Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista Portuguesa de Enfermagem de Reabilitação
versão impressa ISSN 2184-965Xversão On-line ISSN 2184-3023
RPER vol.2 no.1 Silvalde jun. 2019
https://doi.org/10.33194/rper.2019.v2.n1.11.4557
Articles
Intervention of the Specialist Nurse in Rehabilitation on the mobility of the institutionalized elderly person - TEIA Program
1- Curso Mestrado em Enfermagem de Reabilitação - ESEP
2- Instituto de Ação Social das Forças Armadas - CASP
3- Escola Superior de Enfermagem do Porto
4- Centro de Investigação em Tecnologias e Serviços de Saúde (CINTESIS)
5- Centro Hospitalar Póvoa de Varzim/Vila do Conde, EPE
6- Escola Superior de Saúde de Santa Maria (ESSSM)
Introduction:
Aging produces physiological, anatomical, behavioral, social and cultural changes. Arguably, the specialist nurse in rehabilitation, assumes an increasingly important role in the care provided during the aging process, through the elaboration of specialized care plans that maximize the functionality of the elderly, enabling them to have greater autonomy and independence in self-care, such that they can have a better quality of life. In this work, we present the TEIA program that focuses on the training of balance, urinary continence and cognition in active elderly.
Objective:
To assess the impact of the 12-week program on institutionalized elderly individuals on the state of balance, cognition, symptoms of urinary incontinence and quality of life.
Method:
Quasi-experimental study, before-after, with control group with a total sample of 30 elderly people, 16 in the program group and 14 in the control group. Several functional evaluation instruments were applied in the Portuguese version, namely: Falls Efficacy Scale International (FES I); Tinetti's test; Berg Balance Scale (BBS); Timed Up and Go Test (TUG); International Consultation on Incontinence Questionnaire - Short Form (ICIQ-SF); Lawton-Brody Index; Geriatric Depression Scale of 15 questions (GDS15); Cognitive Decline Test of 6 items (6CIT); and Health-related Life Questionnaire (SF-36).
Results:
Seniors in the program group improved their static and dynamic balance, fear of falling and gait execution (Tinetti, Z=-3,126, p=0,002; BBS, Z=-3,304, p=0,001; FES I, Z=-3,059, p=0,002; and TUG, Z=-3,516, p=0,0001). Additionally, the program brought them benefits in the performance of cognition (6CIT, Z= -3,088, p=0,002) and in the perception of quality of life associated with urinary incontinence (ICIQ-SF, Z=-2,680, p=0,007).
Conclusion:
The implementation of the TEIA Program led to significant gains on the health of the elderly population, improving the balance, competence of the pelvic floor muscles and the performance of cognition, resulting in enhanced the participants' quality of life.
Keywords: Aging; Balance; Urinary Incontinence; Cognition; Nursing Rehabilitation
Introdução:
O envelhecimento produz alterações fisiológicas, anatómicas, comportamentais, sociais e culturais. Indiscutivelmente, o enfermeiro especialista em reabilitação, assume cada vez mais um papel importante nos cuidados prestados durante o envelhecimento, através da elaboração de planos de cuidados especializados que maximizem a funcionalidade do idoso, capacitando-o para uma maior autonomia e independência no autocuidado, incrementando desta forma a sua qualidade de vida. Nesta perspetiva, apresentamos o programa TEIA que se foca no treino do equilíbrio, da continência urinaria e a cognição em idosos ativos.
Objetivo:
Avaliar o impacto do programa de 12 semanas, em idosos ativos institucionalizados, sobre o estado de equilíbrio, cognição, sintomatologia de incontinência urinária e qualidade de vida.
Método:
Estudo quasi-experimental, antes-depois, com grupo de controlo. Amostra total de 30 idosos, 16 no grupo de programa e 14 no grupo de controlo. Foram aplicados vários instrumentos de avaliação funcional, na versão portuguesa, nomeadamente: Falls Efficacy Scale Internacional (FES I); Teste de Tinetti; Escala de Equilíbrio de Berg (EEB); Teste Timed Up and Go (TUG); International Consultation on Incontinence Questionnaire - Short Form (ICIQ-SF); Índice de Lawton-Brody; Escala Geriátrica de Depressão de 15 questões (GDS15); Teste de Declínio Cognitivo de 6 itens (6CIT); e Questionário de vida associado à saúde (SF-36).
Resultados:
Os idosos do grupo de programa melhoraram no equilíbrio, estático e dinâmico, no medo cair e na execução da marcha (Tinetti, Z=-3,126; p=0,002; EEB, Z=-3,304; p=0,001; FES I, Z=-3,059; p=0,002 e TUG, Z=-3,516; p=0,0001). Trouxe-lhes benefícios no desempenho da cognição (6CIT, Z=-3,088; p=0,002) e na perceção da qualidade de vida associada à incontinência urinária (ICIQ-SF, Z=-2,680; p=0,007).
Conclusão:
A implementação do Programa TEIA traduz-se em ganhos significativos para a saúde dos idosos, melhorando o equilíbrio, a competência dos músculos do assoalho pélvico e no desempenho da cognição potenciado a qualidade de vida dos participantes.
Descritores: Envelhecimento; Equilíbrio; Incontinência Urinária; Cognição; Enfermagem de Reabilitação
Introducción:
El envejecimiento produce alteraciones fisiológicas, anatómicas, comportamentales, sociales y culturales. Indiscutiblemente, el enfermero especialista en rehabilitación, asume cada vez más un papel importante en los cuidados prestados durante el envejecimiento, a través de la elaboración de planes de cuidados especializados que maximicen la funcionalidad del anciano, capacitándolo para una mayor autonomía e independencia en el autocuidado, incrementando de esta forma su calidad de vida. En esta perspectiva, presentamos el programa TEIA que se enfoca en el entrenamiento del equilibrio, de la continencia urinaria y la cognición en ancianos activos.
Objetivo:
Evaluar el impacto del programa de 12 semanas, en ancianos activos institucionalizados, sobre el estado de equilibrio, cognición, sintomatología de incontinencia urinaria y calidad de vida.
Método:
Estudio cuasi-experimental, antes-después, con grupo de control. Muestra total de 30 ancianos, 16 en el grupo de programa y 14 en el grupo de control. Varias herramientas de evaluación funcional se aplicaron en la versión portuguesa, a saber: Falls Efficacy Scale Internacional (FES I); Prueba de Tinetti; Escala de Equilibrio de Berg (EEB); Prueba Timed Up and Go (TUG); Internacional Consultation on Incontinence Questionnaire - Short Form (ICIQ-SF); Índice de Lawton-Brody; Escala Geriátrica de Depresión de 15 preguntas (GDS15); Prueba de Declinación Cognitiva de 6 elementos (6CIT); y Cuestionario de vida asociado a la salud (SF-36).
Resultados:
En el caso de los ancianos del grupo de programa mejoraron en el equilíbrio, estático y dinámico, en el miedo a caer y en la ejecución de la marcha (Tinetti, Z=-3,126; p=0,002; EEB, Z=3,304; p=0,001; FES I, Z=-3,059; p=0,002 e TUG, Z=-3,516; p=0,0001). Les traen beneficios en el desempeño de la cognición (6CIT, Z=-3,088; p=0,002) y en la percepción de la calidad de vida asociada a la incontinencia urinaria (ICIQ-SF, Z=-2,680; p=0,007).
Conclusión:
La implementación del Programa TEIA se traduce en ganancias significativas para la salud de los ancianos, mejorando el equilibrio, la competencia de los músculos del piso pélvico y en el desempeño de la cognición potenciada la calidad de vida de los participantes.
Palabras clave: Envejecimiento; Equilibrio; Incontinencia Urinaria; Cognición; Enfermería de Rehabilitación
INTRODUCTION
Improving the quality of life in old age is one of the biggest challenges of our time. But aging with quality of life requires measures and interventions that allow the elderly to be integrated into society, family, institutions, with the means of subsistence and necessary support. It is noteworthy that health care and social support are as important as the active participation of the individual to achieve this goal1,2.
Given the demographic trend of the Portuguese population, characterized by an increase in human longevity and a decrease in birth rates3,4, it is necessary to adapt the care we provide throughout life, especially the specific care in old age where Rehabilitation nursing has a fundamental role, not only in the creation of scientific evidence to support the elaboration of specific and specialized care plans, but also in their execution.
To achieve this purpose, it is essential to understand that aging can lead to the deterioration of various physiological capacities (such as muscle strength, aerobic capacity, neuromuscular coordination, flexibility, among others) which in turn can lead to decline of physical and mental performance, with consequences for the quality of life, well-being and self-care performance, activities of daily living and instrumental activities of daily living5.
Thus, the concept of functional capacity has attracted a growing concern to health professionals, especially rehabilitation nurses, permanently looking for strategies to improve and/or maintain the functional abilities of the elderly people.
Aging is part of the life cycle and as such, it is logical to value it, essencially because it is an opportunity for a enriched society. Aging is often related to the decline of physical and mental faculties, an aspect that associates it with a negative image, which should be avoided at all costs, similarly associated with diseases, loss of autonomy and independence and the consequent withdrawal from social roles6.
Aging cannot be seen as a process of only losses, being possible through the action of behavioral, social, economic and environmental interventions, people can actively age by living longer years with a better quality of life, reducing their dependence and enhancing their autonomy7-9.
The ability to preserve and/or enhance autonomy and independence, increasing the quality of life, in the elderly, is related to the surveillance of health status, the type of health care experienced, the environments in which they live, as well as the adoption of lifestyles10.
In the last EVITA System report of Doctor Ricardo Jorge National Health Institute Instituto Nacional de Saúde Doutor Rivardo Jorge), the injury mechanisms that most contributed to the number of Domestic and Leisure Accidents (DLA) are falls (68.7%), standing out in a pronounced manner as the biggest cause of DLA. It is emphasized that the group with the highest occurrence of falls are female aged 75 years-old or over11.
According to Swift and Iliffe (2014) there are some risk factors that may contribute to falls in the elderly people, namely: history of falls; postural instability; mobility problems; balance problems; continence problems; cognitive impairment; health problems; medication; syncope syndrome; and visual impairment12. It appears that changes in balance, urinary continence and cognition are determinant for the occurrence of falls in seniors.
There are several evidence that support the beneficial effects of balance training, such as: the reduction in fear of falling; the reduction in the number of falls; the improvement of balance performance; improving gait execution, resulting in increase of life quality13-15.
Associated with the advantages of balance training, training the pelvic floor muscles in situations of urinary incontinence is essential. Urinary incontinence can be a very limiting symptom. The fact that the elderly may have, for example, urge urinary incontinence, obliges them to have a quick physical response to reach the toilet before the loss of urine occurs. This type of situation can lead to loss of balance and consequently to falls16-18.
Cognition and motor control are closely related, body movement in general is not performed in the absence of intention, so cognitive processes are essential for motor control5,19, playing a vital role in daily life activities and in instrumental activities of daily living, as well as in the combination of various activities of daily living and instrumental activities of daily living in parallel20.
The construction of the TEIA Program in active elderly people took into account these three variables, body balance, urinary continence and cognition. Considering the components that it integrates, this program is essential to strengthen the functionality of the elderly, enabling them to preserve their independence and autonomy. In this sense, this study aims to evaluate the impact of the implementation of the TEIA program on the state of balance, symptoms of urinary incontinence, cognition, and quality of life in active institutionalized elderly people.
METHOD
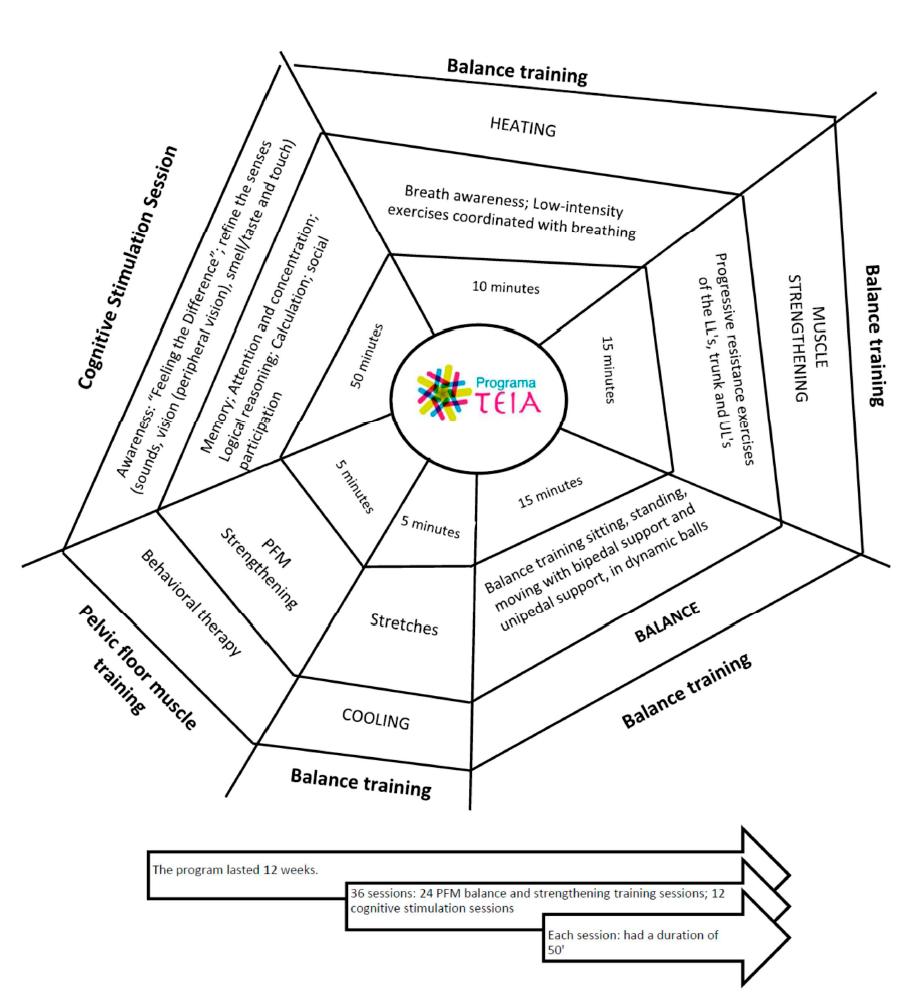
This was a quasi-experimental, before-after, control group study. Lasting 12 weeks, the program group had two weekly sessions of balance training and pelvic floor muscle training and one weekly session of cognitive stimulation interspersed (Figure 1) and the control group was not subjected to the intervention.
The sampling technique used was non-probabilistic, accidental. The inclusion criteria were: individuals over 65 years-old, with preserved gait and institutionalized. Exclusion criteria: individuals with: (i) mental illness that limited the understanding of the object of study, as well as the content of the program sessions; (ii) or with comorbidity that prevents physical exercise.
Authorization was obtained from the two institutions, the Armed Forces Social Action Institute (Instituto de Ação Social das Forças Armadas - IASFA) - Porto Social Support Center (Centro de Apoio Social do Porto - CASP) and the Santa Casa da Misericórdia do Porto - Home of Nossa Senhora da Misericórdia. In this study, all ethical and deontological requirements regarding scientific research were met and guaranteed.
A total of 32 institutionalized elderly people participated in this study, having been divided into a program group and a control group, 17 and 15, respectively. There was one dropout in the program group and one death in the control group. At the end of the study the program group had 16 participants and the control group had 14 participants (Figure 2).
To assess the impact of the TEIA Program, a registration survey was constructed based on the variables operationalized in the table (Table 1).
Table 1 Harvesting Variables and Instruments
| Variables | Dimensions |
|---|---|
| Sociodemographic | Age; sex; marital status; education. |
| Physiological measures | Blood Pressure (BP); Heart rate (HR); Anthropometric measurements (weight, height and BMI) |
| Clinical data | History of chronic disease(s) |
| Perception of quality of life associated with urinary incontinence. | International Consultation on Incontinence Questionnaire - Short Form (ICIQ-SF)22 |
| Fear of Falling Assessment. | Falls Efficacy Scale International (FES I)23 |
| Balance changes | Tinetti Test24; Berg Balance Scale (BBS)25 Time Up and Go Test (TUG)26 |
| Independence in IADL | Lawton- Brody’s index27 |
| Depressive state | 15-question Geriatric Depression Scale (GDS15)28 |
| Cognition | 6-item Cognitive Decline Test (6CIT)29 |
| Perception of quality of life associated with health | Health Associated Life Questionnaire (SF-36)30 |
Descriptive and inferential statistical analysis was performed, using parametric tests, namely the Student t-test, for inter-subject assessment and the Paired Samples t-test for intra-subject analysis, and in certain cases, the respective non-parametric tests, the Mann-Whitney and the Wilcoxon test. The level of significance adopted was 0.0521. The software used for data treatment and statistical analysis was IBM® SPSS® Statistics version 24.
RESULTS AND DISCUSSION
The total sample (n=30) was characterized by an average age of 83.3 years-old, the median of 84 years. Age ranged from 67 years-old to 93 years-old, with a standard deviation of 6.32 years, with an equal representation between gender, 50% men and 50% women, both in the sample and in the groups. Regarding marital status, the most representative groups are married and widowed, either in the sample (40% married and 43.3 widowed) or in the groups (program group - 43.8% married and 43.8% widowed; control group - 35.7% married and 42.9% widowed). Regarding educational qualifications, the one with the greatest representation in the sample was the 1st cycle (40.0%), followed by the 3rd cycle (30.0%). In the groups, the trend was the same (Table 2).
Table 2 Sample Characterization
| Sociodemographic characteristics | Program Group (PG) | Control Group (CG) | Total of sample | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | n | n | % | ||
| Participants | 16 | 53.3 | 14 | 46.7 | 30 | 100 | |
| Average Age (() | 83 (5.56) | -- | 83 (7.32) | -- | 83 (6.33) | -- | |
| Sex | Female | 8 | 50.0 | 7 | 50.0 | 15 | 50.0 |
| Male | 8 | 50.0 | 7 | 50.0 | 15 | 50.0 | |
| Marital status | Single | 0 | 0 | 2 | 14.3 | 2 | 6.7 |
| Married | 7 | 43.8 | 5 | 35.7 | 12 | 40.0 | |
| Separated/ Divorced | 2 | 12.5 | 1 | 7.1 | 3 | 10.0 | |
| Widowed | 7 | 43.8 | 6 | 42.9 | 13 | 43.3 | |
| Education | 1st Cycle | 5 | 31.3 | 7 | 50.0 | 12 | 40.0 |
| 2nd Cycle | 4 | 25.0 | 1 | 7.1 | 5 | 16.7 | |
| 3rd Cycle | 5 | 31.3 | 4 | 28.6 | 9 | 30.0 | |
| Secondary | 1 | 6.3 | 0 | 0.0 | 1 | 3.3 | |
| Higher education | 1 | 6.3 | 2 | 14.3 | 3 | 10.0 | |
Analysis of the implementation of the TEIA Program
Before the program
In the evaluation carried out before the program, it was found that in all variables, except the mean body mass index (BMI) and the perception of quality of life associated with health in the physical performance dimension, the p value had a value greater than 0.05, meaning that there were no statistically significant differences between the program and control groups, inferring the similarity of the groups.
After the program
About Physiological Measurements: in the program group, from the 1st to the 2nd assessment, the mean systolic value of 139 mmHg changed to a value of 127 mmHg and the mean diastolic value went from 77 mmHg to 72mmHg. The average heart rate of 81 bpm increased to 74 bpm.
In the program and control group, there was an average weight of 73,069 kg and 68,585 kg, respectively, in the 1st evaluation. In the 2nd evaluation, the average weight changed to 72,025Kg in the program group; and 70,000Kg in the control group.
These differences in values were reflected in the BMI value. In the 1st evaluation, the program group had a value of 28.30 and in the 2nd evaluation a value of 27.93. The control group, in the 1st evaluation had a value of 25.39 and in the 2nd evaluation a value of 25.89.
These changes in weight and consequently in the value of BMI led to a repositioning regarding the categorization of BMI, there was a variation in the number of people in the program group, which changed from the obese grade I category to pre-obese, that is, in the 1st assessment 43.8% were pre-obese and 31.3% were obese class I. In the 2nd assessment, the percentage of pre-obese individuals rose to 56.3% and the percentage of class I obese individuals rose to 18.8%. In the control group, in the 1st assessment, 50% were pre-obese, 41.9% normal and 7.1% grade I obese and in the 2nd assessment 42.9% pre-obese, 35.7% normal and 21.9 % obese class I.
In the intra-subject analysis, in the program group, all physiological measures had a decrease, with statistically significant changes for blood pressure values, systolic value (t (15) =4.522; p=0.0001) and diastolic value (t ( 15) =2.698; p=0.017); heart rate (t (15) =3.335; p=0.005); weight (t (15) =2.427; p=0.028) and BMI (t (15) =2.318; p=0.035). The same is not true in the control group, since in the variables blood pressure (diastolic and systolic) and heart rate the op value is greater than 0.05, so there were no statistically significant changes in their values from the 1st to the 2nd assessment (t (13)=-2.649; p=0.020). In relation to the BMI (t(13)=-2.370; p=0.034), in this group, there were statistically significant changes, but with an opposite tendency to the program group. When the inter-subject evaluation was performed, it was found that there were no statistically significant changes.
On the perception of quality of life associated with urinary incontinence (ICIQ-SF): The average score of the 1st evaluation in the program group, compared to the 2nd evaluation, decreased significantly, from an average value of 4.19 points to a value of 2.44 points. In the control group, there was an increase in the mean value from 4.93 points to 6.50 points. In this variable, as the distribution is not normal, the Wilcoxon test was used and it was found that there were statistical differences from the 1st to the 2nd evaluation, either for the program group (Z=-2.680; p=0.007) or for the control group (Z=-2.375; p=0.018). When the inter-subject analysis was performed, it was found that there were statistically significant differences between the program group and the control group regarding the 2nd evaluation (U=44,000; p=0.004) (Table 3).
About Cognition (6CIT): The mean score in the program group went from 7 to 4 points, the maximum values from 19 to 14 points and the standard deviation from 6 to 5 points. In the control group, the average score went from 5 to 7 points, maintaining the maximum value and standard deviation. In the intra-subject evaluation, it was found that in the program group there were statistically significant differences (Z=-3.088; p= 0.002) but in the control group there were no statistical differences (Z=-1.901; p=0.57). In the inter-subject evaluation, it was verified that there were no statistical differences (U=72.500; p=0.101) (Table 3).
Table 3 ICIQ-SF and 6 CIT score results.
| Variable | Outcomes | PG (n=16) | CG (n=14) |
p value ( between groups |
||||
|---|---|---|---|---|---|---|---|---|
| 1st evaluation |
2nd evaluation |
p value 1 st and 2 nd evaluation |
1st evaluation |
2nd evaluation |
p value 1 st and 2 nd evaluation |
|||
| Perception of quality of life associated with urinary incontinence Average score (() |
ICIQ-SF Max: 21 Min: 0 |
4.19 (5.09) |
2.44 (5.02) | 0.007 | 4.93 (5.48) |
6.50 (5.26) | 0.018 | 0.004 |
| Cognition Average score (() |
6CIT Max:28 Min: 0 |
7 (6) |
3.56 (4.99) | 0.002 | 5 (7) |
6.79 (7.13) | 0.573 | 0.101 |
About Fear of Falling (FES-I) and Balance (Tinetti Test, Berg Balance Scale, Timed Up and Go Test): With regard to the variable “fear of falling” analyzed using the FES-I scale, in the program group, the initial average score was 75 points and the final 85 points, and in the control group the average score increased from 82 points to 78 points. When performing the intra-subject analysis, it was found that in the program group there were statistical differences between the 1st evaluation and the 2nd evaluation (Z=-3.059; p=0.002), whereas in the control group there were no statistical differences (Z=-2.366; p=0.18). There were also no statistically significant differences between groups after program implementation (U=111,000; p=0.966).
Regarding the balance assessment, as shown in table 4, in the program group in the 1st assessment the average score was 23 points, passing in the 2nd assessment to 26 points. In the control group, the average score was 24 points, rising to 23 points in the 2nd assessment. Analyzing the Tinetti Test score, in the intra-subject evaluation, taking into account its total value, it was found that there were significant differences between the 1st and 2nd evaluations, in the program group (Z=-3.126; p=0.002), but not in the control group (Z=-2.271; p=0.23). In the inter-subject evaluation, it was found that in the 1st evaluation there were no differences between the groups (U=101,000; p=0.667), but in the 2nd evaluation, there were statistically significant differences between the program group and the control group (U=60,000; p=0.031).
The Berg Balance Scale score in the program group went from an average of 44 points to an average of 49 points. The control group went from 42 points to 39 mean points. There was also a change in the mode of scores from the 1st to the 2nd assessment, in the program group it went from 50 to 52 points, in the control group it went from 49 to 42 points. Transposing to the intra-subject assessment, it was found that there were statistically significant differences, both for the program group (Z=-3.304; p=0.001) and for the control group (Z=-3.203; p=0.001). In the inter-subject evaluation, it was found that there were also statistically significant differences in the 2nd evaluation, confirmed by the Mann-Whitney test (U=36,000; p=0.001) (table 4).
Regarding the time needed to perform the Timed Up and Go test, it was found that in the program group an average value of 20.16 sec., a maximum value of 44.17 sec. and a minimum value of 9.74 sec., the average value was 16.66 sec., a maximum value of 40.20 sec. and a minimum value of 7.71 sec. In the control group, it went from an average value of 20.66 sec. to 24.07 sec., the maximum value increased from 44.19 sec. for 45.20 sec. and the minimum value of 11.39 sec. to 12.27 sec. In the intra-subject evaluation, it was found that there were statistically significant differences from the 1st to the 2nd evaluation, either in the program group (Z=-3.516; p=0.0001) or in the control group (Z =-3.296; p=0.001). In the inter-subject evaluation, it was found that there were statistically significant changes in the 2nd evaluation (U=55,000; p=0.017) (Table 4).
Table 4 Results for the Tinetti Test, Berg Balance Scale, Timed Up and Go Test and FES-I.
| Variable | Outcomes | PG (n=16) | CG (n=14) |
p value ( between the groups |
||||
|---|---|---|---|---|---|---|---|---|
| 1st evaluation | 2nd evaluation |
p value 1 st and 2 nd evaluation |
1st evaluation | 2nd evaluation |
p value 1 st and 2 nd evaluation |
|||
| Balance Average score (() |
Tinetti’s test Max: 28 Min: 0 |
23 (4) |
25.88 (3.01) |
0.002 | 24 (4) |
23.07 (4.34) | 0.231 | 0.031 |
| BBS Max:56 Min: 0 |
44 (7) |
49.00 (6.46) |
0.001 | 42 (8) |
39.00 (8,73) | 0.001 | 0.001 | |
| TUG Test Seg. |
20,16 (9,93) |
16.67 (9.68) |
0.0001 | 20.60 (9,49) |
24.07 (11.31) | 0.001 | 0.017 | |
| Fear of falling Average score (() |
FES I Max:100 Min: 0 |
75 (24) |
85.19 (14.76) | 0.002 | 82 (28) |
78.07 (32.15) | 0.018 | 0.984 |
In the analysis of Independence in instrumental activities of daily living (Lawton-Brody Index): For the Lawton-Brody Index score, the mean values remained from the 1st to the 2nd assessment in both groups. Analyzing each item of the scale, for the program group, it was found that, in the item “Taking care of the house”, 37.5% “Taking care of the house without help” and maintained a score in the 2nd evaluation; in the answer "I do everything except heavy work", from 12.5% it went to 18.8%, and in the answer "I do light tasks", from 43.8% went to 37.5% in the 2nd evaluation. In the item "Preparing food", 50% went to 62.5% in the answer "I plan, prepare and serve my meals without help" and 37.5% went to 25% in the answer "I prepare if you give the ingredients". In the item “Going shopping”, 43.8% said they were “unable to go shopping” and in the 2nd evaluation it decreased to 37.5%; in the answer “do the shopping accompanied” from 18.8%, it went up to 25%. In the item "use of transport" it was found that 25% went to 18.8% in the answer "I need follow-up" and in the inverse proportion, from 18.8% went to 25% in the answer "I only take a taxi”.
In this variable there were no statistically significant differences either in the intra-subject or inter-subject assessment. This evidence is confirmed by the intra-subject analysis, where there were no statistically significant differences from the 1st to the 2nd evaluation, in the program group (Z=-1.633; p=0.102) and in the control group (Z=-1.342; p=0.180) and accordingly, in the inter-subject evaluation there were also no statistical differences between the 2nd evaluation (U=99.500; p=0.608).
On Depressive State (15-question Geriatric Depression Scale): The program group had an average of 4 points, either in the 1st or 2nd evaluation. Through the frequency of cumulative percentages, it was found that the number of participants within the cutoff points of 0-5 points, in this group, increased from 56.3% to 68.8%, from the 1st to the 2nd assessment. The control group had an average score of 5 points in the 1st assessment and increased to 6 points in the 2nd assessment. In this variable, in the intra-subject evaluation, according to the Wilcoxon test, there were no statistical differences in the program group (Z=-1.121; p=0.262), and in the control group there were statistical differences (Z=-2.232; p=0.026), since there was an increase in the 15-question Geriatric Depression Scale. In the inter-subject evaluation, it was found that there were no statistically significant differences between the groups in the 2nd evaluation (U=71.500; p=0.091).
From the analysis of the Perception of Health-Associated Quality of Life (SF-36 Health-Associated Life Questionnaire): When we grouped the dimensions of the SF-36 Health-Associated Life Questionnaire into physical component (physical function, physical performance, pain and health in general) and in the mental component (vitality, social function, emotional performance and mental health), it was found that in the sample, there was a variation from the 1st to the 2nd assessment. The average value of 54% went to 66% for the physical component, and in the mental component, it went from an average value of 68% to 78%. In the inter-subject evaluation, we can affirm that there were statistically significant differences, in the program group, either in the physical component (Z=-3.077; p=0.002), or in the mental component (Z=-2.552; p=0.011). In the control group there were no differences in the physical component (Z=-1.454; p=0.146), and in the mental component there were statistical differences, but in the opposite direction, that is, there were losses (Z=-2.805; p=0.005). In the inter-subject evaluation, it was verified that there were differences between the groups in the mental component in the 2nd evaluation (U=62,000; p=0.038) that did not exist in the 1st evaluation (U=103,500; p=0.728). In the physical component there were no statistically significant differences between the groups, neither in the 1st (U=95.500; p=0.498) nor in the 2nd assessment (U=81,000; p=0.208).
Inter-subject evaluation (1st evaluation)
With regard to the inter-subject evaluation in the 1st evaluation, it is important to point out some data.
Regarding the distribution of the gender variable, either in the total sample or in the two groups that constitute it, the distribution was equal and with a representation of 50% for each of the genders, unlike most studies where there was a greater representation of the female gender34,35, as well as, in the Portuguese population, between the age group 80-84 years-old, the average age in our study, where about 62% of the population is female3.
As for marital status, they are married and widowed with greater expression, followed by separate/divorced and single marital status in both study groups, analogous to the study by Possamai Menezes et al.36. The distribution of educational qualifications showed that 50% or more of the participants in both groups had educational qualifications higher than the 1st cycle, coinciding with another study33.
Regarding the other variables, in the inter-subject analyzes in the 1st assessment, confirmed with the respective statistical tests, it was found that the groups did not have statistically significant differences, except for the BMI value and the physical performance dimension of the life questionnaire associated with health SF-36. This allowed us to conclude that the groups before the implementation of the TEIA program were very equivalent, thus contributing to guarantee the internal validity of the study. Given that the more similar the program and control groups are in recruitment and the more these similarities are confirmed by the tests of the 1st assessment, the more effective this control will be21.
Intra-subject evaluation (program group)
There were several findings that met with the implementation of the program, namely: the reduction in blood pressure, the decrease in heart rate, the decrease in weight and consequently the BMI and repositioning in the BMI categories. As well as the change in the perception of quality of life associated with urinary incontinence; the decrease in fear of falling; better balance performance; improvement in cognitive aptitude and variation in the perception of health-related quality of life.
The systolic and diastolic value, in the program group, suffered a statistically significant decrease. Based on the norm on arterial hypertension defined by the General Directorate of Health, 2013, the systolic values changed from a high normal classification to a normal classification. The diastolic values, on the other hand, maintain an optimal classification37. The value of heart rate at rest from the 1st to the 2nd evaluation decreased, this finding is in agreement with the relationship that exists between the effect of physical activity and the decrease in HR at rest38.
Now approaching the assessment of weight and BMI, it was found that in the intra-subject assessment of the program group there was weight loss, on average of 1kg and consequently the BMI also decreased, leading to a repositioning of the BMI category. Although this average value maintains this sub-sample in the pre-obese category, it is noteworthy that there was a variation in the number of people who went from the obese grade I category to pre-obese. Once again, the relationship between physical activity and the reduction in weight and BMI was proven39.
The perception of quality of life associated with urinary incontinence was assessed through the International Consultation on Incontinence Questionnaire - Short Form; it was found that there was a decrease in the mean score of the questionnaire. Contributing to this score reduction was the tendency of score decrease in all the questions in the questionnaire that contribute to the final score. This variation in results can be attributed to the analysis that was carried out to question 6, in the first assessment, which in this way allowed us to understand which types of urinary incontinence were more frequent, in the sub-sample, and thus adapt to more effective strategies to reduce the frequency, the quantity and impact of urinary incontinence, proving the relationship between pelvic floor muscle training and behavioral therapy as predictors of improved quality of life associated with urinary incontinence40,41.
Analyzing now the Falls Efficacy Scale I score, it was found that there were differences between the 1st and 2nd assessment in the program group, with the average score increasing. Through these values, it was found that the fear of falling decreased, since the participants are more confident in performing the 10 tasks that the scale includes, thus enhancing the association between balance training and fear of falling35,42.
The scores of the Tinetti test, Berg Balance Scale and Timed Up and Go test also changed from the 1st to the 2nd assessment. In the Tinetti Test and in the Berg Balance Scale, the average score increased and the mode of the scores was also in favor of the trend towards an increase in the score. The average time of the Timed Up and Go test decreased from the 1st to the 2nd assessment. Through these results, we can attest that program group participants improved mobility and consequently improved gait, balance, static and dynamic performance, which may be a predictor of decreased risk of falling in the elderly31,33,43.
When analyzing the performance of the participants in relation to the execution of instrumental activities of daily living, it was found that there were no statistically significant differences between the 1st and 2nd assessments, and the average score of the Lawton-Brody Index remained. However, in the analysis of the score variation for each item in the Index, it was found that there were statistical differences in the responses to the items "Taking care of the house", "Preparing food", "Going shopping" and "Use of transportation", or that is, the answers that confer greater independence had an increase from the 1st to the 2nd assessment. The above leads us to infer that the participants felt more confident in performing domestic tasks, such as taking care of the house and preparing food, as well as going abroad.
The relationship between fear of falling, quality of life and performing instrumental activities of daily living was established in the studies by Jahana and Diogo, 2007 and Fhon et al., 2012. Effectively, the TEIA Program contributed to reducing the fear of falling, but despite the fact that the average score did not change, it was evident that in certain instrumental activities of daily living there was an improvement in the confidence to perform them, namely, in the instrumental activities mentioned above. Similar results have been obtained in other studies44,45.
Also, in the analysis of the 15-question Geriatric Depression Scale, it was found that there were no statistical changes in the intra-subject analysis. It was found that in the program group, the mean score of the participants remained in the cohort points suggestive of “no depressive symptoms”. Allied to this data was the fact that there was an increase in the percentage of the number of participants, who moved to this classification.
The fear of falling and the frequency of falls can make the elderly person more anxious and more depressed, therefore it leads to social isolation, decreased physical activity, spending more time sitting or lying down, impairing mobility and independence in self-care. We have already verified with the implementation of the TEIA Program, the participants reduced their fear of falling and this factor can be reflected in depressive symptoms44-46.
The decay of cognitive function can lead to an increase in the number of falls in the elderly population, and for this reason, cognitive stimulation was included in the structure of the TEIA Program. The average score of the 6-item Cognitive Decline Test scale, from the 1st to the 2nd assessment in the program group, decreased, suggesting better cognitive performance, which means that the implementation of a cognitive stimulation program for the elderly population contributes to a better performance in cognitive functions32.
Guszman et al., 2015 established the relationship between fear of falling and cognition, that is, when the first increases, the second is declining, with an intrinsic relationship between cognition and the level of physical activity, which can lead to limited mobility, meaning, mobility is affected by cognition if it limits physical activity47. The TEIA Program was shown to improve confidence, mobility, gait performance and balance, leading to a reduction in fear of falling. It also improved the performance of cognition, soon the cognitive functions, namely those related to the fear of falling, prospered. The relationship between the training of cognition and the fear of falling was evidenced.
It was our intention to understand how the TEIA Program interfered with the quality of life associated with the health of the participants. Through the scores of the SF-36 Health Associated Life Questionnaire, in its various dimensions, it was found that in the intra-subject evaluation of the program group, there were statistically significant differences, both in the physical component (physical function, physical performance, pain and general health) or in the mental component (vitality, social function, emotional performance and mental health). The aforementioned, proves that the TEIA Program had a positive implications for the quality of life of the participants31,48.
Regarding the intra-subject evaluations of the program group, it was validated that the TEIA Program introduced statistically significant changes in the quality of life associated with urinary incontinence, fear of falling, balance performance, whether static or dynamic, mobility, gait, in some instrumental activities of daily living, in depressive symptoms, cognitive function and health-related quality of life. In all these variables, there was an improvement in their performance, which translates into better physical and mental performance, as well as benefits in the perception of quality of life. Training allowed for secondary gains, such as the decrease in tension values, heart rate, weight and BMI.
Inter-subject evaluation 2nd assessment
With regard to the inter-subject assessment, after the implementation of the TEIA Program, it was found that in the perception of quality of life when it is associated with urinary incontinence, there were statistically significant differences, findings in agreement with the study by Berlezi et al., 201349 showing again the relation between pelvic floor muscle training and behavioral therapy, and the perception of quality of life associated with urinary incontinence.
Regarding the assessment of fear of falling, it was found that although there was a decrease in fear of falling after the implementation of the TEIA Program in the program group, there were no statistically significant differences between the program group and the control group, a very similar result to that found in other studies31,42, this fact may be related to the sample size.
When examining the scores of the Tinetti test, Berg Balance Scale and the running time of the Timed Up and Go test, it was found that there were statistically significant differences. We can conclude that the TEIA Program, in its balance training component, managed to improve static and dynamic balance, mobility, gait, stability in walking, which indirectly produced a decrease in the risk of falling in agreement with the findings of other studies13,33,42, contributing to the evidence of the relation between balance training and decreased risk of falls in the elderly people.
In the assessment of dependence on instrumental activities of daily living and depression, it was validated that there were no differences between groups. In a study on cognitive stimulation by Apóstolo et al., 2011 findings were the same, although they showed gains in the intra-subject evaluation in the program group, as happened after the implementation of the TEIA Program11, attributing this data to the sample size.
In the cognition variable, despite the statistically significant differences, in the intra-subject evaluation in the program group, it was found that there were no statistically significant gains between the groups. We can infer that this analysis may be related to the fact that the sample is small to support this difference. No studies were found that used only the 6-item Cognitive Decline Test scale, in order to relate the results.
The statistically significant differences observed in the intra-subject assessment, regarding the perception of quality of life associated with health, were not confirmed in the inter-subject assessment for the physical component. It’s different evidence to what was found in the study by Kyrdalen et al., 2013, in which there were differences between groups in the physical component, but not in the mental component31.
In short, the 2nd evaluation showed intergroup differences in the perception of quality of life associated with urinary incontinence, in balance performance, in gait, in the perception of quality of life associated with health in the mental component. There were no statistically significant changes in the cognition variable, which may be related to the fact that the study sample was small.
CONCLUSION
Aging enriches the Human Being with life experiences, increased resilience and the capacity to face the vicissitudes that arise. But aging also brings about the maturation of organs and consequent physiological and anatomical changes in the body, which may or may not translate into dependence and/or loss of autonomy. These alterations can interfere with the gait behavior, the speed of postural changes, the ability to adopt compensatory mechanisms for maintaining balance, the balance performance, the competence of the pelvic floor muscles and the performance of cognition.
The TEIA Program was designed to contemplate several dimensions, from balance training, pelvic floor muscle training to cognitive stimulation. We found that these three dimensions, if worked together, produce positive effects on the life quality, correlating to a reduction in the falls risk, favoring independence, low levels of dependence and the autonomy in the elderly.
The implementation of this program, not only gave contribution to the elderly population, helping to raise their functional potential, but also to the nursing community, namely, to rehabilitation nurses. The rehabilitation nurse has a important role in adopting attitudes that promote active aging, as they optimize the functional potential, promote independence and autonomy, increasing elderlies quality of life, as strengthen physical and mental skills that make it possible to overcome the limitations of that aging produces, which makes it possible to rationalize human and financial resources.
Being TEIA Program a specific physical activity and behavioral program for the three dimensions already described, it was found that its implementation allowed for primary and secondary gains. As secondary gains, it was found that teaching and awareness of breathing times as the constituent part of balance training sessions, allowed to increase aerobic capacity and tolerance to cardiovascular effort, causing a decrease in the mean value of blood pressure and heart rate.
Another secondary gain was weight loss, probably related to the continued practice of physical activity. Participants in the program group lost an average of one kilogram and consequently decreased their body mass index value. Another secondary factor is related to quality of life, which generally improved, as it was found that there were statistical differences in the perception of quality of life associated with health in the mental component.
As primary gains, the effectiveness of static and dynamic balance performance, improved mobility, improvement in gait ability, improved performance and muscle competence of the pelvic floor, which in association with behavioral therapy, potentiated the increased quality of life associated with urinary incontinence, as well as the performance of cognitive functions.
All these benefits made it possible to prove the importance of this type of exercise program in this type of population, with the TEIA Program being an asset for the elderly and for the professionals who take care of them.
A fundamental limitation of the study was the fact that the sample was small, which may have limited certain statistical findings. It was also considered a limitation the fact that there was not a 3rd evaluation to be carried out within a period after the completion of the program implementation to further highlight the need for frequent physical activity, aimed at training the dimensions, balance, urinary continence and cognition.
As a future work, it would be important to confirm the conclusions of this study with other studies with larger samples to corroborate the benefits of implementing this type of program. It would also be important to carry out a reassessment of the participants after a period without the activities inherent to the program, in order to verify the existence of complications intrinsic to the lack of training.
REFERÊNCIAS BIBLIOGRÁFICAS
1 São José J. de, Teixeira A. Envelhecimento ativo: contributo para uma discussão crítica. análise social, Revista do Instituto de Ciências Sociais da Universidade de Lisboa. 2014;210. ISSN:0003-2573 [ Links ]
2 Paúl M, Ribeiro O. Manual de envelhecimento ativo. 2nd ed. Lisboa: Lidel; 2018. ISBN:978-989-752-333-5 [ Links ]
3 Instituto Nacional de Estatística. Instituto Nacional de Estatística - Statistics Portugal. [Web page] Lisboa: Instituto Nacional de Estatística, 2017. [Updated 2019; cited 2019 09 Janeiro] Available from: https://ine.pt/xportal/xmain?xpid=INE&xpgid=ine_bdc_tree&contexto=bd&selTab=tab2. [ Links ]
4 Eurostat. Estrutura populacional e envelhecimento. Eurostat Statistics Explained. [Web page]: Eurostat; 2018 [Updated 2018; cited 2019 09 Janeiro] Available from: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Population_structure_and_ageing/pt#A_percentagem_de_idosos_continua_a_aumentar. [ Links ]
5 Kalsait, A., Lakshmiprabha, R., Iyyar, S. e Mehta, A. Correlation of Cognitive Impairment with funcional Mobility & Risk of Fall in Elderly Individuals. Indian J Physiother Occup Ther. 2017; 11(2): pp7-11. [ Links ]
6 Schneider, R. e Irigaray, T. O envelhecimento na atualidade: aspetos cronológicos, biológicos, psicológicos e sociais. Campinas. Estud Psicol. 2008; 25(4): pp.585-593. [ Links ]
7 Sequeira, C. Cuidar de idosos com dependência física e mental. 1ed. Lisboa: Lidel; 2010. ISBN: 978-972-757-717-0. [ Links ]
8 Saúde, Organização Mundial de. Relatório Mundial de Envelhecimento e Saúde. 1ed. Genebra: World Health Organization; 2015. [ Links ]
9 Saúde, Direção Geral de. Estratégia Nacional para o Envelhecimento Ativo e Saudável 2017-2025, Proposta do Grupo de trabalho Interministerial (Despacho nº 12427/2016). Lisboa: DGS; 2017. [ Links ]
10 Firmino, H., Simões, M. e Cerejeira, J. Saúde Mental das Pessoas Mais Velhas. 1ed. Lisboa: Lidel; 2016. ISBN: 978-989-752-147-8. [ Links ]
11 Jorge, Instituto Nacional de Saúde Doutor Ricardo. EVITA-Epidemiologia e Vigilância dos Traumatismos e Acidentes: relatório 2009-2012. 1ed. Lisboa: INSA,IP; 2014. ISBN: 978-989-8794-00-0. [ Links ]
12 Swift CG, Iliffe S. Assessment and prevention of falls in older people-concise guidance. Clin Med. [Internet]. 2014 Dec 1 [cited 17 June 2019]; 14(6):658-62. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4954140/ [ Links ]
13 Gouveia BR, Jardim HG, Martins MM, Gouveia ÉR, de Freitas DL, Maia JA, Rose DJ. An evaluation of a nurse-led rehabilitation programme (the ProBalance Programme) to improve balance and reduce fall risk of community-dwelling older people: A randomised controlled trial. Int J Nurs Stud. 2016 Apr 1;56:1-8.. [ Links ]
14 Barban F, Annicchiarico R, Melideo M, Federici A, Lombardi M, Giuli S, et al. Reducing fall risk with combined motor and cognitive training in elderly fallers. Brain Sci. 2017 Feb 10;7(2):19. [ Links ]
15 Marques EA, Figueiredo P, Harris TB, Wanderley FA, Carvalho J. Are resistance and aerobic exercise training equally effective at improving knee muscle strength and balance in older women?. Arch Gerontol Geriatr. 2017 Jan 1;68:106-12. [ Links ]
16 Madill SJ, Pontbriand-Drolet S, Tang A, Dumoulin C. Effects of PFM rehabilitation on PFM function and morphology in older women. Neurourol Urodyn. 2013 Nov;32(8):1086-95.. [ Links ]
17 Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010 Jan;29(1):213-40. [ Links ]
18 Kim H, Yoshida H, Suzuki T. The effects of multidimensional exercise on functional decline, urinary incontinence, and fear of falling in community-dwelling elderly women with multiple symptoms of geriatric syndrome: a randomized controlled and 6-month follow-up trial. Arch Gerontol Geriatr. 2011 Jan 1;52(1):99-105. [ Links ]
19 Shumway-Cook, A. e Woollacott, M. Motor Control Traslating research into clinical pratice. 3 ed. Filadelfia: Lipincot Williams & Wilkins; 2007. [ Links ]
20 Apóstolo, J., Cardoso, D., Marta, L. e Amaral, T. Efeito da estimulação cognitiva em Idosos. Referência. 2011; III (5):193-201. [ Links ]
21 Fortin, M. F. Fundamentos e Etapas do Processo de Investigação. 1ed. Loures: Lusodidata; 2009. ISBN: 978-972-8383-10-7. [ Links ]
22 Orientações sobre Incontinência Urinária [Internet]. Apurologia.pt. 2019 [cited 22 May 2019]. Available from: https://www.apurologia.pt/guidelines/Incont-Urinaria.pdf [ Links ]
23 Melo CA. Adaptação cultural e validação da escala "Falls Efficacy Scale" de Tinetti. Ifisionline [Internet]. 2011 [cited 22 May 2019]; 1 (3): 33-43.. [ Links ]
24 Petiz E. A atividade física, equilíbrio e quedas um estudo com idosos institucionalizados. Mestrado em Ciência do Desporto, na área de especialização de Atividade Física para a Terceira Idade, pela Faculdade de Ciências do Desporto e de Educação Física -Universidade do Porto (não publicado); 2002. [ Links ]
25 Santos AP, Ramos NC, Estevão PC, Lopes AM, Pascoalinho J. Instrumentos de medida úteis no contexto da avaliação em fisioterapia. Re (habilitar)[Internet]. 2005 [cited 22 May 2019];(1): 131-156. [ Links ]
26 Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991 Feb;39(2):142-8. [ Links ]
27 Sequeira C. Cuidar de idosos dependentes. Coimbra: Quarteto Editora; 2007. [ Links ]
28 Alves Apóstolo JL, Batista Cardoso DF, Gonçalves Marta LM, de Oliveira Amaral TI. Efeito da estimulação cognitiva em Idosos. Referência. 2011;II(5)..193-201. [ Links ]
29 Paiva DD, Apóstolo JL. Cognição e Envelhecimento: Estudo de Adaptação Transcultural e Validação do Six Item Cognitive Impairment Test (6-Cit). Escola Superior de Enfermagem de Coimbra, Coimbra. 2013. [ Links ]
30 Ferreira PL. Criação da versão portuguesa do MOS SF-36. Parte I - Adaptação cultural e linguística. Acta Med Port. 2000 Jan Abr; 13(1-2): 55-66. [ Links ]
31 Kyrdalen, Ingebjørg L. et al. The Otago Exercise Program Performed as Group Training Versus Home Training in Fall-prone Older People: A Randomized Controlled Trial. Physiother Res Int. 2013; 19(2):108-116. [ Links ]
32 Apóstolo JL, Cardoso DF, Rosa AI, Paúl C. The effect of cognitive stimulation on nursing home elders: A randomized controlled trial. J Nurs Scholarsh. 2014 May 1;46(3):157-66.. [ Links ]
33 Mulasso A, Roppolo M, Liubicich ME, Settanni M, Rabaglietti E. A multicomponent exercise program for older adults living in residential care facilities: direct and indirect effects on physical functioning. J Aging Phys Act. 2015 Jul;23(3):409-16. [ Links ]
34 Zelinski EM, Spina LM, Yaffe K, Ruff R, Kennison RF, Mahncke HW, Smith GE. Improvement in memory with plasticity-based adaptive cognitive training: Results of the 3-month follow-up. J Am Geriatr Soc. 2011 Feb;59(2):258-65.. [ Links ]
35 Gawler S, Skelton DA, Dinan-Young S, Masud T, Morris RW, Griffin M, Kendrick D, Iliffe S. Reducing falls among older people in general practice: The ProAct65+ exercise intervention trial. Arch Gerontol Geriatr. 2016 Nov 1;67:46-54. [ Links ]
36 Possamai Menezes, L., Stamm, B., Tambara Leite, M., Hildebrandt, L. e Kirchner, R. Cair faz parte da vida: Fatores de risco para quedas em idosos. Rev Pesqui Cuid Fundam. 2016; 8(4):5080 [ Links ]
37 Saúde, Direção Geral de. Hipertensão Arterial: definição e classificação. 1ed. Lisboa: DGS; 2013. [ Links ]
38 Brum, P., Forfaz, C., Tinucci, T. e Negrão, C. Adaptações agudas e crônicas do exercício físico no sistema cardiovascular. Rev Bras Educ Fís Esp. 2004; 18:21-31. [ Links ]
39 Nelson, M., Rejeski, W., Blair, S., Duncan, P. e Judge, J. Physical Activity and Public Health in Older Adults: Recommendation From the American College of Sports Medicine and the American Heart Association. Circulation. 2007; 116(9):1094-1105. [ Links ]
40 Rosqvist, E., Aukee, P., Kallinen, M. e Rantanen, T. Feasibility and acceptability of the pelvic floor muscle and bladder training programme. Int J Urol Nurs. 2008; 2(3):113-118. [ Links ]
41 Pereira, V., Correia, G. e Driusso, P. Individual and group pelvic floor muscle training versus no treatment in female stress urinary incontinence: a randomized controlled pilot study. Eur J Obstet Gynecol Reprod, 2011; 159(2):465-471. 42 Kapan A, Luger E, Haider S, Titze S, Schindler K, Lackinger C, Dorner TE. Fear of falling reduced by a lay led home-based program in frail community-dwelling older adults: A randomised controlled trial. Arch Gerontol Geriatr. 2017; 68: pp.25-32. [ Links ]
42 Kapan A, Luger E, Haider S, Titze S, Schindler K, Lackinger C, Dorner TE. Fear of falling reduced by a lay led home-based program in frail community-dwelling older adults: A randomised controlled trial. Arch Gerontol Geriatr. 2017; 68: pp.25-32. [ Links ]
43 Emilio EJ, Hita-Contreras F, Jiménez-Lara PM, Latorre-Román P, Martínez-Amat A. The association of flexibility, balance, and lumbar strength with balance ability: risk of falls in older adults. J Sports Sci Med. 2014 May;13(2):349-357. [ Links ]
44 Jahana KO, Diogo MJ. Quedas em idosos: principais causas e conseqüências. Saúde Colet. 2007; 4(17):148-153. [ Links ]
45 Fhon JR, Fabrício-Wehbe SC, Vendruscolo TR, Stackfleth R, Marques S, Rodrigues RA. Accidental fails in the elderly and their relation with functional capacity. Rev Latino-Am Enferm. 2012; 20(5):1-8. [ Links ]
46 Yardimci, B., Aran, S., Ozkaya, I., Aksoy, S., Demir, T., Tezcan, G. e Kaptanoglu, A. The role of geriatric assessment tests and anthropometric measurements in identifying the risk of falls in elderly nursing home residents. Saudi Med J. 2016; 37(10):1101-1108. [ Links ]
47 Guzman AB, Lacampuenga PE, Lagunsad AP. Examining the structural relationship of physical activity, cognition, fear of falling, and mobility limitation of Filipino in nursing homes. Educ Gerontol. 2015; 41(7):527-542. [ Links ]
48 Riva N, Faccendini S, Lopez ID, Fratelli A, Velardo D, Quattrini A, et al. Balance exercise in patients with chronic sensory ataxic neuropathy: a pilot study. Journal of the Peripheral Nervous System. 2014; 19:145-151. [ Links ]
49 Berlezi EM, Martins M, Dreher DZ. Programa individualizado de exercícios para incontinência urinária executado no espaço domiciliar. Sci Med. 2013 Oct 1;23(4),232-238. [ Links ]
Received: January 31, 2019; Accepted: June 25, 2019











 texto em
texto em