Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Portuguesa de Enfermagem de Reabilitação
Print version ISSN 2184-965XOn-line version ISSN 2184-3023
RPER vol.1 no.2 Silvalde Dec. 2018
https://doi.org/10.33194/rper.2018.v1.n2.02.4404
Articles
International Classification Of Functioning, Disability And Health For Stroke
2- USF Vista Tejo, Monte da Caparica
3- Hospital Egas Moniz, Centro Hospitalar Lisboa Ocidental
4- Hospital de São Francisco Xavier, Centro Hospitalar Lisboa Ocidental
5- Escola Superior de Saúde Atlântica
6- Hospital Curry Cabral, Centro Hospitalar Universitário Lisboa Central
Background:
Stroke is a cardiovascular disease with the highest prevalence worldwide, with impact on the functionality of survivors.
Objective:
To identify the Score Set of the International Classification of Functioning, Disability and Health (ICF) for people after stroke.
Material and Methods:
The research question was performed according to the Joanna Briges Institute (JBI) recommendations and PICo framework (Population, Interest phenomenon, Context). Each dimension of the PICo contributed to the definition of inclusion criteria, namely Population (P) Person after stroke; Interest phenomenon (I) Score set ICF; Context (Co) Community. The electronic research was done in the Medline, SciELO, virtual health library and EBSCO databases, between 2013 and 2017.
Results:
Out of the identified articles 11 were selected and 160 ICF codes were identified, which characterize the functionality of people after stroke. Of these 160 codes, it was verified that 21, divided by 3 ICF categories, presented a frequency greater than or equal to 50%.
Conclusions:
The ICF score set for people after stroke is distributed as follows: 6 Body Functions (29%), 13 Activity and Participation (61%) and 2 Environmental Factors (10%).
Keywords: International Classification of Functioning; Disability and Health; Stroke; Rehabilitation Nursing
Contexto:
O Acidente Vascular Cerebral (AVC) é uma das doenças com maior prevalência a nível mundial, com impacto na funcionalidade das pessoas sobreviventes.
Objetivo:
identificar o Score Set da Classificação Internacional de Funcionalidade, Incapacidade e Saúde (CIF) para pessoas após AVC.
Material e Métodos:
A pergunta de investigação, foi elaborada segundo as recomendações do Joanna Briges Institute (JBI) a partir da estratégia PICo (Population, Interest phenomenon, Context). Cada dimensão do PICo contribuiu para a definição de critérios de inclusão, nomeadamente Population (P) Pessoa após AVC; Interest phenomenon (I) Score set CIF; Context (Co) Comunidade. A pesquisa eletrónica foi feita nas bases de dados Medline, SciELO, biblioteca virtual em saúde e EBSCO, de publicações entre 2013 a 2017.
Resultados:
Dos artigos identificados, foram selecionados 11, tendo sido identificados 160 códigos da CIF, que caraterizam a funcionalidade das pessoas após AVC. Destes 160 códigos, verificou-se que 21, divididos por 3 categorias CIF, apresentam uma frequência maior ou igual a 50%.
Conclusões:
O score set da CIF para pessoas após AVC está distribuído da seguinte forma: 6 códigos das Funções do Corpo (29%), 13 códigos das Atividades e Participação (61%) e 2 códigos dos Fatores Ambientais (10%).
Descritores: Classificação Internacional de Funcionalidade; Incapacidade e Saúde; Acidente Vascular Cerebral; Enfermagem de Reabilitação
Contexto:
el Accidente Vascular Cerebral (AVC) es una enfermedad cardiovascular con mayor prevalencia a nivel mundial, con impacto en la funcionalidad de las personas sobrevivientes.
Objetivo:
identificar el Score Set de la Clasificación Internacional de Funcionalidad, Incapacidad y Salud (CIF) para personas después del AVC.
Material y Métodos:
la pregunta de investigación, fue elaborada según las recomendaciones del Joanna Briges Institute (JBI) a partir de la estrategia PICo (Population, Interés, Context). Cada dimensión del PICo contribuyó a la definición de criterios de inclusión, en particular Population (P) Persona después de AVC; (I) Score set CIF; Context (Co) Comunidad. La pesquisa electrónica se realizó en las bases de datos Medline, SciELO, Biblioteca Virtual em Saúde y EBSCO, de publicaciones entre 2013 a 2017.
Resultados:
De los artículos identificados,han sido seleccionados 11 artículos donde fueron identificados 160 códigos de la CIF, que caracterizan la funcionalidad de las personas después del AVC. De estos 160 códigos, se verificó que 21 están divididos por 3 categorías CIF, presentan una frecuencia mayor o igual al 50%..
Conclusiones: El score set de la CIF para personas después de AVC está distribuido de la siguiente forma: 6 códigos de las Funciones del Cuerpo (29%), 13 códigos de las Actividades y Participación (61%) y 2 códigos de los Factores Ambientales (10%).
Descriptores: Clasificación Internacional del Funcionamiento; de la Discapacidad y de la Salud; Accidente Cerebrovascular; Enfermería en Rehabilitación
INTRODUTION
Cerebrovascular accident (CVA) can be defined as a cardiovascular disease caused by the interruption of the blood supply to the brain, with a decrease or absence of oxygen and nutrients supply, causing damage to the brain tissue.1
Stroke has a high worldwide prevalence.2 This pathology is the second leading cause of death worldwide, accounting for approximately 5.7 million deaths, equivalent to 9.9% of all deaths.1
The incidence of stroke, adjusted to the World Health Organization (WHO) standard world population, ranged from 76 per 100,000 population per year in Australia (2009-10) to 119 per 100,000 population per year in New Zealand (2011-12).3 The incidence of stroke has increased worldwide, in both men and women of all ages.4
At the beginning of the 21st century, the age-standardized incidence of stroke in Europe ranged from 95 to 290/100,000 per year, with monthly mortality rates ranging from 13 to 35%.5
In Portugal, between 1990 and 2012, there was an increase in the incidence rate of stroke from 265.1/105 to 343.7/105.6
In 2015, there were 11,778 deaths in Portugal due to cerebrovascular diseases. By gender, there were 5057 deaths of men and 6,721 of women.7
In addition to the high mortality rate, this clinical condition is assumed to be one of the main causes of morbidity, with high social and economic burdens, since only 10% of stroke survivors recover almost entirely, 25% recover with minimal sequelae, 40% are left with moderate to severe disability, requiring specialized care, 10% need long-term care requiring institutionalization, and 15% die after stroke.8 In this perspective, the person after a stroke, it has some altered functions, with implications for activity and participation and consequently for its functionality, namely with regard to basic, instrumental and social activities of daily living. The ICF presents a conceptual framework that allows analyzing the person's functionality under these conditions.
The ICF resulted from the revision of the previous International Classification of Impairments, Disabilities and Handicaps (ICIDH), experimental version published in 1980 by WHO. In 2001, WHO proposed an update to the old model, creating the ICF.9 This new model has the general objective of providing a unified and standardized language as well as a framework for the description of health and health-related conditions. The ICF includes all aspects of human health and some health-relevant components related to well-being and describes them in terms of health domains and health-related domains. These domains describe changes in physiological functions and body structures, describing the ability of a person with a certain health condition to influence their environment and performance.9
This is a very extensive classification, which may be one of the reasons for its little use in clinical practice, so WHO and its collaborators have developed smaller code lists called Score Sets. Score Sets arise from several processes, which require several steps and are still in the process of development and study, with the aim of facilitating its applicability in clinical practice, in research and service management.10-11
In this way, it is intended to speed up the assessment of the person with stroke, since, instead of evaluating all aspects of their functionality; the most significant categories for them are evaluated. The selection of codes for the elaboration of the Score set based on the ICF will serve as a minimum standard for the assessment and documentation of functionality and health in clinical studies, clinical meetings and comprehensive multiprofessional assessment.11
The Stroke Score Set theme based on the ICF was chosen because of its current prevalence, which gives it special importance in the field of rehabilitation nursing. Thus, this study aims to identify the most appropriate Score Set based on the ICF for assessing functionality and health-related aspects of stroke patients.
METHOD
It was decided to carry out a SLR, as it is intended to answer a clearly formulated question using systematic and explicit methods to identify, select and critically evaluate relevant research and collect and analyze data from studies included in the review.12 With this methodology, the strategies used reduce biases in the selection of articles and, based on a well-defined question, synthesize the results of primary studies in a given area.13
For an analysis of all the available evidence and, in order to understand if a practice is effective or not, it is necessary to follow several steps: 1. Elaboration of the research question; 2. Literature search; 3. Selection of articles; 4. Data extraction; 5. Assessment of methodological quality; 6. Data synthesis; 7. Assessment of the quality of evidence; and 8. Writing and publication of results.14
The research question was elaborated according to the recommendations of the Joanna Briges Institute (JBI)15 from the PICo16 strategy (Population, Interest phenomenon, Context). Each dimension of the PICo contributed to the definition of inclusion criteria, namely Population (P) Person with stroke; Interest phenomenon (I) ICF Score set; Context (Co) Community. What is the most suitable ICF-based Score Set for the person with stroke in the community?
As a form of exclusion from the studies, the criteria used were, language other than English, Spanish, Portuguese, studies referring to children that are not provided in full texts, studies that do not address the topic of ICF in people with stroke and, finally, articles that present quality criteria below 75%, in the JBI grids.15
The research was carried out from October 19th to November 19th, 2017, in the Medline, SciELO, virtual health library, EBSCO, Nurses Order and General Directorate of Health databases, including articles and books published between 2013 and 2017.
The descriptors were validated in the platforms, Health Sciences Descriptors (DeSC) and Medical Subject Headings 2017 (MeSH), using a Boolean equation in the research, (International Classification of Functioning, Disability and Health) OR (ICF)) AND (Stroke).
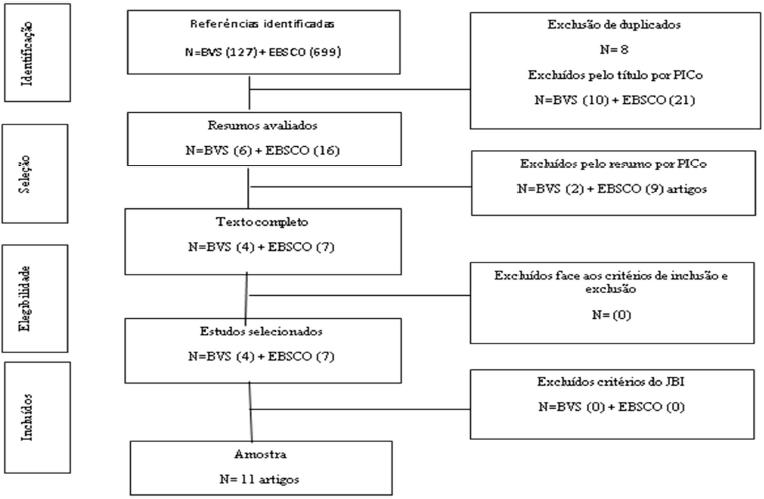
After outlining the strategy, research and selection of articles were carried out according to the indications of the PRISMA recommendations 17 (Figure I).
The results were obtained by reading the title, after the abstract and later, the full text. For greater credibility of the study, the results were compared and the agreement between the researchers was verified.
RESULTS
Out of the 11 articles analyzed, three were published in 2013,18-20 three in 2014,21-23 three in 2015,24-26, one in 201610 and one in 201727.
As far as countries of origin Brazil,18,20,27 USA,21 Sweden,19,22 Spain,24 Germany 26 China 10,23 and Finland25 were included.
The samples used in the analyzed studies ranged between 1218 and 22710 persons diagnosed with stroke.
The studies analyzed are descriptive quantitative studies10,19,20-21,23-27 and qualitative studies,19,22 with level of evidence III.
After analyzing the different articles, their objectives, their level of evidence were identified and the ICF codes mentioned in each article were grouped (Chart 1).
Table 1 Systematiztionof the information required by the article
| Author/ Year/Country | Population(Sample) | Objectives | NE | Category Codes CIF |
|---|---|---|---|---|
| Campos et al. (2013), Brazil18 | 12 persons with stroke | To compare the instruments for the assessment of sleep, cognition and function with the ICF in people with stroke | III | Body functions - b110, b114, b117, b134, b140, b144, b156, b164, b167, b176, b180, b210, b310, b320, b510, b525, b620, b710, b730, b760, b770 Activity and Participation d115, d160, d166, d170, d172, d175, d210, d230, d310, d345, d410, d420, d430, d440, d445, d450, d455, d465, d510, d520, d530, d540, d550, d570 |
| Paanalahti, et al. (2013), Sweden19 | 22 persons with a previous diagnosis of stroke . | To apply and to understand the ICF code to persons, living in a community, who have survived stroke. | III | Body functions - b110, b126, b130, b134, b140, b144, b152, b164, b167, b210, b215, b260, b265, b270, b280, b310, b320, b330, b410, b455, b510, b525, b640, b710, b715, b730, b735, b740, b755, b760, b770 |
| Riberto, et al. (2013) Brazil 20 |
132 persons with stroke in 3 Brazilian health institutions. | To validate a set of CIF codes for stroke, checking the frequency of problems in each individual. | III | Body functions - b110, b114, b117, b126, b130, b134, b140, b144, b147, b152, b156, b160, b164, b167, b172, b176, b180, b210, b215, b230, b235, b240, b265, b270, b280, b310, b320, b330, b340, b410, b415, b420, b430, b435, b440, b450, b455, b510, b515, b525, b530, b535, b540, b545, b550, b620, b630, b640, b710, b715, b730, b735, b740, b750, b755, b760, b770, b810 Body structure- s110, s410, s720, s730, s750 Activity and participation - d115, d120, d130, d135, d155, d160, d166, d170, d172, d175, d117, d210, d220, d230, d240, d310, d325, d330, d335, d345, d350, d360, d410, d415, d420, d430, d440, d445, d450, d455, d460, d465, d470, d475, d510, d520, d530, d540, d550, d560, d570, d620, d630, d640, d710, d750, d770, d845, d850, d860, d870, d910, d920, d930, d940 Environment - e110, e115, e120, e125, e135, e150, e155, e165, e210, e240, e250, e310, e315, e320, e325, e340, e355, e360, e410, e415, e420, e425, e440, e450, e455, e460, e465, e515, e525, e535, e540, e550, e555, e570, e575, e580, e590 |
| Beninato, Parikh & Plummer, (2014), USA 21 | 43 persons with a previous diagnosis of stroke. | To analyze the "Stroke Impact Scale - 16" in relation to individuals with stories of falls. | III | Body functions - b525, b620 Activity and participation - d415, d510, d530, d420, d450, d455, d430, d540, d640, d620 |
| Paanalahti, et al. (2014) Sweden22) | 22 persons with a previous diagnosis of stroke . | To validate a set of ICF codes for problems related to daily life on person with stroke. | III | Body functions - b110, b114, b117, b126, b130, b134, b140, b144, b152, b160, b164, b172, b176, b180, b210, b215, b220, b240, b260, b265, b270, b280, b320, b330, b410, b420, b435, b455, b510, b530, b550, b710, b730, b735, b740, b760, b765, b770, b780, b830 Body structure - s110, s410, s730, s750 Activity and participation - d110, d155, d160, d166, d170, d172, d175, d177, d210, d220, d230, d240, d310, d325, d330, d345, d350, d360, d410, d415, d420, d430, d440, d445, d450, d455, d460, d465, d470, d475, d510, d520, d530, d540, d550, d560, d570, d620, d630, d640, d710, d750, d760, d850, d855, d910, d920 |
| Wang et al. (2014) China23 | 208 persons with stroke | To verify the feasibility and validity of the ICF content describing the relevant aspects of body functions and environmental factors in stroke victims. | III | Body functions - b110, b114, b117, b126, b130, b134, b140, b144, b152, b156, b164, b167, b172, b176, b180, b210, b215, b260, b265, b270, b280, b310, b320, b330, b410, b415, b420, b455, b510, b525, b620, b640, b710, b715, b730, b735, b740, b750, b755, b760, b770 Body structure - s110, s410, s720, s730, s750 Activity and participation - d115, d155, d160, d166, d170, d172, d175, d210, d220, d230, d240, d310, d315, d325, d330, d335, d345, d350, d360, d410, d415, d420, d430, d440, d445, d450, d455, d460, d465, d470, d475, d510, d520, d530, d540, d550, d570, d620, d630, d640, d710, d750, d760, d770, d845, d850, d855, d860, d870, d910, d920, Environment - e110, e115, e120, e125, e135, e150, e155, e165, e210, e310, e315, e320, e325, e340, e355, e360, e410, e420, e425, e440, e450, e455, e460, e510, e525, e535, e540, e550, e555, e570, e575, e580, e590 |
| Benito García, et al. (2015) Spain24 | 24 persons with stroke | To evaluate the effectiveness of the rehabilitation program based on Bobath's concept. | III | Body functions - b7302, b4500, b4501, b4502, b4503 |
| Tarvonen-Schröder, et al. (2015). Finland 25 |
62 persons with stroke | -Comparison between the MIF and the ICF in assessing the ability and performance of a person with stroke. | III | Activity and participation - d330, d530, d450, d550 |
| Ottiger et al. (2015), Germany 26 | 102 persons with stroke | To develop and to assess the reliability and validity of a scale - LIMOS; To evaluate the correlation between LIMOS and MIF. |
III | Activity and participation - d510, d598 |
| Chen et al. (2016). China10 | 227 persons with stroke | To investigate how professionals' experience in ICF valuation determines its reliability. | III | Body functions - b110, b114, b140, b144, b167, b730 Body structure - S110, S730 Activity and participation - d310, d330, d450, d510, d530, d540, d550 Enviroment - e310, e355, e580 |
| Santana & Chun (2017), Brazil27 | 50 persons, over 18 years old, diagnosed with stroke | To evaluate and to classify aspects of language, functionality and participation of people with stroke based on the ICF | III | Body functions - b114, b144, b167, b176, b230, b310, b320, b330 Activity and participation - d160, d310, d315, d325, d330, d345, d350, d360, d450, d750, d760, d860, d910, d920 |
After analyzing the 11 articles, it appears that 160 ICF codes are mentioned, divided by Body Functions (53 codes, 33%), Activities and Participation (61 codes, 38%), Environmental Factors (40 codes, 25%) and Structures of the Body (6 codes, 4%).
Codes were selected with a frequency ≥ 50% and a total of 21 codes were identified, of which 6 codes (29%) related to the Body Functions component, 13 codes (61%) related to the Activities and Participation component, 2 codes (10%) referring to the Environmental Factors component.
In a comparative analysis of all the codes obtained, with codes with a frequency ≥ 50%, we can conclude that the Body Functions and Activities and Participation are the most evident categories, with a percentage of 33% and 38%, respectively. With regard to codes with a frequency ≥ 50%, it was found that Activities and Participation (61%) have greater evidence than body functions (29%). Regarding the Environmental Factors and Structures of the Body, they continued to have less evidence in patients with stroke, both in all articles and in ≥ 50% (Table 2).
Table 2 Frequency of occurrence of codes
| Total of analized articles | Analized articles > or = 50% | |||||
|---|---|---|---|---|---|---|
| Components | Number of articles | Nº of codes used | % of codes used | Nº of codes used | % of codes used | |
| Body functions | 11 | 53 | 33% | 6 | 29% | |
| Activity and participation | 11 | 61 | 38% | 13 | 61% | |
| Environmental factors | 11 | 40 | 25% | 2 | 10% | |
| Body structure | 11 | 6 | 4% | 0 | ||
The proposed core set for people with stroke features twenty-one main codes. The body functions component has six codes: b144 Memory functions, b730 Muscle strength functions, b114 Orientation functions, b140 Attention functions, b167 Mental language functions, b320 Joint functions.
In the Activities and Participation component, 13 codes are highlighted, d450 walking, d510 Washing, d530 Care related to the excretion processes, d330 Speaking, d540 Dressing, d550 Eating, d160 Focusing attention, d310 Communicating and receiving oral messages, d345 Writing messages, d410 Change basic body position, d420 Auto-transfers, d430 lifting and carrying objects and d455 moving.
In the Environmental Factors component, 2 codes are highlighted, e355 Health Professionals, e580 Services, Systems and Policies related to health (Table 3).
Table 3 Score Set ICF Stroke
| Components | Codes and Categories | (n) | Percentage % | |
|---|---|---|---|---|
| Body functions | b144 | Memory Functions | 7 | 64% |
| b730 | Muscle strength functions | 6 | 55% | |
| b114 | Guidance functions | 6 | 55% | |
| b140 | Functions of attention | 6 | 55% | |
| b167 | Mental functions of language | 6 | 55% | |
| b320 | Joint functions | 6 | 55% | |
| Activity and participation | d450 | Walking | 9 | 82% |
| d510 | Washing up | 8 | 73% | |
| d530 | Care related to excretion processes | 8 | 73% | |
| d330 | Speaking | 7 | 64% | |
| d540 | Dressing up | 7 | 64% | |
| d550 | Eating | 7 | 64% | |
| d160 | Focus attention | 6 | 55% | |
| d310 | Communicate and receive oral messages | 6 | 55% | |
| d345 | Writing messages | 6 | 55% | |
| d410 | Changing basic body position | 6 | 55% | |
| d420 | Auto-transfers | 6 | 55% | |
| d430 | Lifting and transporting objects | 6 | 55% | |
| d455 | Moving around | 6 | 55% | |
| Environmental factors | e355 | Health professionals | 6 | 55% |
| e580 | Health-related services, systems and policies | 6 | 55% | |
DISCUSSION
In this SLR, 11 articles were included, nine present designs that fit a quantitative approach. Study designs are heterogeneous, which may limit the results of this study.
It was possible to identify the score set most frequently used in studies carried out in people with stroke.
It should be noted that body structures have no evidence in the score set, as there is no code with a percentage ≥ 50%, so it seems that health professionals who care for people with stroke value Body Functions and Activities and Participation, in detriment of the Structures of the Body.
The results obtained in this SLR corroborate those obtained by Geyh et al.28 since, as in the score set presented here (Table 3), the greatest evidence lies in the Body Functions and Activities and Participation. However, these authors 28 evidence two codes in the structures of the body, s730 Structure of the Upper Limb and s110 Structure of the Brain, which, even not being included in the score set for this SLR, are the codes with the highest percentage (47% and 36%, respectively) within the Structures of the Body, accompanied by the code s750 Structure of the lower limb (36%).
In a study carried out in Sweden 29 the most affected functions after 6 months were: b130 Energy and conduction functions, b144 memory function, b455 exercise tolerance functions, b730 muscle strength, b740 muscle endurance functions, and b770 functions of the gait pattern. In terms of activity and participation, the most frequently mentioned ICF codes were: d630 preparing meals, d640 performing domestic tasks, d920 recreation and leisure. At least 50% of persons after stroke had problems at work, namely, d220 multiple tasks, d440 use fine hand movements, d450 walking and d460 moving in different places.
This SLR corroborates the results found in other studies carried out before 2013 (28,0) in which the functions of orientation, memory and attention, language and muscle strength stood out in the dimension of body functions; in activities and participation, the main areas mentioned were walking, washing, talking, dressing, eating, communicating and receiving oral messages and writing messages; and in the environment dimension, health professionals were mentioned, as well as health-related services, systems and policies. Furthermore, in the study by Seyh et al.28 at the level of the environment dimension, they address the immediate family (e310) and in the body structure they refer to the brain (s110).
As limitations of this study, we considered the heterogeneity of the designs of the included studies and the fact that one of the inclusion criteria was the availability of full texts.
Body functions are the physiological functions of organic systems (ICF) that, even if the body structures are altered due to stroke sequelae, the person is able, through a rehabilitation program, to overcome these changes and acquire skills to rebuild their autonomy and independence. For this reason, even if a person has a change in an organ or member (Body Structures), the most important thing is their independence and the ability to perform tasks and keep them involved in their everyday activities (Activities and Participation). These activities are related to the basic and instrumental activities of daily living,31 in which the specialist nurse in rehabilitation nursing plays an important role in enabling the person through teaching, instruction and training in activities of daily living.32
Implications for practice
With this SLR, it was possible to increase knowledge in nursing, as well as to contribute to simplifying the assessment of the persons functionality after stroke, since the most used ICF codes were highlighted, thus identifying the ICF Score Set for this specific population. In future investigations, it is recommended that content validation be performed by a panel of rehabilitation nurses (Delphi technique)28 and then clinical validation30 in order to verify the adequacy of the ICF score set that allows for the description health and health-related conditions, namely the functionality of people after stroke.
In the implementation and operationalization of the ICF, measures based on the ICF must be developed and detailed manuals on evaluation and completion must be drawn up in order to ensure inter-rater reliability.33
CONCLUSIONS
In this SLR, 11 studies were analyzed identifying 160 ICF codes used to classify and assess the characteristics of post-stroke patient.
After analyzing all the codes, more than 50% of the codes were selected, making a total of 21, distributed by the categories Body Functions, Activities and Participation and Environmental Factors, thus constituting the score set for patients with stroke.
It is important to introduce this information into the practice of specialist nurses in rehabilitation nursing, since the standardized classifications and languages describe and organize the data, in order to highlight the health gains sensitive to rehabilitation nursing care
REFERÊNCIAS BIBLIOGRÁFICAS
1 World Health Organization. WHO STEPS stroke manual: the WHO STEPwise approach to stroke surveillance. Geneva: World Health Organization; 2005. [ Links ]
2 Marques-Vieira C, Sousa L, Braga R. Reabilitar a pessoa com Acidente Vascular Cerebral. In C. Marques-Vieira; L. Sousa (Eds). Cuidados de Enfermagem de Reabilitação à Pessoa ao Longo da Vida. Loures: Lusodidacta. 2017:465-474. [ Links ]
3 Thrift AG, Thayabaranathan T, Howard G, Howard VJ, Rothwell PM, Feigin VL, Norrving B, Donnan GA, Cadilhac DA. Global stroke statistics. Int J Stroke. 2017 Jan;12(1):13-32. [ Links ]
4 Feigin VL, Norrving B, Mensah GA. Global Burden of Stroke. Circ Res. 2017 Feb 3;120(3):439-48. [ Links ]
5 Béjot Y, Bailly H, Durier J, Giroud M. Epidemiology of stroke in Europe and trends for the 21st century. Presse Med. 2016 Dec 1;45(12):e391-8. [ Links ]
6 Sousa Uva M, Antunes L, Rodrigues A, Pinto D, Nunes B, Dias CM. Acidente Vascular Cerebral: evolução e tendência da taxa de incidência na população sob observação da rede Médicos-Sentinela de 1990 a 2012. Congresso Nacional de Saúde Pública, 2-3 outubro 2014. Instituto Nacional de Saúde Doutor Ricardo Jorge, IP. [ Links ]
7 Instituto Nacional de Estatística. Causas de morte 2015 - Statistics Portugal. Lisboa: Instituto Nacional de Estatística. 2017. [ Links ]
8 National Stroke Association. Rehabilitation Therapy after a Stroke. Denver: National Stroke Association. (Acedido em 16.02-2018). Disponível em: http://www.stroke.org/we-can-help/stroke-survivors/just-experienced-stroke/rehab [ Links ]
9 Organização Mundial de Saúde. Classificação Internacional de Funcionalidade, Incapacidade e Saúde. Lisboa: Direção Geral de Saúde. 2004. [ Links ]
10 Chen S, Tao J, Tao Q, Fang Y, Zhou X, Chen H, Chen Z, Huang J, Chen L, Chan CC. Rater experience influences reliability and validity of the brief International Classification of Functioning, Disability, and Health Core Set for Stroke. J Rehabil Med. 2016 Mar 5;48(3):265-72. [ Links ]
11 Cieza A, Ewert T, Ustun TB, Chatterji S, Kostanjsek N, Stucki G. Development of ICF Core Sets for patients with chronic conditions. J Rehabil Med. 2004 Jul 1(44):9-11. [ Links ]
12 Sousa L, Firmino CF, Marques-Vieira CMA, Severino SSP, Pestana HCFC. Revisões da literatura científica: tipos, métodos e aplicações em enfermagem. Rev Port Enferm Reabit.2018; 1(1):46-55. [ Links ]
13 Bettany-Saltikov J. How to do a systematic literature review in nursing: a step-by-step guide. Berkshire (US): McGraw-Hill International; 2012 May 1. [ Links ]
14 Galvão TF, Pereira MG. Systematic reviews of the literature: steps for preparation. Epidemiol Serv Saude. 2014 Mar;23(1):183-4. [ Links ]
15 Joanna Briggs Institute, & Joanna Briggs Institute. 's user manual: version 5.0 system for the unified management. Assessment and Review of Information. Adelaide: Joanna Briggs Institute. 2011. [ Links ]
16 Sousa LMM, Marques JM, Firmino CF, Frade F, Valentim OS, Antunes AV. Modelos de formulação da questão de investigação na prática baseada na evidência. Rev Inv Enferm. S2(23):31-39. [ Links ]
17 Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic reviews. 2015 Dec;4(1):1. Acessivel em: https://doi.org/10.1186/2046-4053-4-1 [ Links ]
18 Campos TF, Rodrigues CA, Farias I, Ribeiro TS, Melo LP. Comparison of instruments for sleep, cognition and function evaluation in stroke patients according to the international classification of functioning, disability and health (ICF). Braz J Phys Ther. 2012 Feb;16(1):23-9. [ Links ]
19 Paanalahti M, Lundgren-Nilsson Å, Arndt A, Sunnerhagen KS. Applying the Comprehensive International Classification of Functioning, Disability and Health Core Sets for stroke framework to stroke survivors living in the community. J Rehabil Med 2013 Apr 5;45(4):331-40. [ Links ]
20 Riberto M, Lopes KA, Chiappetta LM, Lourenção MI, Battistella LR. The use of the comprehensive International Classification of Functioning, Disability and Health core set for stroke for chronic outpatients in three Brazilian rehabilitation facilities. Disabil Rehabil. 2013 Mar 1;35(5):367-74.. [ Links ]
21 Beninato M, Parikh V, Plummer L. Use of the International Classification of Functioning, Disability and Health as a framework for analyzing the Stroke Impact Scale-16 relative to falls. Physiother Theory Pract. 2014 Apr 1;30(3):149-56. [ Links ]
22 Paanalahti M, Murphy MA, Lundgren-Nilsson Å, Sunnerhagen KS. Validation of the Comprehensive ICF Core Set for stroke by exploring the patient's perspective on functioning in everyday life: a qualitative study. Int J Rehabil Res. 2014 Dec 1;37(4):302-10. [ Links ]
23 Wang P, Li H, Guo Y, Xie Y, Ge R, Qiu Z. The feasibility and validity of the comprehensive ICF core set for stroke in Chinese clinical settings. Clin Rehabil. 2014 Feb;28(2):159-71. [ Links ]
24 Benito García M, Arratibel A, Ángeles M, Terradillos Azpiroz ME. The Bobath Concept in walking activity in chronic Stroke measured through the International Classification of Functioning, Disability and Health. Physiother Res Int. 2015 Dec 1;20(4):242-50. [ Links ]
25 Tarvonen-Schröder S, Laimi K, Kauko T, Saltychev M. Concepts of capacity and performance in assessment of functioning amongst stroke survivors: a comparison of the Functional Independence Measure and the International Classification of Functioning, Disability and Health. J Rehabil Med. 2015 Jul 5;47(7):662-4. [ Links ]
26 Ottiger B, Vanbellingen T, Gabriel C, Huberle E, Koenig-Bruhin M, Plugshaupt T, Bohlhalter S, Nyffeler T. Validation of the new Lucerne ICF based Multidisciplinary Observation Scale (LIMOS) for stroke patients. PloS one. 2015 Jun 25;10(6):e0130925. [ Links ]
27 Santana MT, Chun RY. Language and functionality of post-stroke adults: evaluation based on International Classification of Functioning, Disability and Health (ICF). InCoDAS 2017; 29(1): e20150284. DOI:10.1590/2317-1782/20172015284 [ Links ]
28 Geyh S, Cieza A, Schouten J, Dickson H, Frommelt P, Omar Z, Kostanjsek N, Ring H, Stucki G. ICF Core Sets for stroke. J Rehabil Med. 2004 Aug 1;36(0):135-41. [ Links ]
29 Algurén B, Lundgren-Nilsson Å, Sunnerhagen KS. Functioning of stroke survivors-a validation of the ICF core set for stroke in Sweden. Disability and rehabilitation. 2010 Jan 1;32(7):551-9. [ Links ]
30 Quintas R, Cerniauskaite M, Ajovalasit D, Sattin D, Boncoraglio G, Parati EA, Leonardi M. Describing functioning, disability, and health with the international classification of functioning, disability, and health brief core set for stroke. Am J Phys Med Rehabil. 2012 Feb 1;91(13):S14-21. [ Links ]
31 Vigia C, Ferreira C, Sousa LM. Treino de Atividade de Vida. Marques-Vieira C., Sousa L. (Eds). Cuidados de Enfermagem de Reabilitação à Pessoa ao Longo da Vida. (p. 351-364). Loures: Lusodidacta. 2017. [ Links ]
32 Pestana, H. Cuidados de Enfermagem de Reabilitação: Enquadramento C. Marques-Vieira C., Sousa L. (Eds). Cuidados de Enfermagem de Reabilitação à Pessoa ao Longo da Vida. (p. 047-56). Loures: Lusodidacta. 2017. [ Links ]
33 Starrost K, Geyh S, Trautwein A, Grunow J, Ceballos-Baumann A, Prosiegel M, Stucki G, Cieza A. Interrater reliability of the extended ICF core set for stroke applied by physical therapists. Phys Ther. 2008 Jul 1;88(7):841-51. [ Links ]
Received: July 17, 2018; Accepted: November 26, 2018; Published: December 06, 2018











 text in
text in