Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Portuguesa de Enfermagem de Reabilitação
Print version ISSN 2184-965XOn-line version ISSN 2184-3023
RPER vol.1 no.1 Silvalde June 2018
https://doi.org/10.33194/rper.2018.v1.n1.08.4389
Articles
Timed Up And Go Test In Community-dwelling People With Stroke
1- IPO Francisco Gentil de Lisboa
2- Centro Hospitalar Tâmega e Sousa
5- Escola Superior de Saúde Atlântica
Background:
Stroke is the first cause of acquired disability in adults, causing changes in the normal gait pattern. The use of evaluation tools that are easy to apply, valid, reliable and responsive is imperative.
Objective:
To evaluate the metric properties of the Timed Up and go Test in community-dwelling people with stroke.
Method:
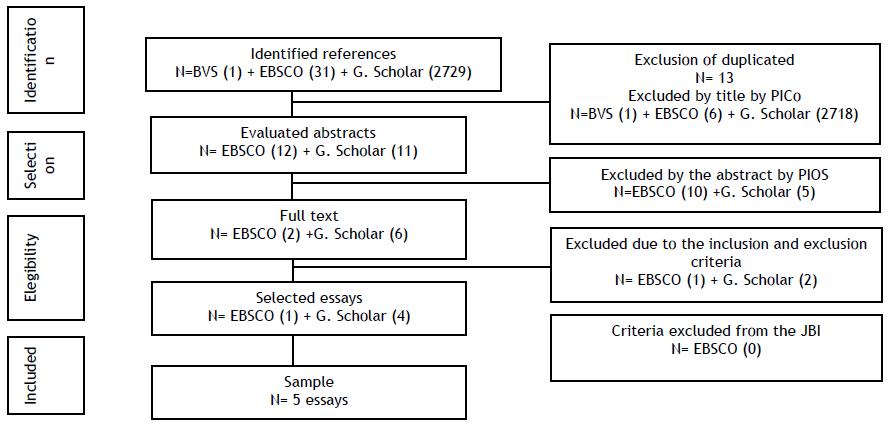
Systematic Review of Literature based on the recommended actions of the Joanna Brigs Institute for the PICo strategy and PRISMA recommendations, starting with the question: "What are the metric properties of the Timed Up and Go test in community-dwelling people with stroke?"
Results:
Five studies were included in this review. This test presents significant reproducibility values and responsiveness. Criterion and construct validity is demonstrated in two studies.
Conclusions:
The Timed Up and go Test can be considered as a reliable, valid instrument with responsiveness in community-dwelling people with stroke.
Keywords: stroke; psychometry; postural balance; reproducibility of results; nursing in rehabilitation
Introdução:
O Acidente Vascular Cerebral é a primeira causa de incapacidade adquirida no adulto, provocando alterações no padrão de marcha normal. A utilização de instrumentos de avaliação, de fácil aplicação, válidos, fiáveis e responsivos é imperativo.
Objetivo:
Avaliar as propriedades métricas do Timed Up and go Test na pessoa com Acidente Vascular Cerebral, residente na comunidade.
Método:
Revisão Sistemática da Literatura baseada nas recomendações do Joanna Brigs Institute para a estratégia PICo e recomendações PRISMA, partindo-se da questão: “Quais as propriedades métricas do Timed Up and go test na pessoa com Acidente Vascular Cerebral, residente na comunidade?”
Resultados:
Foram incluídos cinco estudos nesta revisão. Este teste apresenta valores de reprodutibilidade significativos, e de responsividade. A validade de critério e de constructo é demonstrada em dois estudos.
Conclusões:
O Timed Up and go Test pode ser considerado como um instrumento fiável, válido e com responsividade, nas pessoas com AVC residentes na comunidade.
Palavras chave: acidente vascular cerebral; psicometria; equilíbrio postural; reprodutibilidade dos resultados; enfermagem em reabilitação
Introducción:
El Accidente Vascular Cerebral es la primera causa de incapacidad adquirida en el adulto, provocando cambios en el patrón de marcha normal. El uso de instrumentos de evaluación, de fácil aplicación, válidos, fiables y responsivos es imperativo.
Objetivo:
Evaluar las propiedades métricas del Timed Up and go Test en la persona con Accidente Vascular Cerebral, residente en la comunidad.
Método:
Revisión Sistemática de la Literatura basada en las recomendaciones del Joanna Brigs Institute para la estrategia PICo y recomendaciones PRISMA, partiendo de la cuestión: ¿Cuáles son las propiedades métricas del Timed Up and Go Test en la persona con Accidente Vascular Cerebral, residente en la comunidad?
Resultados:
Se incluyeron cinco estudios en la revisión. El test presenta valores de reproducibilidad significativos, y de responsividad. La validez de criterio y de constructo se demuestra en dos estudios.
Conclusiones:
El Timed Up and Go Test puede considerarse como un instrumento fiable, válido y con responsividad en las personas con AVC residentes en la comunidad.
Palavars clave: accidente vascular cerebral; psicometría; equilibrio postural; reproducibilidad de los resultados; enfermeria en rehabilitación
INTRODUCTION
The World Health Organization (2015) defined cerebrovascular accident (CVA) as a focal (or sometimes global) neurological impairment, of sudden occurrence and lasting more than 24 hours (or causing death) and of probable vascular origin.[1] Stroke has a high prevalence worldwide.[2] As the population ages, the incidence of this pathology increases. Inevitably, when approaching the subject, aging is referred to as an increase in the risk of stroke associated with age. [1,3] About 60 to 70% of strokes occur in people over 65, making it a major problem for our society.[3]
It is the first cause of acquired incapacity in the adult, leaving physical, mental and social sequelae as a rule, particularly restricting the person's functionality. It is characterized by a total or partial loss of motor function on one side of the body, and according to the WHO International Classification of Functioning, Disability and Health,[4] the functions of gait and balance in a person with stroke are compromised, limiting the performance of Activities of Daily Living.
Gait symmetry and some spatiotemporal parameters are affected, causing deficit in motor resources, with direct repercussions on gait.[5] There is a partial loss of muscle strength, with a shift in the center of gravity, change in the base of support and transfer of weight to the healthy side. The performance of any motor activity implies the integrity of the postural center. Difficulty in transferring weight to the affected side interferes with postural control, causing loss of stability and preventing guidance in performing movements.[6]
The impossibility or difficulty in performing a walk is considered to be one of the most disabling and frustrating problems for a person in post-stroke. More than half of people do not walk independently in the acute phase after stroke; furthermore, such dependence is based on 25% of people after 3 months.[7] Gait recovery is one of the main goals of rehabilitation, in order to promote autonomy and increase the person's quality of life.[2] The Rehabilitation nurse has a fundamental role in the process of adaptation to the person's new condition of life, in the application of actions that improve and limit the impact of disability, thus contributing to the maintenance and recovery of quality of life. [8] For this, rehabilitation nurse has technical, relational and educational competences that allow training, the promotion of autonomy, in order to reduce the impact of stroke in the life of the person and family.[9]
Gait instability, in line with postural changes and neuromuscular disorders caused by stroke are often the cause of falls. [10] People who have had a stroke may have an incidence of falls greater than 73% in the first six months.[12] Currently, there are balance and gait assessment instruments that allow the assessment of these two functions. Assessment tools are useful in defining the objective, documenting needs, and demonstrating the operations performed. [13] In people with stroke, an assessment of postural control and the risk of falls is highly provided, thus, in this context,
the evaluation protocols evaluated usually include the Timed Up and Go. [14] This is a test of balance, related to the level of functional mobility. It is a quick and simple assessment tool allowing to assess the risk of falling in a person.[3] This test requires that participants get up from a chair, walk 3 meters, return to the chair and sit down again. The time taken to complete the test is recorded in seconds using a stopwatch. The participant can walk with a cane or other walking aid. [13] The knowledge of psychometric properties is essential in order to verify whether the test has validity and reliability, so as not to compromise the results obtained. In this sense, it is intended to evaluate the psychometric properties of the Timed up and Go Test, to ensure that the results obtained after its application are not biased. The aim of this study is to identify the metric properties of the Timed and Go Test in community-dwelling people after stroke.
MATERIAL AND METHODS
Systematic Literature Reviews (SLR) allows the identification, selection and critical evaluation of a set of studies in order to extract the best scientific evidence to answer a research question. The main purpose of SLR is to gather all the empirical evidence through the application of systematic and explicit methods, in order to reduce biases, in order to obtain more reliable results, and thus draw more adequate conclusions. [14]
A systematic literature review was carried out, as it is a careful process, which allows the identification, evaluation and interpretation of all available and relevant research, in order to answer a question that arises in the context of clinical practice. The fundamental elements of a systematic review consist of 8 steps: research question, problem definition, systematic review objectives; inclusion and exclusion criteria; search strategy; selection procedure; data extraction procedure; and procedure for assessing the methodological quality of selected studies.[15]
A systematic quality review should contain the formulation of one and only one starting question, being it sufficiently understandable and specific.[14] To formulate the research question, the recommendations of the Joanna Briggs Institute[16] were considered based on the PICo strategy (Population, Interests area, context). Each dimension of the PICo contributed to the definition of the inclusion criteria: P- Population: Adult person with stroke; I- area of interest: the psychometric properties of the Timed Up and Go Test; Co - Context: resident in the community.
Having resulted in the research question: “What are the metric properties of the Timed Up and go test in the person with stroke, living in the community?”.
The descriptors related to each of the components of the PICo strategy were identified, Stroke; Psychometrics; validity of test, Reproducibility of results, Postural Balance, previously validated in the Descriptors in Health Sciences and Medical Subject Headings platform. The following keywords were also used: Timed up and go test and community resident. The electronic search was carried out during the month of October 2016 using the EBSCOHost® platform (CINAHL®, Nursing & Allied Health Collection, British Nursing Index, Cochrane Collection, MEDLINE®), Virtual Health Library (BVS) and Academic Google. Subsequently, the descriptors with the following research strategy were inserted into these databases: (Table 1)
Table 1 Research strategy
| (Timed and Go Test) AND (Stroke) |
| (Timed and go Test) AND (Stroke) AND (Community) |
| (Stroke) AND (Timed up and Go Test) AND (Community) AND (Rehabilitation) |
| (Stroke) AND (Timed up and Go Test) AND (Psychometrics) |
| (Stroke) AND (Timed up and Go Test) and (Reproducibility of results) |
| (Stroke) AND (Timed up and Go Test) AND ( Postural Balance) AND (Reproducibility of results) |
| (Stroke) AND (Timed up and Go Test) AND (Psychometrics) AND (Reproducibility of results) AND (Postural Balance) AND (Rehabilitation) |
| (Stroke) AND (Timed up and Go Test) AND (Psychometrics) AND (Reproducibility of results) AND (Postural Balance) |
In a systematic quality review, the inclusion and exclusion criteria must be defined rigorously, transparently, in order to guide the research and select the scientific literature, so that all relevant studies can be included and the irrelevant ones excluded, in order to increase the accuracy of the results against the identified issue.[14] The following inclusion criteria were considered: Adult person with stroke, Evaluate at least one psychometric parameter, Quantitative Study, with publication date between 2011 and 2016, in Portuguese/English/Spanish/French, and article available in full and free access. As exclusion criteria, articles that present less than 75% of the JBI quality criteria were defined, that is, the Joanna Briggs Institute 2011 grid. Articles of systematic literature review were also defined as exclusion criteria.
After identifying the research question, the inclusion and exclusion criteria and the research strategy, the study selection procedure was defined in order to filter the studies. The exact definition of this procedure reduces bias and possible errors, making it possible to select all articles in the same way, and ensure the validity and veracity of the results.[14] The selection process involved, in a first phase, the independent analysis of the researchers, the titles and abstracts of the articles, taking into account the criteria defined in advance. The entire study selection process was recorded in a selection grid by two investigators. Subsequently, the results of the selection of investigators were compared and in case of divergences, another investigator was used.
The researchers then proceeded to select the articles independently, based on the previously defined inclusion and exclusion criteria. Quantitative studies were only selected for presenting a higher level of evidence and for responding more satisfactorily to the purpose of this review. Each investigator assessed the methodological quality of the studies based on the JBI classification for descriptive studies.
The information contained in the essays was systematized in a table, which allowed a better interpretation of the results obtained in each study. The levels of evidence from the studies contained in the articles were classified according to the criteria of the Registered Nurses Association of Ontario.[18]
RESULTS
The five essays that make up the sample were published in the following years, one in 2011,[23] two in 2013[19,21] and two in 2014,[20,22] with the countries of origin being Brazil,[19,23] United States of America (USA),[21] Sweden[22] and Australia.[20] All studies included (Table 2) are descriptive studies, with level of evidence III.[18]
Tabela 2 : Principais Resultados e conclusões dos cinco artigos
| AUTHORS, YEAR, COUNTRY AND POPULATION | RESULTS |
CONCLUSIONS |
||
|---|---|---|---|---|
| Reproducibility | Validity | Responsiveness | ||
| Faria C., Teixeira-Salmela L., Nadeau S., 2013, Brazil, n= 44[19] | -- | Discriminant and predictive validity at lens and moderate speed in stroke and healthy people | -- | Valid |
| Vernon S., Paterson K, Bower K, McGinley J, Miller K, Pua Y-H et al. 2014, Australia, n=30[20] | Test-retest Intraclass correlation coefficient (ICC) >0.90 |
Validity Competitor between TUG and Kinect-TUG Predictive validity of TUG on Age and stride length |
Effect Size (sensibility to changing) |
Valid, reliable and responsive |
| Murphy K, Lowe S. 2013; USA, n=15[21] |
Test-retest Pearson correlation coefficient r=0.77 and after training 0.86 |
-- |
-- | Reliable |
| Persson C. Danielsson A., Sunnerhagen K, Grimby-Ekman A. and Hansson P-O, 2014, Sweden n=91[22] | -- | -- | Linear regression model IC =95%, p<0.001 |
Responsive |
| Faria C, Teixeira-Salmela L, Gomes Neto M, Rodrigues-de-Paula F. 2011, Brazil, n= 16[23] |
Intra-observer (0.75<ICC<0.96) and inter-observer (0.91<ICC<0.96) reliability. | -- | -- |
Reliable |
Reproducibility
The US study [21] assesses the inter-observer reproducibility between a nurse and a physical therapist, with the aim of demonstrating the importance of training professionals in the application of an instrument such as the TUG. Initially, the TUG was applied without professional training, with the inter-observer reliability being 0.77, and after training, it increased to 0.86 (p=0.001).
One of the studies from Brazil[23] addresses intra- and inter-observer reliability, with the application of TUG being performed by experienced physiotherapists at different times. Significant values of intra-observer (0.75<ICC<0.96) and inter-observer (0.91<ICC<0.96) reliability were obtained.
In the study in Australia,[20] through the retest test, reliability was demonstrated in most of the Kinect-TUG variables, with ICC> 0.90.
Validity
Regarding the discriminant validity, one of the studies in Brazil[19] assesses the difference between the TUG means of a group of healthy individuals and a group with stroke in the community. Through ANOVA, the researchers verified that there were differences in the TUG means in the healthy group and in the stroke group. Each group was divided into 3 subgroups: Fast, Moderate and Slow, depending on the TUG results (according to quartiles). For both stroke groups (F=26.21; p<0.013) versus Healthy (F=32.73; p<0.006), there were significantly different results between the various subgroups. The ANOVA analysis of variance also revealed a significant interaction between groups and subgroups, since the differences in measurements between groups depended on the values obtained by the subgroups. However, in the Fast subgroup, TUG cannot discriminate the stroke group from the Healthy group, since the performance is similar.
Also in this study [19] the predictive validity or accuracy was evaluated. According to the analysis, 86.4% of the individuals were well classified, in relation to the association predictions made from the results obtained by the TUG. But there was an exception in the CVA Rapids subgroup, as it has very identical values to the Healthy Rapids subgroup.
Regarding concurrent validity, the study from Australia,[20] indicates excellent validity values between the total time of the TUG and all the Kinect-TUG variables, with the exception of the trunk flexion angle (p=-0.23, P> 0.05) , and the step length (p=0.70, P<0.001). The total time of the TUG was considered a significant predictor, when associated with step length and age, in the evaluations of the 10-meter walk test (10 MWT) and Step Test. There was a 7% (P<0.01), and 6% (P=0.03) improvement, respectively, in the performance of the regression model.
Responsiveness
One study,[22] carried out in Sweden, investigated responsiveness by evaluating TUG in 91 people during the first year after the first stroke in the community (at week 1, at 3 months, at 6 months and at 12 months). A non-parametric statistic (median and 25th and 75th percentile) and the linear regression model were used, leading to the conclusion that the TUG is a responsive test during the first three months after stroke, given that there was a reduction in the mean time by 5 .3 seconds (95% CI, p<0.001). In the assessments carried out at intervals between 3-6 months and 6-12 months after stroke, the mean time did not have a statistically significant change. All changes verified from one assessment to another are only always detected in the youngest.
In the study from Australia,[20] the TUG was evaluated using a motion sensor camera (Kinect), which allows to provide useful information about the performance of independent components of motion. The Kinect - TUG association provides information on sensitivity to change (responsiveness). The Effet Size observed in the study was compared with the respective minimum detected results of 0.17m/s for walking speed and 1.7 steps for the Step Test.
DISCUSSION
The TUG is one of the most used mobility assessment instruments nationally and internationally, covers most basic activities and is practical and quick to apply.[25] Knowledge of the metric properties of an instrument allows for a more objective reading of results, avoiding interpretation errors, thus reducing a subjective appreciation of the quality of results obtained in research and clinical practice.[26-27] Systematic literature reviews on the Metric properties of the instruments applied in practice allow to verify the scientific evidence and confirm that the instrument is valid, reliable and responsive.
The results of this systematic review show that the TUG version in Brazil[23] and Australia,[20] according to Sousa et al.,[27] has excellent levels of reliability, ICC> 0.90. Only the Australian version assesses the intra-observer reliability (Test-Retest) and is excellent.[24,27]
The inter-observer reliability is evaluated in the Brazilian[23] and US[21] versions, while the US version presents weak to very weak reliability values (0.77 <r <0.86). Intra-observer reliability is assessed only in the Brazilian version,[23] proving to be excellent (0.75 <ICC <0.96).[26]
The discriminative validity is only mentioned in the Brazilian version,[19] where it was concluded that the TUG is able to discriminate intra-groups, but not inter-groups. In a study comparing people with and without hemiparesis also found no differences, however the differences were found when comparing people with and without fear of falling.[28] In a study of people after stroke, they concluded that 69.8% of people had fear of falling as measured by the Fall Efficacy Scale-International,[29] and as fear of falling affects performance on the TUG[28] programs that improve balance are recommended and gait parameters in people with stroke as well as fear of falling.[30-31]
Criterion validity was addressed in Brazil[19] and Australia[20] versions, where the predictive value of TUG is confirmed. In the Brazilian version[19], the TUG allowed grouping individuals according to time, while in the study from Australia,[20] the predictive validity is addressed by associating the TUG with other variables. There was a correlation between the total time of the TUG and all the Kinect-TUG variables in the Australia version, with the exception of trunk flexion, according to Sousa et al.[27] and the step length considered good (p=0, 70) [26]. Both studies have adequate criterion validity (accuracy).[26] Sensitivity to TUG change was addressed in the study from Sweden[22] and Australia.[20] In the Swedish study,[22] the TUG makes it possible to detect changes from one assessment to another, although not always significant, only the younger ones always change, but not in the older ones. This study used different statistical methods, one used non-parametric statistics and the other linear regression, not allowing comparisons and determining whether there is strong evidence about the response to change. The results of this study cannot be extrapolated to people with recurrent stroke, as people were only selected after the first stroke. In the Australian version,[20] the Effect Size was addressed, but it does not present significant statistical values that allow us to know the responsiveness to the TUG change.
Some selected studies [19,21,23] in this systematic review have small samples, being referred to as a limitation by the studies themselves. According to Sousa et al.,[24] a sample with n <100 is considered poor.
Another limitation mentioned by the studies is the need to introduce other variables in future studies, such as speed, muscle strength, balance, extensor muscle strength, trunk flexion,[19-20] in order to improve the predictive value of TUG.
Two studies[19,21] refer to the need for further investigations, taking into account the limitations found, in a practical way to increase the level of evidence. With regard to the practical implications, it is recommended that professionals receive adequate training in the application of the instrument, in order to guarantee the reliability of the results obtained. It is still necessary to better understand the discriminating characteristics of people with stroke, with better performance in TUG compared to healthy people.
In summary, the TUG test-retest values and the inter-observer evaluation showed that this instrument is reliable and reproducible. It has validity and is sensitive to short-term changes after stroke. The heterogeneity of the included studies makes it difficult to draw precise conclusions regarding the psychometric properties of TUG.
Practical implications
TUG is a recommended test to predict the risk of falling.[19,28] People with stroke who have poor TUG performance level, with longer times since stroke onset and right hemisphere injury are at higher risk of fall and the TUG cutoff points for predicting fall vary by cerebral hemisphere, meaning, 13 seconds for the right hemisphere and 28 seconds for the left hemisphere.[32]
TUG can be used to predict performance on motor tasks and the bearing point is 13.49 seconds.[33]
CONCLUSION
Only five studies that studied the metric properties of the TUG in people with stroke in the community were included; however we can conclude that the TUG is a reliable intraobserver and interobserver instrument, valid and with some limitation in the responsiveness to change (responsiveness).
It is recommended that more studies be carried out in order to verify the sensitivity to change of this test in the person after a stroke.
Although the population samples are small, it allows us to verify that this assessment is transversal to different cultures; however, it will be important to carry out the TUG adapted to the Portuguese reality, taking into account the specific characteristics of this population.
REFERÊNCIAS
1 World Health Organization. Stroke, Cerebrovascular accident. Health topics. 2016. Disponível em: http://www.who.int/topics/cerebrovascular_accident/en/ [ Links ]
2 Marques-Vieira C, Sousa L, Braga R. Reabilitar a pessoa com Acidente Vascular Cerebral. In C. Marques-Vieira; L. Sousa (Eds). Cuidados de Enfermagem de Reabilitação à Pessoa ao Longo da Vida. Loures: Lusodidata. 2017: 465-474. [ Links ]
3 Silva IF, Neves CF, Vilela AC, Bastos LM, Henriques MI. Viver e Cuidar Após o Acidente Vascular Cerebral. Referência. 2016 Mar; IV(8):103-11. Disponível em http://www.scielo.mec.pt/scielo.php?script=sci_arttext&pid=S0874-02832016000100012 [ Links ]
4 World Health Organization . International Classification of Functioning,Disability and Health.Geneva:WorldHealthOrganization.2001Availablein http://apps.who.int/gb/archive/pdf_files/WHA54/ea54r21.pdf?ua=1 [ Links ]
5 Lewek MD, Bradley CE, Wutzke CJ, Zinder SM. The relationship between spatiotemporal gait asymmetry and balance in individuals with chronic stroke. J Appl Biomech. 2014 Feb 1;30(1):316.Available in http://journals.humankinetics.com/doi/10.1123/jab.2012-0208 [ Links ]
6 Trindade AP, Barboza MA, Oliveira FB, Borges AP. Influência da simetria e transferência de peso nos aspectos motores após acidente vascular cerebral. Rev Neurocienc. 2011;19(1): 61-7. [ Links ]
7 Silva JM, Hasse HK, Yussef SM, Kaminski EL. Efeitos da dupla tarefa com demanda motora e demanda cognitiva na marcha de sujeitos hemiparéticos pós AVC. Rev Neurocienc. 2015;23(1):48-54. Disponível em http://www.revistaneurociencias.com.br/edicoes/2015/2301/original/936original.pdf [ Links ]
8 Ordem dos Enfermeiros, Conselho de Enfermagem Rede Nacional de Cuidados Continuados Integrados:Referencialdoenfermeiro.Março2009.Disponívelem http://www.ordemenfermeiros.pt/documentosoficiais/documents/rncci%20%20v.final%20referencial%20do%20enfermeiro%20-%20abril%202009.pdf [ Links ]
9 Matter,C,Rugnaff,P.Lafonctioninfirmièreenrééducation-réadaptation.Soins. 2006;711:61.Disponible http://www.airr.eu/docs/711-Matter.pdf [ Links ]
10 Leclair, F. Proposition d'un atelier équilibre chez le patient hémiplégique post AVC: Etude auprès de 4 cas Cliniques. Institute de Formation Régional Aux Métiers De La Rééducation et Rééadaptation. 2012. [ Links ]
11 Bertrand AM, Howald A, Siegenthaler J, Kühne N. Utilisation d'instruments de mesure avec des personnes ayant subi un accident vasculaire cérébral: une enquête par questionnaire auprès d'ergothérapeutes en Suisse romande. Revue Francophone de Recherche en Ergothérapie. 2015 Jan 25;1(1):43-61. [ Links ]
12 Woellner SS, Araújo AG, Cabral FM, Uessler PN, Soares AV. Testes de equilíbrio em pacientes hemiparéticos por AVC. Neurociências. 2015;11(1):32-40. Disponível em http://www.ace.br/documentos/fisioterapia/2015/artigo_testes_de_equilibro_2015.pdf [ Links ]
13 Hafsteinsdóttir TB, Rensink M, Schuurmans M. Clinimetric properties of the Timed Up and Go Test for patients with stroke: a systematic review. Top Stroke Rehabil. 2014 May 1;21(3):197-210. [ Links ]
14 Bettany-Saltikov J. How to do a systematic literature review in nursing: a step-by-step guide. New York: Open University press; 2012. [ Links ]
15 Green S, Higgins JPT, Alderson P, Clarke M, Mulrow CD, Oxman AD. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 updated March 2011[Internet]. Melbourne: TheCochraneCollaboration;2011[cited2010Sept01].Available from: http://handbook.cochrane.org/ [ Links ]
16 Joanna Briggs Institute (2011). Joanna Briggs Institue's user manual: version5.0 system for the unified management. Assessment and Review of Information. Adelaide: The Joanna Briggs Institute. 2011. Available in http://www.joannabriggs.org/assets/docs/sumari/SUMARI-V5-Userguide.pdf [ Links ]
17 Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA). Welcome to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). 2015. Disponível em http://www.prisma-statement.org/ [ Links ]
18 Registered Nurses'Association of Ontario. Falls prevention: building the foundations for the patient safety. A self-learning package. Toronto: Registered Nurses' Association of Ontario. 2007 Available in http://rnao.ca/sites/rnao-ca/files/Falls_Prevention_-_Building_the_Foundations_for_Patient_Safety._A_Self_Learning_Package.pdf [ Links ]
19 Faria CD, Teixeira-Salmela LF, Nadeau S. Predicting levels of basic functional mobility, as assessed by the Timed "Up and Go" test, for individuals with stroke: discriminant analyses. Disabil Rehabil.2013Jan1;35(2):146-52. Available in http://www.tandfonline.com/doi/abs/10.3109/09638288.2012.690497 [ Links ]
20 Vernon S, Paterson K, Bower K, McGinley J, Miller K, Pua YH, Clark RA. Quantifying individual components of the timed up and go using the kinect in people living with stroke. Neurorehabilitation Neural Repair. 2015;29(1):48-53. Available in http://journals.sagepub.com/doi/abs/10.1177/1545968314529475 [ Links ]
21 Murphy K, Lowe S. Improving fall risk assessment in home care: interdisciplinary use of the Timed Up and Go (TUG). Home Healthc Now. 2013 Jul 1;31(7):389-96. Available in http://journals.lww.com/homehealthcarenurseonline/Fulltext/2013/07000/Improving_Fall_Risk_Ass essment_in_Home_Care_.7.aspx?trendmd-shared=0 [ Links ]
22 Persson CU, Danielsson A, Sunnerhagen KS, Grimby-Ekman A, Hansson PO. Timed Up & Go as a measure for longitudinal change in mobility after stroke-Postural Stroke Study in Gothenburg (POSTGOT). J. Neuroengineering Rehabil. 2014;11:83. [ Links ]
23 Faria CD, Teixeira-Salmela LF, Neto MG, Rodrigues-de-Paula F. Performance-based tests in subjects with stroke: outcome scores, reliability and measurement errors. Clin Rehabil. 2012 May 1;26(5):460-9. [ Links ]
24 Sousa LM, Marques-Vieira C, Carvalho ML, Veludo F, José HM. Fidelidade e validade na construção e adequação de instrumentos de medida. Enformação. 2015;5:25-32.Disponível em http://hdl.handle.net/10884/1016 [ Links ]
25 Dutra MC, Cabral AL, de Azevedo Carvalho G. Tradução para o português e validação do Teste Timed up and Go. Revista Interfaces, Saúde, Humanas e Tecnologia. Revista Interfaces: Saúde, Humanas e Tecnologia. 2016 Apr 22;3(9):81-88. DOI: 10.16891/2317-434X.430. Disponível em http://interfaces.leaosampaio.edu.br/index.php/revista-interfaces/article/view/242/pdf [ Links ]
26 Sousa LM. As propriedades psicométricas dos instrumentos de hétero-avaliação. Enformação. 2015;6:20-4. Disponível em http://hdl.handle.net/10884/998 [ Links ]
27 Sousa LM, Marques-Vieira C, Severino S, Caldeira S. Propriedades psicométricas de instrumentos de avaliação para a investigação e prática dos enfermeiros de reabilitação. In C. Marques-Vieira, L. Sousa (Eds). Cuidados de Enfermagem de Reabilitação à Pessoa ao Longo da Vida. Loures: Lusodidacta. 2017:113-122. [ Links ]
28 Danielli Coelho de Morais Faria C, Fuscaldi Teixeira-Salmela L, Nadeau S. Effects of the direction of turning on the timed up & go test with stroke subjects. Top Stroke Rehabil. 2009 May 1;16(3):196-206. [ Links ]
29 Khan S, Hadian MR, Olyaei G, Arslan SA, Yekaninejad S, Tafakhori A. Comparing Falls Efficacy Scale-International and Berg Balance Scale in Predicting Recurrent Risk of Fall in Stroke Patients. J Modern Rehabil. 2017 Apr 1;11(2):103-8. [ Links ]
30 Ordahan B, Karahan AY, Basaran A, Turkoglu G, Kucuksarac S, Cubukcu M, Tekin L, AD P, Kuran B. Impact of exercises administered to stroke patients with balance trainer on rehabilitation results: a randomized controlled study. Hippokratia. 2015;19(2):125-30. [ Links ]
31 Jung Y, Lee K, Shin S, Lee W. Effects of a multifactorial fall prevention program on balance, gait, and fear of falling in post-stroke inpatients. J Phys Ther Sci. 2015;27(6):1865-8. [ Links ]
32 Pinto EB, Nascimento C, Marinho C, Oliveira I, Monteiro M, Castro M, Myllane-Fernandes P, Ventura LM, Maso I. Risk Factors Associated With Falls in Adult Patients After Stroke Living in the Community: Baseline Data From a Stroke Cohort in Brazil. Top Stroke Rehabil.2014;21(1):220-7. [ Links ]
33 Chan PP, Tou JI, Mimi MT, Ng SS. Reliability and Validity of the Timed Up and Go Test With a Motor Task in People With Chronic Stroke. Arch Phys Med Rehabil. 2017 Nov 1;98(11):2213-20. [ Links ]
Received: May 24, 2018; Accepted: June 20, 2018; Published: June 23, 2018











 text in
text in