Immunotherapy data on R/M HNSCC
Head and neck squamous cell carcinoma (HNSCC), can be potentially cured if diagnosed at early stages and adequately treated.
Still, most patients are diagnosed at stages III or IV disease, with estimated local and distant failure rates of 60% and 30%, respectively, notwithstanding aggressive multimodality curative intent treatment strategies approved.1-3
The excellent results of the EXTREME trial published in 20084 showing a median overall survival (mOS), of 10.1 months for patients with recurrent and/or metastatic (R/M) HNSCC, treated with platinum plus fluorouracil (5FU) and cetuximab, changed the standard of care (SOC), for these patients. The EXTREME regime was the only to evidence an OS benefit before the immunotherapy era.1,4,5
HNSCC is considered an immunogenic tumor,5 partly because of its high mutational burden, being a good candidate for immunotherapy, either by immune blockade suppression or immune response stimulation. Increasing research efforts over the last decade have expanded immunotherapy options for HNSCC, bringing them closer to those available for other tumor types, such as malignant melanoma, lung cancer, and kidney cancer.
A. Treatment of platinum-resistant R/M HNSCC
Nivolumab was the first immunotherapy drug with proven results in a phase III trial of R/M HNSCC. Promising pre-clinical and phase I and II clinical trial results led to the phase III CheckMate 141 (CM 141) trial,6 which enrolled 361 patients with R/M HNSCC progressing within 6 months after platinum-based chemotherapy.
CM 141 achieved a median overall survival (mOS) of 7.5 months for nivolumab versus 5.1 months for the control group, with an estimated 1-year survival rate approximately 19% higher for nivolumab (36.0% vs 16.6%). This was relevant, given the historical mOS of less than 6 months for patients with disease progression within 6 months of standard platinum-based therapy (Table 1).
Table 1: Characteristics and results of the 2 phase III trials on R/M SCHNC platinum resistant.
| Phase III trials | CM 141 | KN 040 |
|---|---|---|
| R/M SCHNC progressing during or after platinum-based chemotherapy | ≤ 6 months | Between 3 to 6 months of multimodal treatment if for locally advanced disease |
| Randomization | 2:1 | 1:1 |
| Standard therapy (comparator arm) | w methotrexate 40 to 60 mg/m2 iv w docetaxel 30 to 40 mg/ m2 iv Cetuximab loading dose 400 mg/m2 D1 >>250 mg/m2 w iv | w methotrexate 40 to 60 mg/m2 iv docetaxel 75 mg/m2 every 3 weeks iv cetuximab loading dose 400 mg/m2 D1 >> 250 mg/m2 w iv |
| Stratification | Receipt or not previous cetuximab therapy | ECOG / PS (0 vs 1) p16 status in the oropharynx (positive versus negative) PD-L1 tumour proportion score 50% vs <50%) |
| Primary endpoint | OS | OS |
| Secondary endpoints | Progression-free survival (PFS), Objective response rate (ORR), Safety, Patient-reported quality of life (QoL) | OS in the population with CPS ≥ 1 In all participants and those with a CPS ≥ 1 : safety; PFS; ORR; duration of confirmed response; time to progression. |
| mOS | Nivolumab 7.5 months (95% CI, 5.5−9.1) vs Control group 5.1 months (95% CI, 4.0−6.0) | Pembrolizumab 8·4 months (95% CI 6·4-9·4) vs Standard of care 6·9 months (5·9-8·0) (HR 0·80, 0·65-0·98; nominal p=0·0161) |
| Estimated 1-year survival rate | 36.0% vs 16.6% | NA |
| PFS rate at 6 months | 19.7% vs 9.9% | NA |
| ORR | 13.3% vs 5.8% | 14·6% vs 10·1% |
| Median time to response | 2.1 months vs 2.0 months | 4·5 months vs 2·2 months |
| TRAEs (treatment related adverse events) grade 3 or 4 | 13.1% vs 35.1% | 4 vs 19 (grades 3- 5) |
| Patient-reported QoL (QLQ-C30) and QLQ-H&N35) | Stable versus meaningfully worse | NA |
| Biomarker analysis (p16) for oropharynx | 90.6% patients | All |
| Tumor PD-L1 membrane expression | IHC testing (Dako North America) | IHC 22C3 pharmDx assay (Agilent Technologies, Carpinteria, CA, USA) |
| Score | TPS ≥1%, ≥5%, and ≥10%, in a minimum of 100 tumor cells | TPS ≥ 50% and CPS≥1 |
| Number of publications | 3 | 1 |
Other favorable outcomes in this trial included progression-free survival (PFS) rate at 6 months (19.7% vs 9.9%), overall response rate (ORR) (13.3% vs 5.8%), and grade 3 or 4 treatment-related adverse events (13.1% vs 35.1%). As previously described in the publication by Kevin J Harrington et al,7 patient-reported quality of life (QoL) also favored nivolumab, with stable QoL regarding physical, role, and social functioning with the anti-PD-1 compared with meaningfully worse with standard therapies.
Results at the 24-month follow-up (FU), were consistente with initial data: nivolumab nearly tripled the estimated OS rate (16.9%) compared with investigator choice (IC) treatment (6.0%).8 The safety profile observed for longterm survivors was also consistent with previous observations.
Although in this trial the OS and progression free survival (PFS) curves began to separate at 3 months, PFS results were worse before that time, fact consistent in the 24 months FU publication.6,8
The OS benefit was similar regardless of tumor PDL1 expression (≥1% or <1%) or human papillomavirus (HPV) status (positive or negative), although a trend was observed towards better outcomes for PD-L1 “expressors” and HPV-positive patients. However, as PDL1 expression and p16 status were not mandatory for screening and stratification in this trial, they were unknown for a large number of patients (86 and 175, respectively), analyzed in the study.
A total of 222 patients (150 in nivolumab and 72 in the standard-treatment arm) had previously received cetuximab, a stratification factor in CM 141 trial. These were probably patients who received the EXTREME protocol first, with the remaining actually in first-line treatment for R/M disease, after early progression following primary curative intent treatment with cisplatin and radiotherapy.
Overall, patients responded to nivolumab regardless of whether they received cetuximab before, but those who did not, responded better. This was also observed in the KEYNOTE 040 (KN 040) trial, which investigated the other immune checkpoint inhibitor pembrolizumab,9 although with a less pronounced difference. This is not surprising for those were patients actually in first line treatment for R/M disease, as mentioned before.
Pembrolizumab (formerly MK-3475 or lambrolizumab) was the other anti-PD-1 to be investigated in R/M HNSCC. The first relevant results with this agent came from the head and neck cohort of the KEYNOTE 012 (KN 012) phase 1b open-label, multicenter trial. This study evaluated the drug’s safety and clinical activity in the treatment of R/M HNSCC, with results published in July 2016 in the Lancet Oncology.10
KN 012 showed that pembrolizumab was well tolerated and had clinically relevant antitumor activity, leading to the accelerated approval by the Food and Drug Administration (FDA) of the anti-PD-1 for the treatment of R/M HNSCC patients with disease progression after or during platinum-based chemotherapy.
The phase III KN 040 was the confirmatory trial of KN 012. Trial results were presented at the ESMO 2017 Congress and subsequently published in 2018.9
KN 040 excluded patients who recurred or progressed within 3 months of previous platinum multimodal therapy for locally advanced disease. By excluding patients with rapidly progressive disease, a better patient selection was achieved, as referred in another publication.11
The OS for the group with PD-L1 tumor proportion score (TPS) ≥50% was clearly better for pembrolizumab compared with standard treatment since the first month of treatment, with a hazard ratio (HR) of 0.53 (95% CI 0.35-0.81; nominal p=0.0014). Pembrolizumab was also associated with longer PFS in the population with PD-L1 TPS of 50% (Table 1).
In the KN 040 trial, when disease progressed patients received subsequent therapy, which consisted of imune checkpoint inhibitors in 4% of pembrolizumab and 13% of SOC group. In the latter, patients who subsequently received an immune checkpoint inhibitor had a much better mOS than those who received other therapies or even no subsequent therapy (20.1 vs 9.7 vs 4.5 months, respectively).
While no crossover was planned in the KN 040 trial, in CM 141 the protocol was amended to allow patients in the IC arm to crossover to nivolumab arm at the time of disease progression. Another difference between CM 141 and KN 040 was that docetaxel, one of the comparators in standard of care (SOC) arm, chosen in a similar proportion of patients in both trials (approximately 45%), was used in different doses in each trial: weekly in CM 141 and each 21 days in KN 040. Previous data for various tumors indicate that lower weekly docetaxel doses are better tolerated but have lower efficacy than once-every-3-week doses.
This could also be one subject that makes difficult to compare data from the two trials, even if indirectly. The choice between the two immune checkpoint inhibitors for platinum resistance R/M HNSCC is therefore, difficult to establish if at all in clinical practice. If and when the two drugs are available in each country, the choice will fall in the experience of each clinician for they are both very similar in terms of efficacy and tolerability.
B. Treatment of platinum-sensitive R/M HNSCC
To our knowledge, KEYNOTE 048 (KN 048) was the only phase III trial to date to investigate the treatment of platinum-sensitive R/M HNSCC. In this trial, pembrolizumab, either in monotherapy or in association with a platinum chemotherapy backbone and 5FU, was compared with the SOC EXTREME protocol.12
In KN 048, PD-L1 positivity was not required for study entry, patients were stratified according to PD-L1 expression, p16 status, and performance status and randomized 1:1:1 to pembrolizumab alone, pembrolizumab plus platinum and 5FU, or the EXTREME protocol. Primary endpoints were OS and PFS in the intention-to-treat (ITT) population (Table 2).
Table 2: Results of KN 048 for primary endpoints, OS and PFS, at 1st, 2nd interim analysis, and final analysis.
| KN 048 | Pembrolizumab versus cetuximab plus CT | Pembrolizumab plus CT versus cetuximab plus CT |
|---|---|---|
| OS CPS ≥ 20 population | 14·9 months vs 10·7 months, HR 0·61 [95% CI 0·45-0·83], p=0·0007) | 14·7 vs 11·0, 0·60 [0·450·82], p=0·0004) |
| OS CPS ≥ 1 population | 12·3 vs 10·3 0·78 [0·64-0·96], p=0·0086) | 13·6 vs 10·4, 0·65 [0·53-0·80], p<0·0001) |
| OS Total population | 11·6 vs 10·7, 0·85 [0·71-1·03] | 13·0 months vs 10·7 months, HR 0·77 [95% CI 0·63-0·93], p=0·0034) |
| PFS CPS ≥ 20 population | (HR 0·99 [95% CI 0·75-1·29], p=0·4562) | HR 0·73 [95% CI 0·55-0·97], p=0·0162) |
| PFS CPS ≥ 1 population | HR 1·16 [95% CI 0·96-1·39]** | 0·82 [0·67-1·00]** |
| PFS Total population | 1·34 [1·13-1·59]** | HR 0·92 [95% CI 0·77-1·10], p=0·1697 |
**No formal statistical testing, because superiority was not met for the other comparisons for PFS. CT - chemotherapy
Study results showed that pembrolizumab monotherapy improved OS in patients with tumor PD-L1 combined positive score (CPS) ≥20 or ≥1 and had a non-inferior OS compared with SOC in the total study population. Pembrolizumab plus chemotherapy significantly improved OS compared with SOC in patients with tumor PD-L1 CPS ≥20 or ≥1 and in the total study population. Pembrolizumab alone was non-superior to cetuximab plus chemotherapy regarding PFS and objective response.Both endpoints showed similar results for pembrolizumab plus chemotherapy and cetuximab plus chemotherapy.
Compared with the EXTREME protocol, an inferior PFS was observed either with pembrolizumab alone or in combination with chemotherapy in the average first 6 months of treatment, but the median response duration was better with pembrolizumab plus chemotherapy compared with cetuximab plus chemotherapy (7.1 vs 4.2 months in the CPS ≥20 population; 6.7 vs 4.3 months in the CPS ≥1 population; 6.7 vs 4.3 months in the total population).
As expected, compared with the EXTREME regimen the incidence of any-grade or grade ≥3 adverse events was lower with pembrolizumab monotherapy and similar with pembrolizumab plus chemotherapy.
Pembrolizumab alone and pembrolizumab plus chemotherapy were associated with more complete responses and a longer response duration. Pembrolizumab alone improved median response duration by more than 16 months versus cetuximab with chemotherapy. For pembrolizumab monotherapy, greater PD-L1 expression was associated with greater response.
Based on these results, pembrolizumab plus platinum and 5FU was considered a suitable regimen for first-line treatment of R/M HNSCC, and pembrolizumab monotherapy a suitable first-line treatment for PD-L1-positive R/M HNSCC.
The European Medicines Agency (EMA) recommends the use of pembrolizumab as monotherapy or in combination with platinum and 5-fluorouracil (5-FU) chemotherapy, for the first-line treatment of R/M HNSCC in adults whose tumours express PD-L1 with a CPS ≥ 1, and as monotherapy for the treatment of R/M disease
in adults whose tumours express PD-L1 with a ≥ 50% tumor positive score (TPS) and progressing on or after platinum-containing chemotherapy.
Even so, the authors consider that can still exist a population candidate to the EXTREME protocol. Patients “fit” but symptomatic in the context of a great volume of disease, that need a rapid response and at the same time tolerate the association of platinum, 5FU and cetuximab could probably benefit from this treatment.
Another important aspect is the fact that the skill to determine CPS and TPS need to be acquired from each pathology departments to ensure an adequate selection of patients for treatment with pembrolizumab.
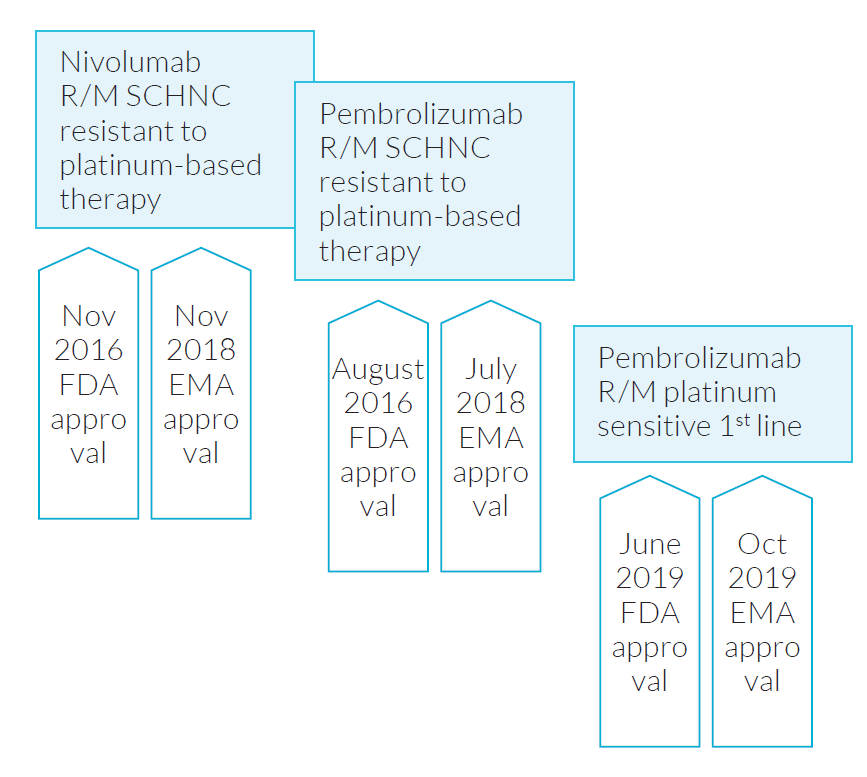
The sequence of authorization in the United States of America and in Europe for usage of these two imune checkpoint inhibitors are depicted in Fig. 1.
Conclusion
Keeping in mind that it is not legitimate to compare results of trials with different designs, immunotherapy clearly improves OS in patients with platinum-resistant disease, while preserving QoL. The same is not so straightforward in the platinum-sensitive setting.
It is acknowledged that R/M HNSCC patients who respond to IT have a good response, sustained for a longer period of time and with better tolerability than with standard therapies. However, it should be emphasized that some patients may respond worst in the first months of immunotherapy compared with standard therapies and consequently be seriously harmed by it.
Symptomatic patients and those with a high burden of disease requiring a rapid response will probably respond better with chemotherapy upfront. Whether chemotherapy should be combined with cetuximab or pembrolizumab remains unanswered. For example, testing for germline EGFR mutations could potentially help in this selection.
While the clinician must specify to the pathologist the PD-L1 score required to opt for pembrolizumab treatment, no pre-specified PD-L1 score is needed for nivolumab, demanding a tight interaction between specialists.
The human immune system is a complex and fascinating microsystem and its relation with tumor cells is far from total grasp. Consequently, much more needs to be understood to determine the best biomarker(s) for these treatments.
Other immune checkpoints are being tested in early phase clinical trials, for example TIM-3 (T cell immunoglobulin mucin receptor 3), LAG3 (lymphocyte-activation gene 3), TIGIT (T cell immunoreceptor with Ig and ITIM domains), that could bring more information and other means to stimulate and de block our immune system.13
Till now there are conflicting data regarding the relation between PD-1, and PD-L1 expression and HPV positivity. Some author refer that higher PD-1 expression in tumor-infiltrating lymphocytes (TILs) of HPV-positive tumours, could mean a strong immune response induced by HPV. Others report differently: high PD-1 levels in HPV-negative HNSCC. Immunosuppressive factors of microenvironment also probably will be important, such as Tregs.
For the time being, only a small proportion of HNSCC patients achieve longer disease control with immunotherapy than with previous therapies. Therefore, it is imperative to better identify patients potentially benefiting from new therapies in order to optimize the overall prognosis of this population.