1.45 | 0.76 | 3.46 | 1.07 | 0.01 |
| If I notice that my tiredness is increasing, I contact the doctor/nurse | 110 | 1.8 | 1.15 | 3.73 | 1.15 | 0.01 |
| My diet is low in salt | 110 | 3.83 | 1.37 | 4.8 | 0.65 | 0.01 |
| I comply with the prescribed medication | 110 | 4.67 | 0.92 | 5 | 0 | 0.01 |
| I practice physical exercise | 110 | 2.32 | 1.41 | 3.91 | 1.29 | 0.01 |
M - Mean; S - standard deviation; P - p value by paired samples t test
Regarding the assessment of the impact of the program on the perception of quality of life, this was operationally defined by the responses obtained by applying the EuroQOL Scale. Likewise, the averages of the answers obtained between the evaluation prior to the implementation of the REPIC program and the evaluation carried out 1 year later were compared (Table 2). As for the perception of health status, this was operationally defined by the visual analogue scale included in the EuroQOL Scale, with 0 being the “worst health status” and 100 the “best health status.
Table 2 Descriptive data on the perception of quality of life (EuroQOL 5D/3L)
| Parameters assessed | n | Initial assessment | Evaluation at the end of 1 year | P | ||
|---|---|---|---|---|---|---|
| M | S | M | S | |||
| Mobility | 110 | 2.26 | 0.54 | 2.65 | 0.48 | 0.01 |
| Personal cares | 110 | 2.39 | 0.65 | 2.69 | 0.52 | 0.01 |
| Usual activities | 110 | 2.34 | 0.63 | 2.63 | 0.57 | 0.01 |
| Pain/discomfort | 110 | 2.53 | 0.63 | 2.61 | 0.49 | 0.21 |
| Anxiety/depression | 110 | 2.05 | 0.66 | 2.26 | 0.69 | 0.01 |
| Comparison of health status during the last 12 months | 110 | 1.6 | 0.83 | 2.51 | 0.65 | 0.01 |
M - Mean; S - standard deviation; P - p value by paired samples t test
Finally, table 3 represents the results obtained relative to the average duration of daily physical exercise (in minutes). It was verified that there are statistically significant differences between the previous moment of implementation of the REPIC program (M=17.04; SD=22.67) and at the end of one year (M=33.32; SD=20.99), these results being also confirmed by the t test for paired samples t (109)=6.03; p=0.01.
Table 3 Descriptive data of the average daily duration of physical exercise (in minutes)
| Parameters assessed | n | Initial assessment | Evaluation at the end of 1 year | P | ||
|---|---|---|---|---|---|---|
| M | S | M | S | |||
| Time/duration of daily physical exercise (minutes) | 110 | 17.04 | 22.67 | 33.32 | 20.99 | 0.01 |
M - Mean; S - standard deviation; P - p value by paired samples t test
DISCUSSION
The analysis of the results allows us to conclude that there was an improvement in the level of knowledge about the disease in the study participants in all dimensions of the scale after the REPIC program, with a statistically significant result (p=0.01).
The results of this study demonstrated that there is a positive impact on the level of knowledge about the disease, an improvement in the perception of quality of life and that there are differences in the average time spent performing physical exercise with the REPIC program. The improvement in the perception of quality of life in people with HF after the REPIC program, were revealed with statistical significance in the dimensions of mobility (p=0.01); personal care (p=0.01); usual activities (p=0.01) and general level of health (p=0.01). Finally, the analysis of the results led to the conclusion that there are differences in the perception of the health status evaluated before the implementation of the REPIC program (M=50.9; SD=17.36) and 1 after the same intervention program (M=69, 5;SD=18.8), these data being also confirmed by Student's t test for paired samples t(109)=7.67; p=0.01.
The state of the art corroborates the results of this research, as nurses, through the health education practices, enhances the understanding of the disease, increases self-management behaviors and reinforces the surveillance of the signs and symptoms of HF decompensation. In fact, recommendations of the European Society of Cardiology also associates nurse education on self-management of HF with a lower risk of hospital readmissions and mortality reduction9. In line with the results of our research, the results of a study revealed that nursing education on self-management significantly improved disease self-management behaviors in people with HF. This difference was statistically significant (β = 4.15, p < 0.05) and increased with each education session 19. Hospitalization constitutes a period of excellence for the beginning of the education program on self-management behaviors, since the person and the caregiver are more receptive and available to assimilate the contents and daily contact with RN specialists is facilitated. The REPIC program includes a systematic and standardized education program during hospitalization and educational reinforcements provided at clinical discharge, supported by flyers. Such strategies seem to improve understanding about the disease, its treatment and, consequently, adherence to the therapeutic regimen, with an improvement in quality of life. Another investigation concluded that a nursing intervention and follow-up program implemented in people with HF improved self-management behaviors and quality of life, being also associated with a lower number of hospitalizations 21. However, in contrast to the results of our study, a meta-analysis indicated that nursing education on self-management of the disease is not associated with improvements in quality of life or knowledge about HF 22. Such contradictory results may be due to the fact that quality of life is not a reliable result measure in short-term interventions. On the other hand, the impact of nursing education on disease self-management is intrinsically dependent on the duration and frequency of the educational process, which are enhanced by periodic follow-ups over time.
Regarding Nursing follow-up after discharge, the results of one study are in line with the results of our research. This randomized study found greater adherence to pharmacological and non-pharmacological behaviors in the Intervention Group that was subject to Nursing education and telephone monitoring (p<0.001). The lowest rate of readmissions and mortality in the Intervention Group after 90 days was another of the results obtained 23. Such conclusions reinforce the importance of telephone follow-up as an alternative strategy associated with multiple benefits (greater adherence to therapy, reduction in readmissions and mortality). In addition, it ensures the monitoring of some people with HF, considering certain factors such as availability to travel to hospital units, clinical status/comorbidities and geographical distance.
In regard to physical exercise training in people with HF, there is consistent literature evidence that corroborates the results and demonstrates that CR programs and physical exercise training improves functional capacity and quality of life. Clinical trials and meta-analyses performed in people with HF with reduced ejection fraction demonstrates that CR reduces hospital readmissions for HF, although uncertainty persists about its effects on mortality 9. The practice of regular physical exercise in people with HF is associated with improved functional capacity and constitutes a recommendation Level of Evidence IA15. A meta-analysis refers beneficial effects of exercise-based CR on HF, improvement in functional capacity and quality of life, as well as decreased hospitalization and mortality 24. Likewise, the institution of protocols with physical exercise that include walking and upper limb muscle strength training improves the performance of daily life activities, gait and functional capacity in people with HF 11. Regarding the REPIC program, exercise training was performed during hospitalization, which allowed the assessment of individual functional capacity, facilitated the initiation of physical exercise in a controlled environment and the management of symptoms and potential complications before hospital discharge. Thus, the conclusions of our research are in line with the results of the INCARD study, by confirming the benefits of in-hospital rehabilitation, namely in the improvement in the left ventricular ejection fraction and increase in the maximum volume of oxygen, which corroborates the idea that training with physical exercise has a positive impact on these people and should be performed regardless of the HF etiology 13. Likewise, the results of the randomized ERIC-HF study also prove that there are statistically significant differences between the group that underwent an exercise training intervention during hospitalization and the control group. The ERIC-HF protocol, like the REPIC program, demonstrated safety and efficacy during its implementation, with no adverse effects occurring. In addition, the ERIC-HF study reveals an increase in functional capacity (assessed by the 6-minute walk test and activities of daily living performance). The conclusions of this study revealed statistically significant differences of 54.2 meters for the training group (p=0.026) in the 6-minute walk test and in the performance of activities of daily living (p=0.003), but not in the level of dependence , evaluated using the Barthel index (p=0.072) 25.
Although CR programs have demonstrated many clinical benefits, participation rates of clients with HF range from 14% to 43% worldwide and are also associated with high dropout rates 26. Likewise, adherence to physical exercise in people with HF is a challenge, despite its benefits in functional capacity of people with HF as previously mentioned 11)(13)(15)(24)(25. Based on REPIC program results, there was an increase in the average duration of time spent performing physical exercise. Thus, we can infer that this increase was enhanced by regular telephone contacts, which allowed motivating participants to practice and reinforcing the importance and benefits of physical exercise. That said, the RN, holds specific skills in the area of readaptation, education and physical exercise training, and works as a facilitating agent in the self-care adherence and self-management behaviors, as well as an promoting agent to regular exercise practice.
CONCLUSION
The present study revealed the positive impact of the REPIC program on the level of knowledge about the disease, on the perception of quality of life and on the average time spent performing physical exercise. Thus, this RN intervention program made it possible to reinforce the educational process, enhance self-management behaviors, improve quality of life and increase the average duration of regular physical exercise.
Despite the frankly positive results, the findings must be interpreted with caution due to some inherent limitations. The time period required to carry out the study was influenced by the need to ensure the planned chronological follow-up of people with HF, and corresponded to a total of six years, in order to reach the defined sample (n=100). This is due to numerous factors, including the study's exclusion criteria; the occupancy rate of the services where the study was carried out, as well as the high number of deaths that occurred during the period in which the study was carried out (n=46). Likewise, due to a shortage of nursing human resources, the CR program was suspended for a period of 6 months, which conditioned data collection and continuity of the RN intervention program. Finally, each follow-up telephone call could reach an average duration of 40 minutes, so carrying out this study also implied a lot of personal availability and motivation.
As possible biases, it should be noted that telephone contact, as a form of non face-to-face monitoring, limited the assessment and monitoring of certain parameters, such as weight, blood pressure or functional capacity. Likewise, data provided by third parties, namely caregivers (n=17), may have somehow conditioned the results obtained. In addition, the assessment of the variables under study was based on the self-report method, which is prone to estimation error and recall bias.
Finally, we highlight the need to guarantee the continuity of care at the level of primary health care, since, to date, there is no HF nursing consultation at the hospital unit where the study was carried out, due to a lack of nursing human resources. In summary, the results of the REPIC program, as a RN intervention program, provide valuable subsidies for the replication of this program in other contexts, services or institutions.
ACKNOWLEDGMENT
The authors would like to thank all the people who made this study possible, especially the participants.
REFERENCES
1 Fonseca C, Brás D, Araújo I, Ceia F. Insuficiência cardíaca em números: estimativas para o séc. XXI em Portugal. Revista Portuguesa de Cardiologia. 2018; 32(2): 97-104. Retirado de: https://www.revportcardiol.org/pt-pdf-S087025511730745X [ Links ]
2 Pestana S, Vermelho A. Programa de enfermagem de reabilitação cardíaca intra-hospitalar em Ribeiro; O. Enfermagem de Reabilitação: conceções e práticas. Lisboa: Lidel; 2021. p.576-599 [ Links ]
3 Dessie G, Burrowes S, Mulugeta H, Haile D, Negess A, Jara D, Alem G, Tesfaye B, Zeleke H, Gualu T, Getaneh T, Kibret GD, Amare D, Worku Mengesha E, Wagnew F, Khanam R. Effect of a self-care educational intervention to improve self-care adherence among patients with chronic heart failure: a clustered randomized controlled trial in Northwest Ethiopia. BMC Cardiovascular Disorders. 2021: 21(1); 1-11. Retirado de: https://www.researchgate.net/publication/353679480_Effect_of_a_self-care_educational_intervention_to_improve_self-care_adherence_among_patients_with_chronic_heart_failure_a_clustered_randomized_controlled_trial_in_Northwest_Ethiopia [ Links ]
4 Ordem dos Enfermeiros. Guia Orientador de Boa Prática em Enfermagem de Reabilitação: Reabilitação Cardíaca. Lisboa: Ordem dos Enfermeiros; 2020. Retirado de: https://www. flipsnack.com/ordemenfermeiros/gobper/full view.html [ Links ]
5 Abreu A, Mendes M, Dores H, Silveira C, Fontes P, Teixeira M, Santa Clara H, Morais J. Mandatory criteria for cardiac rehabilitation programs: 2018 guidelines from the Portuguese Society of Cardiology. Revista Portuguesa de Cardiologia. 2018; 37(5), 363-373. Retirado de: https://www.research-gate.net/publication/325659060_Mandatory_criteria_for_cardiac_rehabilitation_pro-grams_2018_guidelines_from_the_Portu¬guese_Society_of_Cardiology. [ Links ]
6 Back M, Hansen T, Frederix I. Car¬diac Rehabilitation and exercise training recommendations; Cardiac rehabilitation: rationale, indications and core components. Retirado de: www.escardio.org/Education/ESC Prevention of CVD Programme/ Rehabilitation. [ Links ]
7 American College of Sports Medicine. Guidelines for exercise testing and prescription (10th edition). Philadelphia: Wolters Kluwer; 2018. [ Links ]
8 Piepoli MF, Corrà U, Dendale P, Frederix I, Prescott E, Schmid JP, Cupples M, Deaton C, Doherty P, Giannuzzi P, Graham I, Hansen TB, Jennings C, Landmesser U, Marques-Vidal P, Vrints C, Walker D, Bueno H, Fitzsimons D, Pelliccia A (2016). Challenges in secondary prevention after acute myocardial infarction: a call for action. European Journal of Preventive Cardiology. 2016; 23(18): 1994-2006. Retirado de: https://journals.sagepub.com/doi/pdf/10.1177/2047487316663873 [ Links ]
9 European Society of Cardiology. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2021: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2021 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. European Heart Journal. 2021; 42(36): 3599-3726. Retirado de: https://www.escardio.org/Guidelines/Clinical-Practice Guidelines/Acute-and-Chronic-Heart-Failure [ Links ]
10 Reeves GR, Whellan DJ, O'Connor CM, Duncan P, Eggebeen JD, Morgan TM, Hewston LA, Pastva A, Patel MJ, Kitzman DW. A Novel Rehabilitation Intervention for Older Patients With Acute Decompensated Heart Failure: The REHAB-HF Pilot Study. Journal of American College of Cardiology. 2017; 5(5): 359-366. Retirado de: https://www.researchgate.net/publication/352947989_Abstract_16963_A_Novel_Rehabilitation_Intervention_for_Older_Patients_with_Acute_Decompensated_Heart_Failure_the_REHAB-HF_Pilot_Study [ Links ]
11 Awotidebe T, Adedoyin R, Balogun M, Adebayo R, Adeyeye V, Oke K, Ativie R, Akintomide A, Akindele M. Effects of Cardiac Rehabilitation Exercise Protocols on Physical Function in Patients with Chronic Heart Failure: An Experience from a Resource Constraint Nation. International Journal of Clinical Medicine. 2016; 07(08): 547-557. Retirado de: https://www.scirp.org/journal/paperinformation.aspx?paperid=69830 [ Links ]
12 Sagar V, Davies E, Briscoe S, Coats A, Dalal H, Lough F, Taylor R. Exercise-based rehabilitation for heart failure: systematic review and meta-analysis. OpenHeart. 2015; 2(1): 1-12. Retirado de: https://openheart.bmj.com/content/openhrt/2/1/e000163.full.pdf [ Links ]
13 Koukoui F, Desmoulin F, Lairy G, Bleinc D, Boursiquot L, Galinier M, Rouet P. Benefits of Cardiac Rehabilitation in Heart Failure Patients According to Etiology- INCARD french study. Medicine. 2015; 94(7): 1-9. Retirado de: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4554184/ [ Links ]
14 Santa-Clara H, Pezarat-Correia P. Treino de força muscular no doente cardíaco em Sociedade Portuguesa de Cardiologia: Prevenção e Reabilitação Cardiovascular. Lisboa: Agir; 2016. p. 183-196. [ Links ]
15 American College of Cardiology Foundation/American Heart Association. 2013 ACCF/AHA Guideline for the Management of Heart Failure: a Report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Practice Guidelines. 2013: 128(16); e240-e327. Retirado de: https://www.ahajournals.org/doi/10.1161/cir.0b013e31829e8776 [ Links ]
16 Des Jarlais D, Lyles C, Crepaz N. (2004). Improving the Reporting Quality of Nonrandomized Evaluations of Behavioral and Public Health Interventions: The TREND Statement. American Journal of Public Health. 2004; 94(3): 361-366. https://doi.org/10.2105/ajph.94.3.361. Retirado de: https://pubmed.ncbi.nlm.nih.gov/14998794/ [ Links ]
17 Jaarsma T, Arestedt KF, Martensson J, Dracup K, Stromberg A et al. The European Heart Failure Self-care Behaviour scale revised into nine-item scale (EHFScB-9): a reliable and valid international instrument. European Journal of Heart Failure. 2009; 11(1): 99-105. Retirado de: http://www.ncbi.nlm.nih.gov/pubmed/19147463 [ Links ]
18 Pereira F. O Autocuidado na Insuficiência Cardíaca: Tradução, Adaptação e Validação da European Heart Failure Self-Care Behaviour Scale Para o Contexto Português. Dissertação de Mestrado em Ciências de Enfermagem. Porto, Instituto de Ciências Biomédicas Abel Salazar; 2013. Retirado de: https://repositorio-aberto.up.pt/handle/10216/70811 [ Links ]
19 Dessie G, Burrowes S, Mulugeta H, Haile D, Negess A, Jara D, Alem G, Tesfaye B, Zeleke H, Gualu T, Getaneh T, Kibret GD, Amare D, Worku Mengesha E, Wagnew F, Khanam R. Effect of a self-care educational intervention to improve self-care adherence among patients with chronic heart failure: a clustered randomized controlled trial in Northwest Ethiopia. BMC Cardiovascular Disorders. 2021: 21(1); 1-11. Retirado de: https://www.researchgate.net/publication/353679480_Effect_of_a_self-care_educational_intervention_to_improve_self-care_adherence_among_patients_with_chronic_heart_failure_a_clustered_randomized_controlled_trial_in_Northwest_Ethiopia [ Links ]
20 Dev S, Fawcett J, Ahmad S, Wu W, Schwenke, D. Implementation of early follow-up care after heart failure hospitalization. American Journal of managed care. 2021; 27(2): e42-e47. Retirado de: https://www.ajmc.com/view/implementation-of-early-follow-up-care-after-heart-failure-hospitalization [ Links ]
21 Sezgin D, Mert H, Ozpelit E, Akdeniz B. The effect on patient outcomes of a nursing care and follow-up program for patients with heart failure: a randomized controlled trial. Internacional Journal of Nursing Studies. 2017; 70: 17-26. Retirado de: https://www.sciencedirect.com/science/article/abs/pii/S0020748917300470?via%3Dihub [ Links ]
22 Son Y, Choi J, Lee H. (2020). Effectiveness of nurse-led heart failure self-care education on health outcomes of heart failure patients: a systematic review and meta-analysis. International Journal of environmental research and public health. 2020; 17(18): 1-14. Retirado de: https://www.mdpi.com/1660-4601/17/18/6559 [ Links ]
23 Oscalices M, Okuno M, Lopes M, Campanharo C, Batista R. Orientação de alta e acompanhamento telefônico na adesão terapêutica da insuficiência cardíaca: ensaio clínico randomizado. Revista Latino Americana de Enfermagem. 2019; 27; 1-9. Retirado de: https://www.scielo.br/j/rlae/a/vLpYssHvPcTqmtjZTQtnrjy/?lang=pt [ Links ]
24 Ostman C, Jewiss D, Smart N. The effect of exercise training intensity on quality of life in heart failure patients: a systematic review and meta-analysis. Cardiology. 2017;136: 79-89. Retirado de: https://www.researchgate.net/publication/307087910_The_Effect_of_Exercise_Training_Intensity_on_Quality_of_Life_in_Heart_Failure_Patients_A_Systematic_Review_and_Meta-Analysis [ Links ]
25 Delgado B, Lopes I, Gomes B, Novo A. Early rehabilitation in cardiology - heart failure: The ERIC-HF protocol, a novel intervention to decompensated heart failure patients rehabilitation. European Journal of Cardiovascular Nursing. 2020; 19(7): 592-599. Retirado de: https://pubmed.ncbi.nlm.nih.gov/32316758/ [ Links ]
26 Chun K, Kang S. Cardiac Rehabilitation in Heart Failure. International Journal of Heart Failure. 2021; 3(1): 1-14. Retirado de: https://e-heartfailure.org/DOIx.php?id=10.36628/ijhf.2020.0021 [ Links ]
Ethics Committee:The study was authorized by the Hospital Ethics Committee of the institution where it was carried out (Ref. 526/2012).
Declaration of informed consent:Written informed consent to publish this work was obtained from the participants.
Received: February 16, 2022; Accepted: January 18, 2023; Published: January 27, 2023











 text in
text in