Introduction
The novel coronavirus 2019 (COVID-19) was first reported in Wuhan, China in December 2019.1 Since then, it has spread worldwide, with the World Health Organization (WHO) classifying it as a public health emergency on January 30th, 2020.2
On the 2nd of March, the first Portuguese cases were reported in Porto.3 After six days, it was reported the first two cases in Centro Hospitalar Universitário Lisboa-Norte.4 On March 11th, due to the rapid worldwide spread of the virus, the WHO classification changed and rated it as a pandemic.5
Due to this rapidly evolving situation, many health systems across the globe were put under great pressure to manage those patients.6 Like many countries around the world, the Portuguese government declared a lockdown policy on 18th March 2020 imposing quarantine and travel restrictions to mitigate the spread of the infection.7-9 Still, to avoid the collapse of the Portuguese healthcare system and to minimize the risk of spreading the infection, based on the experience of other countries, structural and organizational changes were adopted in our hospital.10-15
Due to the profound impact of the pandemic on social activities and the restructuring of the healthcare system, although not directly involved in the treatment of COVID-19 patients, the department of orthopedic and traumatology surgery had their activities conditioned.
Until now, there are no reports on the literature regarding the impact of the COVID-19 pandemic on the surgical treatment of orthopedic trauma in Portugal and the reports on the international literature are scarce and do not evaluate the impact of the pandemic on global orthopedic trauma.
This is the first paper analyzing this matter in a tertiary hospital in Portugal.
Material and Methods
Based on the electronic registry of our institution, we searched all patients with acute orthopedic trauma events admitted for orthopedic surgical treatment between 8 March 2019-31 December 2019 (non-pandemic group - group A) and 8 March 2020-31 December 2020 (pandemic group - group B). Exclusion criteria were: delayed union or non-union fractures, pathologic fractures, re-interventions, osteoporotic fractures without a history of trauma, knee meniscal or ligament injuries, rotator cuff tears, shoulder instability procedures, and ligamentous injuries of any joint.
Age, gender, injury mechanism, fracture distribution, surgical procedure, rate of positive conversion on patients initially admitted as COVID-19 negative, death rate, and need for admission on ICU were registered and compared between the two groups. Furthermore, the time intervals between diagnosis and surgery (“time to surgery”), between diagnosis and discharge during hospital stay (“time to discharge”), and between clinical discharge and social discharge (“time to social discharge”) were also analyzed.
Firstly, a comparative analysis was performed between patients treated in 2019 (group A) and 2020 (group B). Subsequently, a new descriptive analysis of group B was performed, comparing the values between patients infected with the COVID-19 virus (group B1) and non-infected patients (group B2). The data concerning the patients submitted to surgical treatment due to hip fractures were also analyzed separately.
Statistical analyses were performed using Statistical Package for the Social Sciences version 26.0 (SPSS Inc. Chicago. IL. USA). Statistical significance was set at p<0.05. Unpaired Student’s t-test was used to compare continuous variables, and results reported as t (degrees of freedom), p-value. Contingency tables with Chi-square test calculation were used to compare categorical variable distribution between groups.
Results
A total of 1522 patients were included in the study, 794 patients in 2019 and 728 in 2020. The mean age for groups A and B were 64.14±25.06 years and 64.05±24.9, respectively - p=0.399 (Table 1).
When evaluating the mechanism of traumatic injury there was a statistically significant difference between groups (p=0.001) (Table 2). In both years, the mechanism of injury most often identified was “fall from standing height”, with a decrease in its incidence from 68.4% to 44.5% from 2019 to 2020. There was an increase in the incidence of "falls from height" from 5.4% to 9.2% from 2019 to 2020, and a higher incidence of motorcycle accidents in the pandemic year compared to the previous year (6.9% versus 4.0%). There was also a significant decrease in the percentage of patients sustaining simple blunt trauma from 8.2% in 2019 to 3.0% in 2020. Although with no statistical significance, it was identified intended suicidal attempts in more patients in 2020 (1.6%), compared to 2019 (1.0%).
The number of polytrauma patients in Group A was 71 (8.9%) and 106 (14.6%) in Group B (p<0.001).
Interestingly, although the mean time to surgery was significantly shorter in the pandemic group (4.83 vs 5.55 days, p=0.003), the hospital stay was longer in this group (14.73 vs 12.01 days, p=0.002). There was no difference in terms of time to resolution of the social situation (3.93 vs 2.96, p=0.084) between the two groups.
The mortality rate was 1.9% in both years (p=0.961). There was also no statistical difference between the number of patients needing ICU care between 2019 and 2020 (p=0.514).
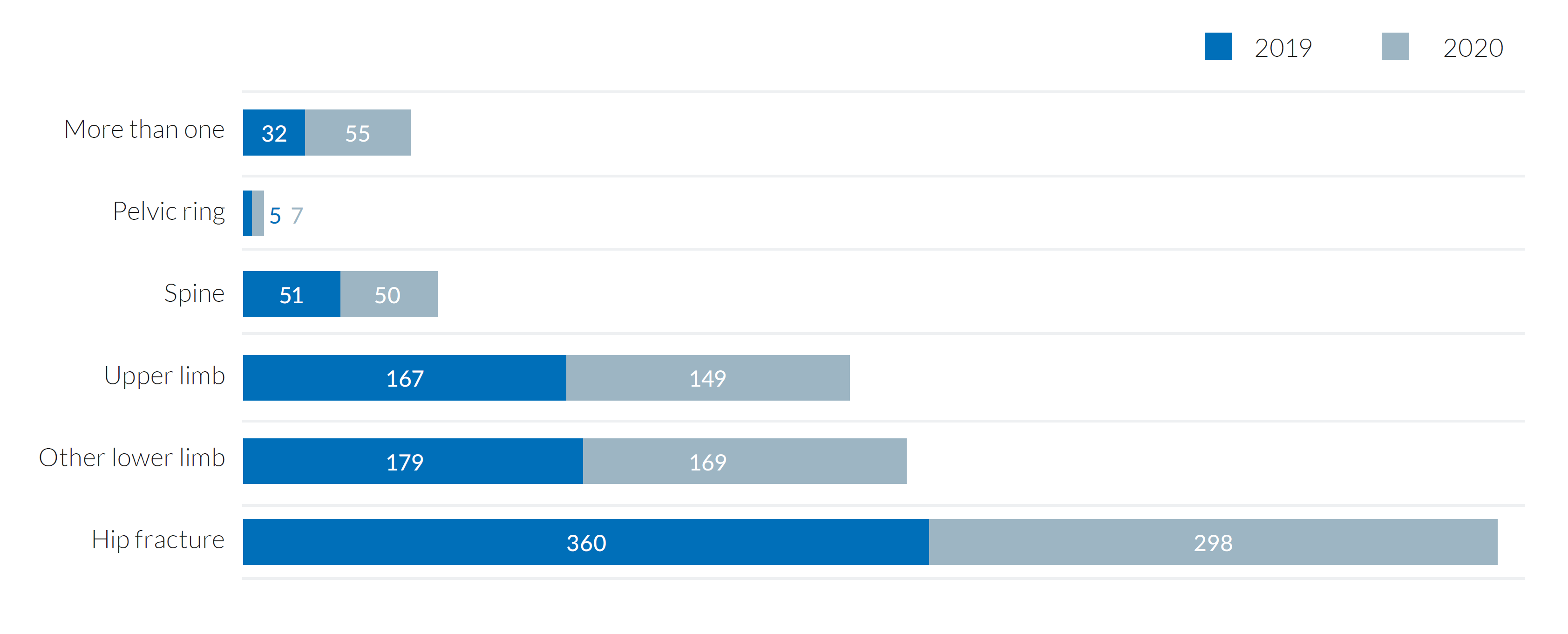
There was no difference in the anatomical distribution of the fractures, p=0.057 (Fig. 1). Hip fracture was the most common diagnosis, with 658 cases diagnosed, 360 in 2019 and 298 in 2020 (Table 3). The mean age of these patients was 81.06±12.76 years in group A and 82.79±10.32 years in group B. The mean time to surgery was 5.75±3.91 days for the first group and 4.38±3.29 days for the pandemic group. The mean hospital stay was 13.48±8.47 days in 2019 and 15.04±12.39 days in 2020. The mean time to social discharge was 6.75±16.21 days for the first group and 5.22±11.07 days for the pandemic group. There was no statistically significant difference between both groups for all these parameters, except for the time to surgery (p=0.018), which was shorter in the pandemic year.
Only 3 hip fracture patients were diagnosed as COVID-19 positive. The mean age for these patients was 90.00±7.00 years, while it was 82.80±10.14 for the COVID-19 negative group. The mean time until surgery was 8.67±6.66 days for the COVID-19 positive group and 4.29±3.14 for the COVID-19 negative group. The mean hospital stay was 22.33±11.06 days in the COVID-19 positive group against 15.19±12.64.
From the initial poll of 728 patients treated in the pandemic year, only 8 tested positive for SARS-CoV-2 (Group B1). The mean age for group B1 was 48.00±36.15 years and 63.52±24.82 for group B2 (COVID-19 negative patients). Time to surgery was 5.75±5.75 days in group B1 and 4.75±5.09 days in group B2. The duration of the hospital stay was 18.63±9.53 days in group B1 and 14.55±16.75 days in group B2. From a statistical point of view, it was not possible to assess the significance of these values, given the discrepancy between the number of patients in the two groups.
No patient admitted with a negative swab turned positive in any of the following tests for SARS-CoV-2 during the hospital stay.
Table 1: Demographic and clinical data of the population.
| 2019 | 2020 | p-value | |
|---|---|---|---|
| Mean age (years) | 63.91±25.062 | 63.05±24.966 | 0.399 |
| Female versus Male (n, %) | 467 vs 327 (58.8% vs 41.2%) | 402 vs 325 (55.3% vs 44.7%) | 0.166 |
| Time to surgery (days) | 5.55±4.547 | 4.83±5.234 | 0.003 |
| Time to clinical discharge (days) | 12.01±14.969 | 14.73±18.223 | 0.002 |
| Time to social discharge (days) | 3.93±13.026 | 2.96±8.324 | 0.084 |
| Mortality (n, %) | 15 (1.9%) | 14 (1.9%) | 0.961 |
| ICU stay (n, %) | 58 (7.3%) | 47 (6.5%) | 0.514 |
Demographic and clinical data for the patients treated in 2019 and 2020 are shown in the present table with the p-value for each parameter analysed presented on the right column.
Table 2: Mechanism of injury of the patients treated in both years.
| 2019 | 2020 | ||||
|---|---|---|---|---|---|
| N | % | N | % | Sig. | |
| Injury Mechanism | 0.001 | ||||
| Suicidal attempt | 8 | 1.0 | 12 | 1.6 | |
| Fall from standing height | 543 | 68. | 435 | 44.5 | |
| Fall from height | 43 | 5.4 | 67 | 9.2 | |
| Car accident | 37 | 4.7 | 35 | 4.8 | |
| Motorcycle accident | 32 | 4.0 | 50 | 6.9 | |
| Run over | 29 | 3.7 | 30 | 4.1 | |
| Sports injury | 30 | 3.8 | 37 | 5.1 | |
| Assault | 2 | 0.3 | 4 | 0.5 | |
| Crush injury | 1 | 0.1 | 2 | 0.3 | |
| Simple blunt trauma | 65 | 8.2 | 22 | 3.0 | |
| Open injury | 2 | 0.3 | 2 | 0.3 | |
| Unknown | 2 | 0.3 | 33 | 4.5 | |
Cramer’s V=0.214. In bold you may find the injury mechanism with a statistically significance between group A and B, according to the adjusted residual.
Table 3: Demographic and clinical data of patients with hip fractures.
| 2019 | 2020 | p-value | |
|---|---|---|---|
| Mean age (years) | 81.06±12.76 | 82.79±10.32 | 0.060 |
| Female versus Male (n, %) | 267 vs 93 (74.2% vs 25.8%) | 226 vs 72 (75.8%vs 24.2%) | 0.622 |
| Time to surgery | 5.75±3.91 | 4.38±3.29 | 0.018 |
| Time to clinical discharge | 13.48±8.47 | 15.04±12.39 | 0.065 |
| Time to social discharge | 6.75±16.21 | 5.22±11.07 | 0.170 |
| Mortality (n, %) | 8 (2.2%) | 8 (2.7%) | 0.702 |
| ICU stay (n, %) | 10 (2.8%) | 4 (1.3%) | 0.204 |
Demographic and clinical data for the patients sustaining hip fractures treated in 2019 and 2020 are shown in the present table with the p-value for each parameter analysed presented on the right column.
Discussion
Since coronavirus spread throughout the world, countries took measures to minimize the impact of the pandemic on the social, financial, and healthcare systems. This led to a profound impact on our daily life activities.
In the literature, several studies are reporting the impact of the pandemic on medical activity. Orthopedic departments from all around the world had their elective surgical activities profoundly limited. However, the impact on trauma surgery is not as well documented. For this matter, we aimed to provide an evaluation of the impact of the pandemic in the trauma activity in a tertiary hospital in Portugal.
In our department, there was only an 8.31% decrease in the number of patients submitted to orthopedic surgery due to trauma from 2019 to 2020. On the contrary, a significant number of studies in the literature report a decrease in trauma surgery by 21.2% to 66.7% around the globe.16-26 In fact, according to data published by the Ministry of Internal Administration and the Portuguese Road Safety Authority, the number of road traffic accidents with victims in Portugal decreased by 26.8% from 2019 to 2020.27 When compared to the current literature, the decrease in trauma surgery in our institution in 2020 is less pronounced. For this reason, it might have contributed the fact that our institution is a Level 1 trauma centre in Portugal, and during that time most of the accidents were probably brought to our emergency department, centralizing the traumatology activity of the region.
Most countries have implemented several lockdown measures to slow the spread of COVID-19 and to avoid healthcare system collapse.8 Consequently, the number of traffic accidents decreased in many countries.8,16,21,27-30 On the contrary, in our study, we report an increase in the incidence of motorcycle accidents (4.0% to 6.9%) and maintenance in the percentage of car accidents registered (Table 2). Such could be explained by the exponential growth in the food delivery services during the pandemic year and the centralization of the trauma referral into our institution. However, most of the studies reporting traffic accidents in the literature are referred to global emergency department assistance and not only to patients submitted to surgery. We report a considerable increase in the number of patients sustaining surgical injuries from falls from height (n=43 to n=67) that once more can be explained because of the status of polytrauma centre of our hospital, receiving the majority of trauma and polytrauma patients in this particular period. We also noticed a significantly increased incidence of polytrauma patients, from 71(8.95%) in 2019 to 106(14.56%) in 2020, that might have not been verified in other national and international orthopedic departments.
As reported by Carlin et al, the number of patients admitted to our institution following an intentional traumatic injury due to a suicide attempt increased from 8 patients in 2019 to 12 patients in 2020.31 Although not statistically significant this is an important subject to address. Undoubtedly, COVID-19 lockdown might have increased the incidence of depression and anxiety symptoms due to the economic and social consequences of the isolation and the restrictions on social activities.32-34
On the other side, low-energy trauma decreased. In fact, there was a reduction in the incidence of fractures resulting from simple falls from standing height from 68.4% to 44.5% and a reduction from 8.2% to 3.0% of simple blunt trauma to the upper and lower limbs. At last, although team sports were greatly limited in our country, we did not notice a decrease in the incidence of sports injuries, contrary to literature.16 Most of these accidents were related to road cycling, as individual sports were allowed during this period.
As reported by Brayda-Bruno et al, the time interval between diagnosis and surgery was significantly shorter in the pandemic group (5.55 days in 2019 and 4.83 days in 2020).6 The main reason for this was the cancellation of all elective surgery, besides oncological surgery, which reallocated all the orthopedic department activities to treat acute and urgent trauma. Nevertheless, there is a potential to improve these results.
Our results, related to the time of hospital stay and social discharge, are different from the literature, with a longer time to clinical discharge but no difference in the time to social discharge.6 These results might be explained by the increased number of polytrauma patients treated in our institution that requested longer hospital care.
Regarding the anatomical area of the lesions, there was no difference between 2019 and 2020. Since hip fracture in the elderly was the most frequent diagnosis, it is important to evaluate the possible influence of the pandemic in the treatment of this entity separately. As reported in the literature, these fractures were treated earlier in our institution in the pandemic year.6 Nonetheless, there is still no protocol established between the orthopedics and internal medicine departments for the treatment of these fractures in the first 48 hours, as advised in the literature.35
Although being a small proportion of the sample, the three COVID-19 positive patients with hip fracture were older and had longer time until surgery and hospital stay compared to COVID-19 negative patients. These results may reflect the difficulties in the logistics regarding the surgical procedure and the postoperative support for patients in our institution, which might need to be revised. In fact, during this period, surgeries of COVID-positive patients took place in a secluded operating room, without clear and individualized circuits for patients and hospital staff, which made the availability of adequate surgical instruments and personal protective equipment difficult during the procedures.
Based on the descriptive analyses of the patients treated in the pandemic year, we reported that COVID-19 positive patients were older, had longer time to surgery and longer hospital stay by 7 days. Although there is no reported information across the literature regarding the time until surgery and hospital stay, we highlight the difficulties in the logistics that we may face when treating these patients. With longer hospital stays, we can expect more medical complications and higher costs. There is a need for all the institutions around the globe to share their institutional protocols and results, to mitigate the impact of the pandemic in the health care system.
Overall, we had no cases of COVID-19 negative patients turning positive during hospitalization in the ‘clean’ area, which was an excellent outcome. COVID-19 spread among hospitalized patients was one of the most severe issues to manage during the first Italian outbreak as reported, which led our institution to adopt measures in this area.36 During the pandemic year, wards were re-designed to accommodate the COVID-positive patients separately. No family visits were allowed during the hospital stay and all patients were tested at admittance and whenever symptoms of a possible COVID-19 infection were detected. This protocol was gradually changed to an “every seven days” testing protocol for all patients during their hospital stay.
Conclusion
The influence of the pandemic has been noted in the most varied medical specialties. Although not being a front-line specialty in combating the pandemic, the orthopedic and traumatology surgery departments had their activities profoundly conditioned by the governmental measures implemented. During the pandemic year, there was a 26.8% decrease in the national number of road traffic accidents with victims when compared to the previous year. Nevertheless, we reported a 5% increase in the number of polytrauma patients treated in our institution, probably explained by the centralization of these patients to our trauma centre. We also report a shorter time to surgery, but longer hospital stays in 2020, which is probably due to the increasing number of polytrauma patients treated in the institution.
Even though there was no difference in the mortality between the pandemic and the previous year, with the growing number of COVID-19 cases, that carried longer hospital stays, it is mandatory to adopt safe and effective measures to reduce the clinical and economic burden of this pandemic.