Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Portuguesa de Enfermagem de Reabilitação
Print version ISSN 2184-965XOn-line version ISSN 2184-3023
RPER vol.2 no.1 Silvalde June 2019
https://doi.org/10.33194/rper.2019.v2.n1.06.4558
Articles
FUNCTIONALITY OF PEOPLE SUBMITTED TO TOTAL SHOULDER ARTHROPLASTY BY PROXIMAL HUMERUS FRACTURES: RETROSPECTIVE STUDY
1- Unidade Local de Saúde do Nordeste
2- Escola Superior de Saúde do Instituto Politécnico de Bragança; NurseID - CINTESIS
Objective:
To retrospectively identify, in people submitted to total shoulder arthroplasty for proximal humeral fractures, the type of arthroplasty used, the functional shoulder scores, the recorded complications, the influence of the elapsed time from the fracture and the placement of the implant in the final functional outcome.
Method:
Retrospective study between 2014 and 2017. The following variables were identified: age, sex, time between fracture and surgery, type of arthroplasty, cementation, modularity, rehabilitation, complications, follow-up time and functionality. Data from the scales Constant Shoulder Score and American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form were obtained.
Results:
Sample comprised of 12 women and 3 men with mean age of 78 years-old and a mean time between fracture and surgery of 29.4 days. In terms of functionality, it was observed that people with inverse prosthesis presented better results compared to the ones submitted to hemiarthroplasty (53.2 vs. 41.1 and 68.5 vs. 44.6). The follow-up duration was 29.4 months.
Conclusion:
The reverse prosthesis seems to be the best treatment option and allows better functionality. Prosthetic modularity is important.
Keywords: Humeral fractures; Surgical Procedures; Orthopedic Procedures; Total shoulder replacement; Rehabilitation
Objetivo:
Identificar retrospetivamente, em pessoas submetidas a artroplastia total do ombro por fraturas do úmero proximal, o tipo de artroplastia utilizado, os scores funcionais do ombro, as complicações registadas, a influência do tempo decorrido desde a fratura e a colocação do implante no resultado funcional final.
Método:
Estudo retrospetivo entre os anos 2014 e 2017. Foram identificadas as seguintes variáveis: idade, sexo, tempo entre a fratura e a cirurgia, tipo de artroplastia, cimentação, modularidade, reabilitação, complicações, tempo de seguimento e funcionalidade. Foram recolhidos dados dos instrumentos Constant Shoulder Score e American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form.
Resultados:
Amostra constituída por 12 mulheres e 3 homens com idade média de 78 anos e um tempo médio entre a fratura e a cirurgia de 29,4 dias. A nível de funcionalidade observou-se que as pessoas com próteses inversas apresentaram melhores resultados em comparação com as submetidas a hemiartroplastia (53,2 vs. 41,1 e 68,5 vs. 44,6). O seguimento foi feito durante foi de 29,4 meses.
Conclusão:
A escolha de prótese inversa parece ser a melhor opção de tratamento e que permite melhor funcionalidade. A modularidade protésica é importante.
Descritores: Fraturas do úmero; Intervenção Cirúrgica; Procedimentos Ortopédicos; Artroplastia do ombro; Reabilitação
Objetivo:
Identificar retrospectivamente, en personas sometidas a artroplastia total del hombro por fracturas del húmero proximal, el tipo de artroplastia utilizado, la puntuación funcional del hombro, las complicaciones registradas, la influencia del tiempo transcurrido desde la fractura y la colocación del implante en el resultado funcional final.
Método:
estudio retrospectivo entre 2014 y 2017. Se identificaron las siguientes variables: edad, sexo, tiempo entre fractura y cirugía, tipo de artroplastia, cementación, modularidad, rehabilitación, complicaciones, tiempo de seguimiento y funcionalidad. Fueron recogidos datos de los instrumentos Constant Shoulder Score y American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form.
Resultados:
Muestra compuesta por 12 mujeres y 3 hombres con una edad media de 78 años y un tiempo medio entre la fractura y la cirugía de 29,4 días. En términos de funcionalidad, se observó que las personas con próstesis inversa presentaran mejores resultados en comparación con las sometidas a hemiartroplastia (53,2 vs. 41,1 y 68,5 vs. 44,6). El seguimiento se realizó durante 29,4 meses.
Conclusión:
La prótesis inversa parece ser la mejor opción de tratamiento y que permite una mejor funcionalidad. La modularidad protésica es importante.
Descriptores: Fracturas humerales; Procedimientos quirúrgicos; Procedimientos ortopédicos; Artroplastia total del hombro; Rehabilitación
INTRODUCTION
Fractures of the proximal humerus (FPH) are the third most frequent fractures; only surpassed by hip and distal radius fractures1. They have an incidence of 4-6%, affecting more women than man. They mostly occur due to low-energy trauma and in the elderly people2.
The type of treatment to be instituted depends on factors such as the patient's age, functional demand, dominance, comorbidities, type of fracture and its classification3.
Although most FPH are treated conservatively, it is estimated that up to 20% of them require surgical treatment. Due to the population aging, the number of FPH can increase and consequently the percentage that need a surgical intervention as well4.
The FDP treatments of 3 or 4 parts Neer is a challenge. Initially, hemiarthroplasty (HA) was recommended as the ideal treatment, due to the difficulty of closed reduction and the risk of avascular necrosis of the humeral head5. It was also recommended for fractures with a “head-split” component6.
However, complex FPH that affect the tuberosities are technically demanding to treat and their poor positioning is correlated with worse functional results, if the option is HA7.
Currently, inverse total shoulder arthroplasty (ITSA) has been shown to be effective in the treatment of 3 or 4 parts Neer’s fractures in elderly patients with rotator cuff arthropathy8-11, with good functional results12-14, and the latter depend less on the positioning of the tuberosities than on HA15.
The progressive increase in the number of these cases treated with arthroplasties can lead to long-term complications that require a surgeon with technical skills to resolve them. Revision surgery for an HA or ITSA also leads to less predictable functional results and higher complication rates16-18.
Among the complications described, aseptic or septic unsealing, instability, wear of the glenoid component and incompetence/rupture of the rotator cuffs are highlighted19-21.
The development of modular implants allows for greater ease in revision surgeries, with the possibility of preserving the humeral component and converting from an HA to an ITSA22. The time elapsed between the fracture and the surgery is considered a factor that affects the final result in HA.
This study aims to retrospectively identify, in people undergoing total shoulder arthroplasty for fractures of the proximal humerus, the type of arthroplasty used, the functional scores of the shoulder, the complications recorded, the influence of the time elapsed since the fracture and the placement of the implant in the final functional result.
METHOD
Retrospective consultation study of clinical files in which patients undergoing HA and ITSA due to FPH were included, in the period from January 1, 2014 to March 31, 2017, in an Orthopedics and Traumatology Service.
Electronic clinical files were consulted, and demographic characteristics (age and gender), type of FPH (Neer classification), time elapsed between fracture diagnosis and initial surgery for HA or ITSA, need for cementation and prosthetic modularity were recorded, need for revision, complications, follow-up time and participation in a regular rehabilitation program.
The functional results of each patient were collected from two previously applied instruments:
- Constant Shoulder Score (CSS)23, adapted for Portugal24, is a 100-point scale that is divided into four subscales - pain, activities of daily living, strength and joint range of motion.
- American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES)25, Portuguese version25, being divided into two sections, one clinical and one self-administered. This second section presents a 100-point scale consisting of two dimensions, a pain subscale worth 50 points, and ten daily life activities items worth the remaining 50 points.
Ethical and deontological procedures were complied with and the best interests of patients, namely their anonymity were safeguarded.
Descriptive and inferential statistical analysis of the data was performed using the IBM SPSS statistics software, version 23. The results are presented in absolute value and as a percentage when it is justified to facilitate their interpretation. Mean values are shown followed by the standard deviation (mean±standard deviation). For the inferential analysis, the non-parametric Mann-Whitney U test was used to compare the groups operated early and late and the groups submitted to HA vs. ITSA. The assumed p value for this study was p ≤ 0.05.
RESULTS
During the time covered by our study, 15 shoulder arthroplasties were performed by FPH in 12 women and 3 men. The mean age of the sample was 78 years-old. (Table 1)
We recorded 6 Neer 2-part FPH cases, 2 Neer 3-part FPH cases and 7 Neer 4-part FPH cases. (Table 1)
The average time between fracture diagnosis and surgery was 29.4 days (Table 1), with 9 of the patients undergoing early surgery (up to 3 weeks after diagnosis). We registered 6 cases of late surgery (3 weeks after diagnosis).
10 ITSA were performed, with the particularity of 3 of them as salvage treatment of failure of conservative treatment (two cases of 2-part Neer FPH and one 3-part Neer FPH) and 2 of them as rescue treatment of initial treatment failure with osteosynthesis (both FPH 2 parts of Neer). 5 HA were recorded. (Table 2)
All procedures were performed by the same surgeon.
Except for 2 cases of ITSA, all implants were cemented and all placed prostheses were modular. (Table 2)
Table 1: Demographic data of the sample: gender (F-female; M-male) and age; follow-up time; fracture classification (Neer classification).
| Gender | Age (years) | Follow-up time (days) | Fracture type (Neer) | |||||
|---|---|---|---|---|---|---|---|---|
| F | M | Min | Max | Average±DP | Average±DP | 2-parts | 3-parts | 4-parts |
| 12 | 3 | 89 | 63 | 77.60±7.76 | 29.40±48.04 | 6 (40%) | 2 (13.3%) | 7 (46.7%) |
Table 2: Type of arthroplasty used (ITSA - inverse total shoulder arthroplasty; HA - hemiarthroplasty); Cementation of arthroplasties; Modularity.
| Type of arthroplasty | Cementation | Modularity | ||
|---|---|---|---|---|
| ITSA | HA | Uncemented | Cemented | |
| 10 (5 rescue; 3 conservative treatment failures; 2 osteosynthesis failures) | 5 | 2 (ATIO) | 13 | 15 |
Table 3: Functional scores (CSS - Constant Shoulder Scores; ASES - American Shoulder and Elbow Score) for the type of arthroplasty used (ITSA -Inverse Total Shoulder Arthroplasty; HA - hemiarthroplasty); Registered complications.
| Functional Scores | Complications | |||||
|---|---|---|---|---|---|---|
| CSS(%) | ASES | Infection | Stem migration | “Impingement” subacromial | ||
| HA | ATRO | HA | ATRO | 1 (ATRO) | 1 (HA) | 1 (HA) |
| 53.2 | 41.1 | 44.6 | 68.5 | |||
Regarding the functionality of the groups, for the group of patients undergoing HA, the mean score was 53.2% and 44.6, respectively for CSS and ASES; in the group of patients undergoing ITSA, the mean scores were 41.1% and 68.5, respectively for CSS and ASES (Table 3).
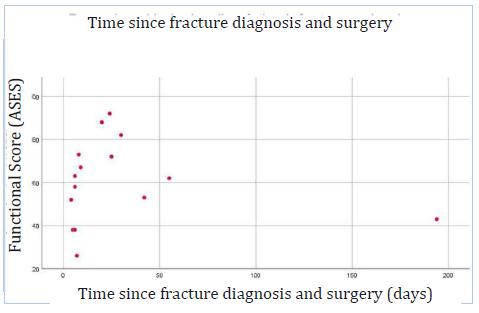
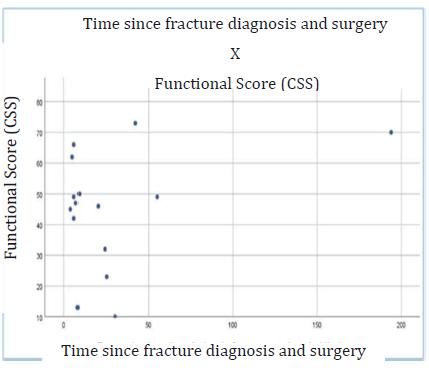
Results with statistical significance were not obtained in the comparative study of the mean values of CSS and ASES between the groups which underwent early and late surgeries (Graphics 1 and 2).
In the comparative study of functional scores between patients undergoing HA and ITSA, there was a statistically significant value (p<0.05) for ASES of patients with ITSA (Graphic 2).
The complications that were recorded were divided into a case of acute infection of an ITSA, a case of proximal migration of the HA’s nail requiring revision (with conversion to ITSA), a case of sub-acromial impingement of an HA (Table 3) needing revision with
conversion into arthroscopic shoulder surgery for treatment of rotator cuff tear (ATRO). In revision surgeries, no complications were recorded.
Graphic 1 Relation between the time since fracture diagnosis and surgery and the CSS (Constant Shoulder Score) functional score
DISCUSSION
Generally speaking, most FPH can be treated conservatively. On the other hand, FPH with surgery indication are typical of the elderly who, due to osteoporosis inherent to their age, increase the complexity of these fractures16,26,27. In fact, a study recently published by Jung et al.28 reported a rate of refraction of more than 18% in elderly people with osteoporosis. The mean age of patients treated in the present study was 78 years-old, which reflects the aging population of the geographic covered area and which is corroborated by several review articles published since 201529-32.
The currently increasing literature recommends ITSA as a first-line treatment in complex FPH in the elderly people with surgical criteria, when osteosynthesis is not indicated8-11. ITSA is also increasingly recommended as a rescue treatment when primary treatments have failed19-21, recognizing the importance of prosthetic modularity for revision surgeries22.
The complications recorded were those foreseen in any shoulder arthroplasty, however complications of vascular-nervous involvement were not recorded16.
In the comparative study of functional outcomes in patients undergoing HA versus ITSA, the best score was recorded for ITSA, but only with statistical significance for the ASES score (p<0.05). These data are in agreement with the literature, which states that ITSA allows better functional results when compared to HA8-11. The results obtained by the ASES assessment are in line with the results found by other studies, namely 64.14 points described in the work published by Horneff et al.33, 66 points in the work developed by Wagner et al.34, 59 points in the article published in 2017 Holschen et al. and 65.3 points in another article published by the same team35,36. Regarding the CSS assessment, the results found range from 57 to 45% in the study developed by Lignel et al.37, 63% in the article published by Holschen et al., 52.9% in the publication by Giardella et al.38 to 73% in the study carried out by Schliemann et al.39. The present study was not able to assess the influence of the time interval from FPH diagnosis to surgery on functional outcomes. The comparative study of functional scores between early and late operated patients was not statistically significant (p>0.05). The fact that the sample in this study was relatively small and that 5 of the cases were implants performed as rescue treatment may have negatively influenced this comparative study.
CONCLUSION
The present study concludes that FPH with surgical criteria are typical of an aging population with poor bone stock.
For complex FPH and in the elderly without criteria for osteosynthesis, this study concludes that ITSA seems to be the best option as a first-line treatment in FPH with surgical criteria and it allows the patient to have better postoperative functionality, with regard to the ASES score.
It can also be concluded that prosthetic modularity is an asset in revision surgeries, making this procedure intrinsically more demanding, safer and simpler.
Therefore, despite a short experience and a small sample of cases, we can deduce that there are good practices regarding the treatment offered and that the most current international recommendations are followed.
In terms of the limitations of the present study, the small sample size, the relatively short follow-up time, the different contexts and experiences of the rehabilitation team and the type of prosthesis used, which was not homogeneous, can be indicated.
For the future, it is suggested to extend the follow-up time, create a specific intervention and rehabilitation team and improve the implant model.
REFERÊNCIAS
1 Baron JA, Barrett JA, Karagas MR. The epidemiology of peripheral fractures. Bone. 1996 Mar;18(3 Suppl):209S-213S. [ Links ]
2 Court-Brown CM, Garg A, McQueen MM. The translated two-part fracture of the proximal humerus. Epidemiology and outcome in the older patient. J Bone Joint Surg Br. 2001 Aug;83(6):799-804. Available from: https://doi.org/10.1016/j.otsr.2008.09.002 [ Links ]
3 Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970 Sep;52(6):1077-89. [ Links ]
4 Hanson B, Neidenbach P, de Boer P, Stengel D. Functional outcomes after nonoperative management of fractures of the proximal humerus. J Shoulder Elb Surg. 2009 Jul;18(4):612-21. Available from: https://doi.org/10.1016/j.jse.2009.03.024 [ Links ]
5 Neer CS. Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am. 1970 Sep;52(6):1090-103. [ Links ]
6 Greiwe RM, Vargas-Ariza R, Bigliani LU, Levine WN, Ahmad CS. Hemiarthroplasty for head-split fractures of the proximal humerus. Orthopedics. 2013 Jul;36(7):e905-11. Available from: https://doi.org/10.3928/01477447-20130624-21 [ Links ]
7 Kralinger F, Schwaiger R, Wambacher M, Farrell E, Menth-Chiari W, Lajtai G, et al. Outcome after primary hemiarthroplasty for fracture of the head of the humerus. A retrospective multicentre study of 167 patients. J Bone Joint Surg Br. 2004 Mar;86(2):217-9. [ Links ]
8 Chambers L, Dines JS, Lorich DG, Dines DM. Hemiarthroplasty for proximal humerus fractures. Curr Rev Musculoskelet Med. 2013 Mar;6(1):57-62. Available from: https://doi.org/10.1007/s12178-012-9152-9 [ Links ]
9 Gallinet D, Clappaz P, Garbuio P, Tropet Y, Obert L. Three or four parts complex proximal humerus fractures: hemiarthroplasty versus reverse prosthesis: a comparative study of 40 cases. Orthop Traumatol Surg Res. 2009 Feb;95(1):48-55. Available from:https://doi.org/10.1016/j.otsr.2008.09.002 [ Links ]
10 Cuff D, Clark R, Pupello D, Frankle M. Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency: a concise follow-up, at a minimum of five years, of a previous report. J Bone Joint Surg Am. 2012 Nov 7;94(21):1996-2000. Available from:https://doi.org/10.2106/JBJS.K.01206 [ Links ]
11 Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006 Aug;88(8):1742-7. Available from: https://doi.org/10.2106/JBJS.E.00851 [ Links ]
12 Singhal K, Rammohan R. Going forward with reverse shoulder arthroplasty. J Clin Orthop Trauma. 2018 Jan;9(1):87-93. Available from: https://doi.org/10.1016/j.jcot.2017.10.002 [ Links ]
13 van der Merwe M, Boyle MJ, Frampton CMA, Ball CM. Reverse shoulder arthroplasty compared with hemiarthroplasty in the treatment of acute proximal humeral fractures. J shoulder Elb Surg. 2017 Sep;26(9):1539-45. Available from: https://doi.org/10.1016/j.jse.2017.02.005 [ Links ]
14 Frombach AA, Brett K, Lapner P. Humeral Head Replacement and Reverse Shoulder Arthroplasty for the Treatment of Proximal Humerus Fracturesm. Open Orthop J. 2017;11:1108-14. Available from: https://doi.org/10.2174/1874325001711011108 [ Links ]
15 Reuther F, Petermann M, Stangl R. Reverse Shoulder Arthroplasty in Acute Fractures of the Proximal Humerus: Does Tuberosity Healing Improve Clinical Outcomes? J Orthop Trauma. 2019 Feb;33(2):e46-51. Available from: https://doi.org/10.1097/BOT.0000000000001338 [ Links ]
16 Stone MA, Namdari S. Surgical Considerations in the Treatment of Osteoporotic Proximal Humerus Fractures. Orthop Clin North Am. 2019 Apr;50(2):223-31. Available from: https://doi.org/10.1016/j.ocl.2018.10.005 [ Links ]
17 Chalmers PN, Boileau P, Romeo AA, Tashjian RZ. Revision Reverse Shoulder Arthroplasty. J Am Acad Orthop Surg. 2019 Jun 15;27(12):426-36. Available from: https://doi.org/10.5435/JAAOS-D-17-00535 [ Links ]
18 Boileau P. Complications and revision of reverse total shoulder arthroplasty. Orthop Traumatol Surg Res. 2016 Feb;102(1 Suppl):S33-43. Available from: https://doi.org/10.1016/j.otsr.2015.06.031 [ Links ]
19 Besch L, Daniels-Wredenhagen M, Mueller M, Varoga D, Hilgert R-E, Seekamp A. Hemiarthroplasty of the shoulder after four-part fracture of the humeral head: a long-term analysis of 34 cases. J Trauma. 2009 Jan;66(1):211-4. Available from: https://doi.org/10.1097/TA.0b013e31815d9649 [ Links ]
20 Cadet ER, Ahmad CS. Hemiarthroplasty for three- and four-part proximal humerus fractures. J Am Acad Orthop Surg. 2012 Jan;20(1):17-27. Available from: https://doi.org/10.5435/JAAOS-20-01-017 [ Links ]
21 Robinson CM, Page RS, Hill RMF, Sanders DL, Court-Brown CM, Wakefield AE. Primary hemiarthroplasty for treatment of proximal humeral fractures. J Bone Joint Surg Am. 2003 Jul;85(7):1215-23. Available from: https://doi.org/10.2106/00004623-200307000-00006 [ Links ]
22 Flury MP, Frey P, Goldhahn J, Schwyzer H-K, Simmen BR. Reverse shoulder arthroplasty as a salvage procedure for failed conventional shoulder replacement due to cuff failure--midterm results. Int Orthop. 2011 Jan;35(1):53-60. Available from:https://doi.org/10.1007/s00264-010-0990-z [ Links ]
23 Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987 Jan;(214):160-4. [ Links ]
24 Leal SM, Cavalheiro L. Constant Score e Shoulder Pain and Disability Index (SPADI)-Adaptação cultural e linguística. Monogr Coimbra Esc Super Tecnol da Saúde Coimbra. 2001; [ Links ]
25 Ruivo RM, Pezarat-Correia P, Carita AI. Versão Portuguesa do American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES). Rev Port Ortop e Traumatol. 2015;23(4):288-97. [ Links ]
26 Ratajczak K, Szczesny G, Maldyk P. Comminuted fractures of the proximal humerus - principles of the diagnosis, treatment and rehabilitation. Ortop Traumatol Rehabil. 2019 Apr 30;21(2):71-86. Available from: https://doi.org/10.5604/01.3001.0013.1544 [ Links ]
27 Misra S, Vaishya R, Trikha V, Maheshwari J. Practice guidelines for proximal humeral fractures. J Clin Orthop Trauma. 2019 May;10(3):631-3. Available from: https://doi.org/10.1016/j.jcot.2019.04.005 [ Links ]
28 Jung H-S, Nho J-H, Ha Y-C, Jang S, Kim H-Y, Yoo J-I, et al. Incidence of Osteoporotic Refractures Following Proximal Humerus Fractures in Adults Aged 50 Years and Older in Korea. J bone Metab. 2019 May;26(2):105-11. Available from:https://doi.org/10.11005/jbm.2019.26.2.105 [ Links ]
29 Schumaier A, Grawe B. Proximal Humerus Fractures: Evaluation and Management in the Elderly Patient. Geriatr Orthop Surg Rehabil. 2018 Jan 25;9:215145851775051. Available from: https://doi.org/10.1177/2151458517750516 [ Links ]
30 Longo UG, Petrillo S, Berton A, Denaro V. Reverse total shoulder arthroplasty for the management of fractures of the proximal humerus: a systematic review. Musculoskelet Surg. 2016 Aug;100(2):83-91. Available from: https://doi.org/10.1007/s12306-016-0409-0 [ Links ]
31 Xie L, Ding F, Zhao Z, Chen Y, Xing D. Operative versus non-operative treatment in complex proximal humeral fractures: a meta-analysis of randomized controlled trials. Springerplus. 2015;4:728. Available from: https://doi.org/10.1186/s40064-015-1522-5 [ Links ]
32 Slobogean GP, Johal H, Lefaivre KA, MacIntyre NJ, Sprague S, Scott T, et al. A scoping review of the proximal humerus fracture literature. BMC Musculoskelet Disord. 2015 May 10;16:112. Available from: https://doi.org/10.1186/s12891-015-0564-8 [ Links ]
33 Horneff JG, Nicholson TA, Namdari S, Williams GR, Abboud JA. The Midterm Results of the Delta Xtend Reverse Shoulder System: A Five-Year Outcome Study. Arch bone Jt Surg. 2018 Nov;6(6):532-8. [ Links ]
34 Wagner ER, Hevesi M, Houdek MT, Cofield RH, Sperling JW, Sanchez-Sotelo J. Can a reverse shoulder arthroplasty be used to revise a failed primary reverse shoulder arthroplasty? Bone Joint J. 2018 Nov;100-B(11):1493-8. Available from:https://doi.org/10.1302/0301-620X.100B11.BJJ-2018-0226.R2 [ Links ]
35 Holschen M, Franetzki B, Witt K-A, Liem D, Steinbeck J. Is reverse total shoulder arthroplasty a feasible treatment option for failed shoulder arthroplasty? A retrospective study of 44 cases with special regards to stemless and stemmed primary implants. Musculoskelet Surg. 2017 Aug;101(2):173-80. Available from: https://doi.org/10.1007/s12306-017-0467-y [ Links ]
36 Holschen M, Siemes M-K, Witt K-A, Steinbeck J. Five-year outcome after conversion of a hemiarthroplasty when used for the treatment of a proximal humeral fracture to a reverse total shoulder arthroplasty. Bone Joint J. 2018 Aug 1;100-B(6):761-6. Available from:https://doi.org/10.1302/0301-620X.100B6.BJJ-2017-1280.R1 [ Links ]
37 Lignel A, Berhouet J, Loirat M-A, Collin P, Thomazeau H, Gallinet D, et al. Reverse shoulder arthroplasty for proximal humerus fractures: Is the glenoid implant problematic? Orthop Traumatol Surg Res. 2018 Oct;104(6):773-7. [ Links ]
38 Giardella A, Ascione F, Mocchi M, Berlusconi M, Romano AM, Oliva F, et al. Reverse total shoulder versus angular stable plate treatment for proximal humeral fractures in over 65 years old patients. Muscles Ligaments Tendons J. 7(2):271-8. [ Links ]
39 Schliemann B, Theisen C, Kösters C, Raschke MJ, Weimann A. Reverse total shoulder arthroplasty for type I fracture sequelae after internal fixation of proximal humerus fractures. Arch Orthop Trauma Surg. 2017 Dec;137(12):1677-83. [ Links ]
Received: February 21, 2019; Accepted: June 27, 2019











 text in
text in