Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista Portuguesa de Enfermagem de Reabilitação
versão impressa ISSN 2184-965Xversão On-line ISSN 2184-3023
RPER vol.1 no.2 Silvalde dez. 2018
https://doi.org/10.33194/rper.2018.v1.n2.02.4422
Articles
Eating Assessment Tool 10 In People With Stroke
1- Hospital Dr Fernando da Fonseca
2- Instituto Português de Oncologia de Lisboa
3- Centro Hospitalar Universitário Lisboa Central, Hospital de São José
4- Centro Hospitalar Lisboa Ocidental
5- Hospital Curry Cabral, Centro Hospitalar Universitário Lisboa Central
6- Escola Superior de Saúde Atlântica
Background:
Swallowing disorders often occur in Stroke. The Eating Assessment Tool-10 allows early detection of dysphagia and response to treatment.
Objective:
To evaluate the metric properties of the Eating Assessment Tool-10 in the person with Stroke that presents swallowing disorders.
Method:
Systematic Review of Literature based on the recommendations of the Joanna Brigs Institute for the PICo strategy, what are the metric properties of the Eating Assessment Tool-10 in people with Stroke that present a swallowing disorder? The research was carried out using the electronic database platforms: EBSCO, Host, Google Scolar, Cochrane Library Collection, Scielo and Proquest, having identified, selected, evaluated the methodological quality and included the articles that take into account the PRISMA recommendations.
Results:
Six studies were included that fulfilled the eligibility and methodological quality criteria. Studies on the reproducibility, validity and responsiveness of the Eating Assessment Tool-10 were found. However, this last property needs to be studied in future investigations. The limitation identified was the applicability of the scale in people with cognitive alterations.
Conclusions:
The Eating Assessment Tool-10 is a reliable, valid and responsive tool for people with stroke that present swallowing disorders.
Key words: Stroke; Psychometry; Deglutition Disorders; Reproducibility of results; Rehabilitation Nursing
Introdução:
Com o Acidente Vascular Cerebral, surgem com frequência alterações da deglutição. O Eating Assessment Tool-10 é um instrumento que permite detetar precocemente a disfagia e a resposta ao tratamento.
Objetivo:
Avaliar as propriedades métricas do Eating Assessment Tool-10 na pessoa com Acidente Vascular Cerebral com alteração da deglutição.
Método:
Revisão Sistemática da Literatura baseada nas recomendações do Joanna Brigs Institute para a estratégia PICo, quais a propriedades métricas do Eating Assessment Tool-10 em pessoas com Acidente Vascular Cerebral com alteração da deglutição? A pesquisa foi realizada com recurso a plataformas de bases de dados eletrónicas EBSCO, Host, Google Escolar, Cochrane Lybrary Collection, Scielo e Proquest, tendo sido identificados, selecionados, avaliados na qualidade metodológica e incluídos os artigos de acordo com as recomendações PRISMA.
Resultados:
Foram incluídos seis estudos que cumpriam os critérios de elegibilidade e de qualidade metodológica. Foram encontrados estudos sobre a reprodutibilidade, validade e responsividade do Eating Assessment Tool-10. Contudo, esta última propriedade necessita de ser estudada em futuras investigações. A limitação identificada foi na aplicabilidade da escala em pessoas com alterações cognitivas.
Conclusões:
O Eating Assessment Tool-10 é um instrumento fiável, válido e com responsividade, nas pessoas com AVC com alterações da deglutição.
Descritores: Acidente Vascular Cerebral; Transtornos de Deglutição; Psicometria; Reprodutibilidade dos resultados; Enfermagem em Reabilitação
Introducción:
Con el Accidente Vascular Cerebral, surgen con frecuencia alteraciones de la deglución. El Eating Assessment Tool-10 es un instrumento que permite detectar precozmente la disfagia y la respuesta al tratamiento. Objetivo: Evaluar las propiedades métricas del Eating Assessment Tool-10 en la persona con Accidente Vascular Cerebral con alteración de la deglución.
Método:
Revisión Sistemática de la Literatura basada en las recomendaciones del Joanna Brigs Institute para la estrategia PICo, cuáles las propiedades métricas del Eating Assessment Tool-10 en personas con Accidente Vascular Cerebral con alteración de la deglución. La investigación se realizó utilizando plataformas de bases de datos electrónicas EBSCO, Host, Google Escolar, Cochrane Lybrary Collection, Scielo y Proquest., Habiendo identificado, seleccionados, evaluados en la calidad metodológica e incluidos los artículos teniendo en cuenta las recomendaciones PRISMA.
Resultados:
Se incluyeron seis estudios que cumplían los criterios de elegibilidad y de calidad metodológica. Se han encontrado estudios sobre la reproducibilidad, validez y responsividad del Eating Assessment Tool-10. Sin embargo, esta última propiedad necesita ser estudiada en futuras investigaciones. La limitación identificada fue en la aplicabilidad de la escala en personas con alteraciones cognitivas.
Conclusiones:
El Eating Assessment Tool-10 es un test fiable, válido y con responsividad, en las personas con AVC con alteraciones de la deglución.
Palabras clave: Accidente Vascular Cerebral; Trastornos de Deglución; Psicometría; Reproducibilidad de los resultados; Enfermería en Rehabilitación
INTRODUCTION
Stroke is one of the leading causes of death and disability worldwide,1-3 with a high prevalence globally.3-4
At the beginning of the 21st century, the age-standardized incidence of stroke in Europe ranged from 95 to 290/100,000 inhabitants per year, with one-month mortality rates ranging from 13 to 35%. Every year, approximately 1.1 million people in Europe have had a stroke.5
The impact of ischemic and hemorrhagic stroke increased significantly worldwide between 1990 and 2010, that is, the number of cases, number of deaths and disability-adjusted life years (DALYs) lost.6
Dysphagia is a common complication in people with stroke, but the estimates of its frequency vary considerably.7 It is an important cause of pneumonia in the first days after stroke, having a major impact on clinical outcomes, mortality and institutionalization of these people.8
In a meta-analysis by Martino et al.9 the prevalence of dysphagia in people with stroke on acute phase is between 37% and 45% in screening evaluations, 51% and 55% in clinical evaluation and 64 and 78% detected with the help of assessment tools.
The concept of dysphagia, or swallowing difficulty, includes behavioral, sensory and motor changes that occur during swallowing, involving the state of consciousness before eating, visual recognition of food and responses to physiological odor and the presence of food.10 Despite all the complications described, the literature shows that dysphagia is underdiagnosed by health professionals.11 Impaired swallowing is a nursing diagnosis and is defined as an alteration in the ability to swallow.12
The early assessment of swallowing, within the first 4 hours after admission, is essential to start nutritional support for all people with acute stroke.13
There are several validated clinical and instrumental methods for diagnosing oropharyngeal dysphagia, and treatment is primarily based on compensatory measures. In this sense, more importance and attention should be given to oropharyngeal dysphagia and screening, treatment and regular monitoring protocols should be included and implemented to avoid its main complications.14
There are currently numerous scales at international level that allow the identification and assessment of dysphagia. However, in Portugal, there are not many instruments available and properly validated. Nonetheless, in 2012 two instruments were validated to assess the existence of dysphagia in the Portuguese population, the Eating Assessment Tool 10 (EAT 10) and the Functional Oral Intake Scale (FOIS).15
The EAT-10 scale was created by Belafsky et al.,16 it is considered a quick, simple and useful assessment tool to detect the existence of dysphagia and monitor the person's response to treatment. It allows easy access only to the self-perception of dysphagia and, based on this information, confirms the degree of commitment of the function and the limitations of functionality caused in people's social and emotional lives. The scale is composed of 10 items, and its completion is carried out by the person, without the need for prior functional assessment. Thus, it classifies the statements with a score ranging from 0 (no problem) to 4 (big problem), with a score equal or greater than 3 to be considered abnormal.
Considering that dysphagia is a problem with such a significant impact on people's lives, the specialist nurse in rehabilitation nursing plays an important role in the proper assessment of dysphagia. In this perspective, knowledge of the psychometric properties is essential in order to verify whether the test has validity and reliability, not to compromise the results obtained. Thus, it is intended to evaluate the metric properties of the EAT-10 in a person with stroke with swallowing disorders.
METHOD
A Systematic Literature Review (SLR) was used, as this allows the identification, selection and critical evaluation of a set of studies in order to extract the best scientific evidence.17 The main steps of an SLR were followed: research question, problem definition, systematic review objectives; inclusion and exclusion criteria; search strategy; procedure selection; data extraction procedure; and procedure for evaluating the methodological quality of the selected studies.18
Based on the PICo strategy recommendations of the Joanna Briggs Institute (JBI),19-20 the research question was formulated, where each dimension of the PICo contributed to define the inclusion criteria: Population (P) - People with stroke; Area of Interest (I) - EAT-10 metric properties and Context (Co) - swallowing/dysphagia alterations. Thus, the following research question was defined for this SLR: “What are the EAT-10 metric properties in a person with stroke with swallowing disorders?”.
The descriptors related to each of the components of the PICo strategy were: Stroke; Dysphagia Psychometrics; Validity of test; Reproducibility of results, previously validated in the Descriptors in Health Sciences and Medical Subject Headings platform. The following Keywords were also used: EAT 10 Assessment and Responsiveness.
The following were defined as eligibility criteria for the inclusion of articles: people with stroke, with swallowing/dysphagia disorders, at least one metric property, published in the last 5 years (2008-2014), in Portuguese, English and Spanish, with accessible full text. In evaluating the psychometric/clinicalmetric and metric properties, reproducibility, reliability, validity and responsiveness were taken into account.21-23
For the research, the strategy used was determined by searching different electronic databases, periodicals and gray literature, in order to find primary/original studies or secondary studies. The search was carried out through electronic database platforms: EBSCO, Host, Google Escolar, Cochrane Lybrary Collection, Scielo and Proquest.
The research was carried out by four people simultaneously, from October 15th to November 15th 2014, the same databases were used for the research, in order to respect inter-observer reliability.
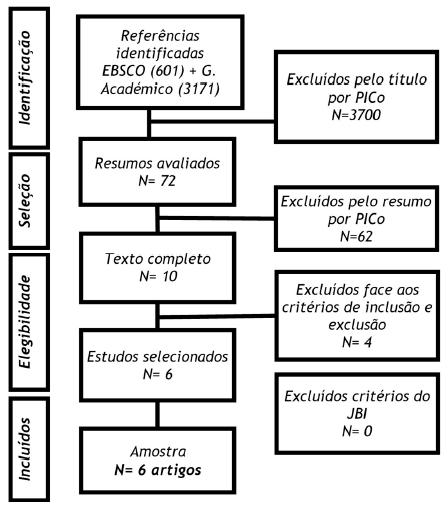
From the bibliographic research process carried out with this methodology, we obtained 3,772 articles for the initial selection. Out of these 3,700 were rejected by title or subject and 62 by abstract. Out of the 10 resulting, 4 were excluded after analysis of the full text, as they did not meet the defined inclusion criteria, with the final result of 6 articles included that met the inclusion criteria.
Table 1 describes the process of combining descriptors and keywords for searching the databases. Figure 1 illustrates the PRISMA24 flowchart corresponding to the identification, analysis, selection and inclusion of articles.
Table 1 Boolean Conjugation
| Boolean Conjugation | EBSCO | GOOGLE SCHOLAR |
|---|---|---|
| “EAT-10” | 235 | 580 |
| “EAT-10” and Deglutition Disorders | 33 | 595 |
| “EAT-10” and Dysphagia | 55 | 163 |
| “EAT-10” and Validity | 73 | 271 |
| “EAT-10” and Reproducibility of results | 65 | 796 |
| “EAT-10” and Responsiveness | 119 | 498 |
| “EAT-10” and Assessment | 8 | 81 |
| Psychometrics and “EAT-10” | 7 | 122 |
| “EAT-10” and Stroke | 53 | 267 |
| “EAT-10” and Stroke and Psychometrics | 3 | 34 |
| “EAT-10” and Stroke and Psychometrics and Swallowing disorders | 3 | 31 |
| Total of articles | 601 | 3171 |
The articles selected for full reading were independently evaluated by two investigators, according to methodological quality criteria proposed by the JBI,19 and articles with more than 75% of the criteria were selected.
Information was extracted from the articles on authors, year, country, sample, data on metric properties, conclusion and level of evidence. The classification of the levels of evidence of the included studies was based on the criteria of the Registered Nurses Association of Ontario.25
RESULTS
Six articles were included in this SLR, published in the following years: one in 2008,16 one in 2012,26 three in 201315,27,29 and one in 2014,28 in which the countries of origin were Brazil,29 Spain26,28, United States of America,16 Italy27 and Portugal.15 The sample of people with dysphagia ranged between 2315 and 482. 16 Regarding the control group, it ranged between 1028 and 269.27 All studies included (Table 2) are studies descriptive, with level of evidence III, meaning, evidence obtained from a well-designed, non-experimental study, such as comparative studies, correlation studies or case reports.25
Table 2 : Main results and conclusions of the six article
| Authors, Year, Country and Population | Results | Conclusions | Evidence Level |
|---|---|---|---|
| Queirós A, Moreira S, Silva A, Costa R, Lains J. 2013, Portugal n= 23 and 23 controls15 | EAT-10 presents acceptable internal consistency (0.75) and observer agreement (0.86), as well as discriminant validity. The results also indicated that the Portuguese version of the FOIS shows acceptable agreement between observers (0.78) and criterion validity. | Valid, reliable and reproducible | III |
| Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, Leonard RJ.. 2008, The United States, n=48216 | The internal consistency (Cronbach's alpha) was 0.960. The intra-item and test-retest correlation coefficients ranged between 0.72 and 0.91. The mean EAT-10 score was 23.58 ± 13.18 for people with esophageal dysphagia, 23.10 ± 12.22 for people with oropharyngeal dysphagia, 9.19 ± 12.60 for people with voice disorders, 22.42 ± 14.06 for people with head and neck cancer and 11.71 ± 9.61 for people with reflux. The mean EAT-10 score of people with dysphagia improved from 19.87 ± 10.5 to 5.2 ± 7.4 after treatment (p < 0.001). | Valid, reliable, reproducible and responsive. | III |
| Burgos R, Sarto B, Segurola H, Romagosa A, Puiggrós C, Vázquez C, Cárdenas G, Barcons N, Araujo K, Pérez-Portabella C.. 2012; Spain, n=6526 |
Internal reliability: good, Cronbach's Alpha 0.87 Validity: High correlation between scale items and total score (p˂0.001). People with dysphagia = 15 ± 8.9 of People at risk of dysphagia = 6.7 ± 7.7 and People without risk of dysphagia = 2 ± 3.1. There was a Moderate correlation between total score and age (Spearman's Coefficient=0.37) |
Reliable and valid | III |
| Schindler A, Mozzanica F, Monzani A, Ceriani E, Atac M, Jukic-Peladic N, Venturini C, Orlandoni P, 2013, Italy n=304 e 269 control27 | - Reproducibility: Internal Consistency (Cronbach's Alpha) in a group of people with dysphagia = 0.90 and for a group of healthy people = 0.93 - Pearson's Correlation Coefficient (0.95 in people with dysphagia and 0.98 in asymptomatic individuals) - Intraclass Correlation (ICC): 0.95 and 0.98, respectively - Cut-off 2.8. Normal if ≤ 2.8 - Correlation between the scores of people with dysphagia and healthy individuals was low. - People with dysphagia had higher values of the score in each item and in total - The EAT-10 total score correlated positively with the assessment through endoscopy - When using the EAT-10 before and after the rehabilitation plan, there was a weak and positive correlation p=0.4. |
Valid, reliable and responsive. |
III |
| Rofes L, Arreola V, Mukherjee R, Clave P.; 2014, Spain, n= 160 e 10 controls28 | - Applied EAT-10 in 133 people with diaphagia (101 with a score ≥3 (75.9%)) - Applied the V-VST in 134 people with dysphagia (in 105 had swallowing disorders (78.4%)) - Accuracy was 0.89 in EAT 10 (ROC curve) - Cut-off: 2 - EAT 10 showed high levels of sensitivity, in detection (0.895), in insecurity in swallowing (0.915) and silent aspiration (0.933) |
Valid | III |
| Gonçalves MI, Remaili C, Behlau M.; Brazil, 2013 N=10729 |
- Discriminative power of 72. 97% - Sensitivity of 69.70% and Specificity of 72. 00% - Cut-off > 3 |
Valid | III |
DISCUSSION
Reproducibility
The internal consistency assessed by Cronbach's alpha ranged between 0.7515 and 0.9616. In the validation study of the Italian version it was 0.9027 and in the study of the Spanish version it was 0.87.26
In studies where internal consistency was assessed15-16,26-27 the scale proved to be reliable as it was higher than 0.7, with values classified as reasonable and excellent21-23.
In the inter-observer agreement, the value of the test was 0.86 in the Portuguese version15, which demonstrates good inter-observer reproducibility.21-23 The test-retest ranged from 0.72 to 0.91 for the American version16 and in the Italian version ranged between 0.95 and 0.98.27 which demonstrated its stability or intra-observer reproducibility. 21-23
Validity
In the validity study, was intended to verify whether the instrument evaluate what it was supposed to evaluate.21-23 Construct validity was verified through the correlation of the items with the total score of the scale, in the study by Belafsky et al.16 Criterion validity was the most studied, through discriminant validity,15-16,26-27 in which it was found that the EAT-10 can discriminate people with dysphagia from healthy individuals, proving to be valid for the purpose of the scale: detect the existence of dysphagia.
The study carried out by Rofes et al.28 highlighted the importance of increasing the sensitivity of the test by around 5%, through the analysis of the ROC curve, defining the cut-off value for ≤ 2, which was found not to affect specificity, resulting in fewer false negatives.
Responsiveness
Through the study by Belasfky et al.16 and Schindler et al.27 it was concluded that the EAT-10 is responsive, as it was shown that this is sensitive to change, namely in the changes in the before and after treatment and plan of rehabilitation in the group of people with dysphagia p< 0.001 and p= 0.01, respectively. However, it was the least studied metric property, the ceiling effect, floor effect, magnitude effect were not verified.21-23
The EAT-10 scale proved to be an easy-to-understand and quick-completion instrument, considered useful in clinical practice for detecting dysphagia. In the study by Burgos et al.,26 as well as in the study by Schindler et al.27, the limitation of this scale was unanimously highlighted, as it is not suitable for its applicability in individuals with cognitive alterations, as it requires person's participation. However, in the article by Gonçalves et al.,15 it was also found that in 13 of the participants, the questionnaire was read to them due to difficulties in reading or understanding the instructions or because of the absence of glasses at the time of the exam.
It is also relevant to consider the conclusion of the SLR, performed by Speyer Speyer et al.30 whose established objective was to assess the psychometric properties of the instruments for the functional assessment of oropharyngeal dysphagia, including the EAT-10. In this study, was concluded that the instruments that included the EAT-10 verified that the validity and reproducibility were classified as insufficient. In this sense, the authors recommended the development of new scales that meet the criteria of reasonableness of the psychometric properties.
Practical implications
Most of the studies included in the SLR carried out the validation study in people with swallowing/dysphagia disorders that appeared in the context of stroke.
Since dysphagia is a common and highly prevalent consequence in people with stroke, it is considered important for clinical practice to carry out further studies that assess all metric properties, with a special focus on responsiveness.
Being dysphagia, a increasingly problem with a great impact on personal life, it is up to the Specialist Nurse in Rehabilitation Nursing to adequately assess and manage dysphagia. Through an individual rehabilitation program, it is intended to adopt appropriate strategies so that the person with dysphagia or swallowing disorders is as autonomous as possible, integrating them into their family and community.
Through the numerous duly validated assessment instruments, namely the EAT-10 scale, the Specialist Nurse in Rehabilitation Nursing is able to identify early swallowing changes, diagnose, intervene and measure the results of their interventions as quickly as possible. It is intended, therefore, to reduce the occurrence of complications and to contribute to an improvement in the care of the person, promoting an improvement in the quality of life.
CONCLUSION
Based on the reading and analysis of the six articles included in this SLR, it was possible to know and to assess the psychometric properties of the EAT-10 scale in people with stroke with swallowing disorders or dysphagia. It was found that the EAT-10 was considered an assessment instrument that proved to be valid in the original English language version as well as in the versions in which cross-cultural equivalence was verified, namely, Portugal, Brazil, Spain and Italy.
The absolute limitation found in the applicability of the EAT-10 scale focused on the incompatibility of its use in individuals with cognitive alterations, as it is a self-assessment scale. Other relative limitations found were related to changes in visual acuity, difficulty in reading or writing.
It was verified with the accomplishment of this work, that there are still few articles that include in their study the responsiveness evaluation, in a pre-established period of time.
REFERÊNCIAS BIBLIOGRÁFICAS
1 World Health Organization. Stroke, Cerebrovascular accident. Health topics. 2016. Disponível em:http://www.who.int/topics/cerebrovascular_accident/en/ [ Links ]
2 Norrving B, Davis SM, Feigin VL, Mensah GA, Sacco RL, Varghese C. Stroke prevention worldwide-what could make it work. Neuroepidemiology. 2015;45(3):215-20. [ Links ]
3 Thiele I, Linseisen J, Heier M, Holle R, Kirchberger I, Peters A, Thorand B, Meisinger C. Time trends in stroke incidence and in prevalence of risk factors in Southern Germany, 1989 to 2008/09. Sci Rep. 2018 Aug 10;8(1):11981. [ Links ]
4 Marques-Vieira C, Sousa L, Braga R. Reabilitar a pessoa com Acidente Vascular Cerebral. In C. Marques-Vieira; L. Sousa (Eds). Cuidados de Enfermagem de Reabilitação à Pessoa ao Longo da Vida. Loures: Lusodidata. 2017: 465-474. [ Links ]
5 Béjot Y, Bailly H, Durier J, Giroud M. Epidemiology of stroke in Europe and trends for the 21st century. Presse Med. 2016 Dec 1;45(12):e391-8. [ Links ]
6 Krishnamurthi RV, Feigin VL, Forouzanfar MH, Mensah GA, Connor M, Bennett DA, Moran AE, Sacco RL, Anderson LM, Truelsen T, O'Donnell M. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health. 2013 Nov 1;1(5):e259-81. [ Links ]
7 González-Fernández M, Ottenstein L, Atanelov L, Christian AB. Dysphagia after Stroke: an Overview. Curr Phys Med Rehabil Rep. 2013;1: 187-196. [ Links ]
8 Arnold M, Liesirova K, Broeg-Morvay A, Meisterernst J, Schlager M, Mono ML, El-Koussy M, Kägi G, Jung S, Sarikaya H. Dysphagia in acute stroke: incidence, burden and impact on clinical outcome. PLoS One. 2016 Feb 10;11(2):e0148424. [ Links ]
9 Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke - incidence, diagnosis, and pulmonary complications. Stroke. 2005;36(12):2756-2763. [ Links ]
10 Leopold NA, Kagel MC. Prepharyngeal dysphagia in Parkinson's disease. Dysphagia. 1996 Dec 1;11(1):14-22. [ Links ]
11 Cichero JA, Altman KW. Definition, prevalence and burden of oropharyngeal dysphagia: a serious problem among older adults worldwide and the impact on prognosis and hospital resources. InStepping stones to living well with dysphagia 2012 (Vol. 72, pp. 1-11). Karger Publishers. [ Links ]
12 Conselho Internacional de Enfermeiros. CIPE versão 2: Classificação internacional para a prática de enfermagem. Lisboa:Ordem dos enfermeiros; 2011. [ Links ]
13 Han TS, Lean ME, Fluck D, Affley B, Gulli G, Patel T, Barrett C, Kakar P, Sharma S, Sharma P. Impact of delay in early swallow screening on pneumonia, length of stay in hospital, disability and mortality in acute stroke patients. Eur J Clin Nutr. 2018 Mar 27:1. [ Links ]
14 Baijens LW, Clave P, Cras P, Ekberg O, Forster A, Kolb GF, Leners JC, Masiero S, Mateos-Nozal J, Ortega O, Smithard DG. European Society for Swallowing Disorders-European Union Geriatric Medicine Society white paper: oropharyngeal dysphagia as a geriatric syndrome. Clin Interv Aging. 2016;11:1403. [ Links ]
15 Queirós A, Moreira S, Silva A, Costa R, Lains J. Contributo para a Adaptação e Validação da Eat Assessment Tool (EAT-10) e da Functional Oral Intake Scale (FOIS). Rev Soc Port Med Fis Reabil. 2013;24(2):25-30. [ Links ]
16 Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, Leonard RJ. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008 Dec;117(12):919-24. [ Links ]
17 Bettany-Saltikov J. How to do a systematic literature review in nursing: a step-by-step guide. New York: Open University press; 2012. [ Links ]
18 Sousa LMM, Firmino CF Marques-Vieira CMA, Severino S, Pestana HCFC. Revisões da literatura científica: tipos, métodos e aplicações em enfermagem. Rev Port Enferm Reabil.2018; 0:46-55. Disponível em: http://www.aper.pt/ficheiros/revista/rpernv1n1.pdf [ Links ]
19 Joanna Briggs Institute (2011). Joanna Briggs Institue's user manual: version5.0 system for the unified management. Assessment and Review of Information. Adelaide: The Joanna Briggs Institute. 2011. Available in http://www.joannabriggs.org/assets/docs/sumari/SUMARI-V5-User-guide.pdf [ Links ]
20 Sousa LM, Marques JM, Firmino CF, Frade F, Valentim OS, Antunes AV. Modelos de formulação da questão de investigação na prática baseada na evidência. Rev Invest Enferm.2018; S2(23):31-39. [ Links ]
21 Sousa LM, Marques-Vieira C, Carvalho ML, Veludo F, José HM. Fidelidade e validade na construção e adequação de instrumentos de medida. Enformação. 2015; 5:25-32. Disponível em http://hdl.handle.net/10884/1016 [ Links ]
22 Sousa LM. As propriedades psicométricas dos instrumentos de hétero-avaliação. Enformação. 2015;6:20-4. Disponível em http://hdl.handle.net/10884/998 [ Links ]
23 Sousa LM, Marques-Vieira C, Severino S, Caldeira S. Propriedades psicométricas de instrumentos de avaliação para a investigação e prática dos enfermeiros de reabilitação. In C. Marques-Vieira, L. Sousa (Eds). Cuidados de Enfermagem de Reabilitação à Pessoa ao Longo da Vida. Loures: Lusodidacta. 2017:113-122. [ Links ]
24 Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA). Welcome to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). 2015. Disponível em http://www.prisma-statement.org/ [ Links ]
25 Registered Nurses'Association of Ontario. Falls prevention: building the foundations for the patient safety. A self-learning package. Toronto: Registered Nurses' Association of Ontario. 2007 Available in http://rnao.ca/sites/rnao-ca/files/Falls_Prevention_-_Building_the_Foundations_for_Patient_Safety._A_Self_Learning_Package.pdf. [ Links ]
26 Burgos R, Sarto B, Segurola H, Romagosa A, Puiggrós C, Vázquez C, Cárdenas G, Barcons N, Araujo K, Pérez-Portabella C. Traducción y validación de la versión en español de la escala EAT-10 (Eating Assessment Tool-10) para el despistaje de la disfagia. Nutr Hosp. 2012 Dec;27(6):2048-54. [ Links ]
27 Schindler A, Mozzanica F, Monzani A, Ceriani E, Atac M, Jukic-Peladic N, Venturini C, Orlandoni P. Reliability and validity of the Italian eating assessment tool. Ann Otol Rhinol Laryngol. 2013 Nov;122(11):717-24. [ Links ]
28 Rofes L, Arreola V, Mukherjee R, Clave P. Sensitivity and specificity of the Eating Assessment Tool and the Volume-Viscosity Swallow Test for clinical evaluation of oropharyngeal dysphagia. Neurogastroenterol Motil. 2014 Sep;26(9):1256-65. [ Links ]
29 Gonçalves MI, Remaili C, Behlau M. Equivalência cultural da versão brasileira do Eating Assessment Tool-EAT-10. CoDAS., São Paulo. 2013 Dec;25(6):601-4. [ Links ]
30 Speyer R, Kertscher B, Cordier R. Functional health status in oropharyngeal dysphagia. J Gastroenterol Hepatol Res. 2014;3(5):1043-8. [ Links ]
Received: September 04, 2018; Accepted: November 26, 2018; Published: December 06, 2018











 texto em
texto em