The usual size of the peroneal tubercle is 3 mm.1 The size of the critical peroneal tubercle - borderline to promote tendon injury - is 4.3 mm on magnetic resonance imaging (MRI).1
It is supposed that most cases are congenital (flat or paralytic foot, equinus foot, insertion of the peroneus quartus muscle), but some are acquired by previous trauma, altered weight support, and/or inflammatory diseases related to spasms of the peroneus longus tendon.2 The portion of the peroneus longus tendon that is located between the fixed bony points of the peroneal tubercle and the cuboid may stretch unnaturally in the presence of a hypertrophied peroneal tubercle and, with sudden or repeated inversion movements, the tendon may rupture.3 The peroneus brevis tendon can collide between the tubercle and the lateral malleolus during the eversion-abduction movement of the foot, resulting in tenosynovitis, tendon laceration, and degeneration.1
The first symptoms occur when the peroneal hypertrophic tuber causes chronic irritation of the tendons and tendon sheaths, with the peroneus longus tendon being more vulnerable to damage than the peroneus brevis tendon owing to its length, sharp change of direction, and subsequent location to the peroneal tubercle.2 The typical finding on physical examination is edema in the lateral region adjacent to the calcaneal bone, focal tenderness over the peroneal tendons, and close to the peroneal tubercle, in addition to a positive peroneal tendon resistance test.1
A peroneal tubercle can be identified by an axial view of the calcaneus or anteroposterior radiographs of the ankle, while the size of the peroneal tubercle can be assessed by multidetector computed tomography and three-dimensional volume rendering.2 Ultrasound and MRI are the diagnostic methods indicated for the assessment of coexisting conditions of the peroneal tendons and their differential diagnoses.2 Furthermore, MRI can detect the hypertrophied peroneal tubercle edema that is induced by frictional peroneal tendon activity.1 The differential diagnosis of lateral ankle pain consists of injury to the lateral ankle ligaments, subluxation/dislocation of the peroneal tendons, peroneal tenosynovitis, and osteochondral lesions of the talus.2,3
The initial treatment is usually conservative, including shoe modifications, padding, bracing, and immobilization.2 However, of the lanyard to the systematic review of Lohrer et al,1 only one case was successful, and in other cases, surgical interventions are indicated, consisting of the removal of the hypertrophic peroneal tubercle and repair of the peroneal tendons.2,3
We report a 42-year-old male with pain in the lateral region of the hindfoot. Refers to worsening when walking for a long time. On physical examination, he presents pain in the eversion of the ankle and foot dorsiflexion, without functional limitation. He does not present edema but presents pain during palpation in the lateral region of the calcaneal bone.
Ultrasound detected echotexture alteration in the peroneal brevis tendon and mild liquid effusion adjacent to the peroneal tubercle (Fig. 1). MRI detected hypertrophy (0.6 mm) and significant edema of the peroneal tubercle (Fig. 2) with peroneal tenosynovitis (Fig. 3) and mild liquid effusion around the region of the skin marker. Those findings are compatible with tenosynovitis due to a hypertrophied peroneal tubercle induced by frictional peroneal tendon activity. The patient was referred to the orthopedics department for scheduled surgery.
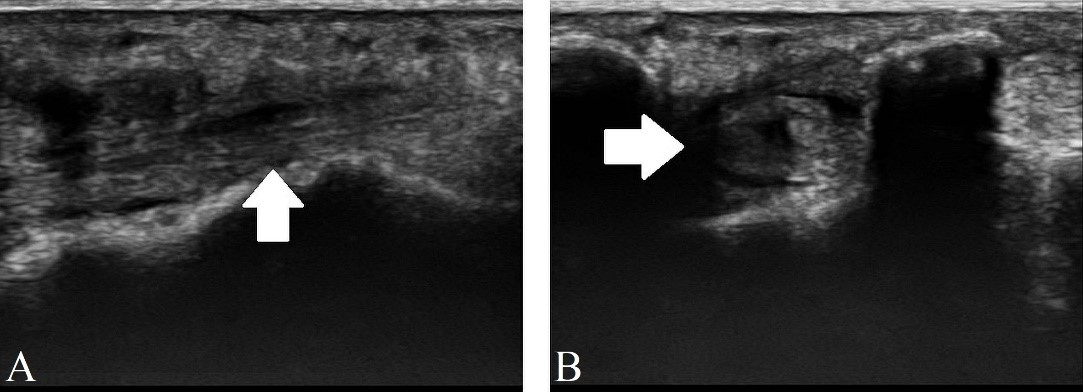
Figure 1: Ultrasound demonstrating tenosynovitis of the peroneal brevis (white arrow) in the sagittal section (A) and axial section (B).
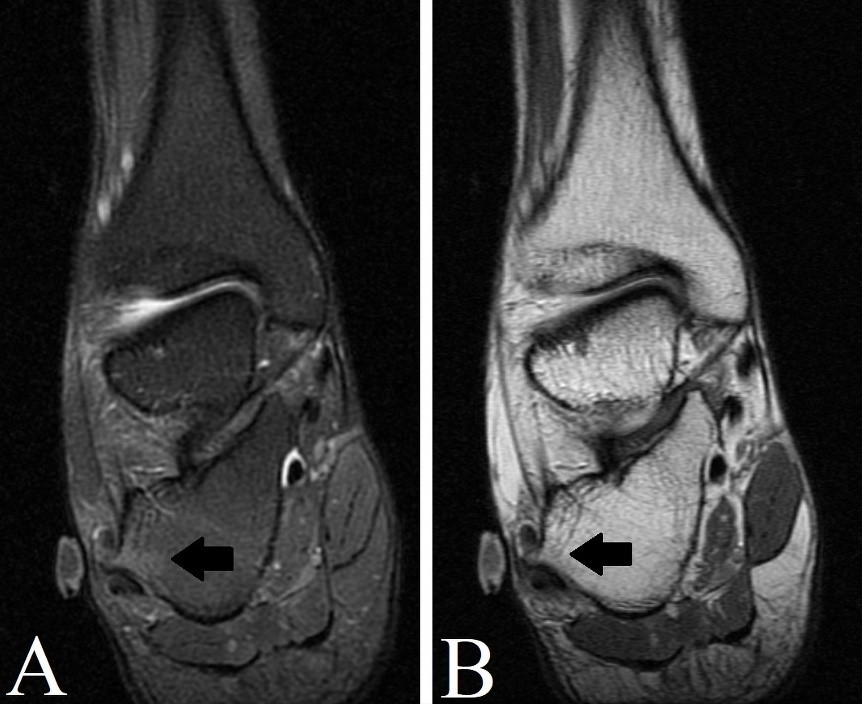
Figure 2: MRI in the coronal section of the right ankle, T2 FAT SAT weighted-image (A) and T2 weighted-image (B) demonstrating edema in the hypertrophied peroneal tubercle (black arrow).
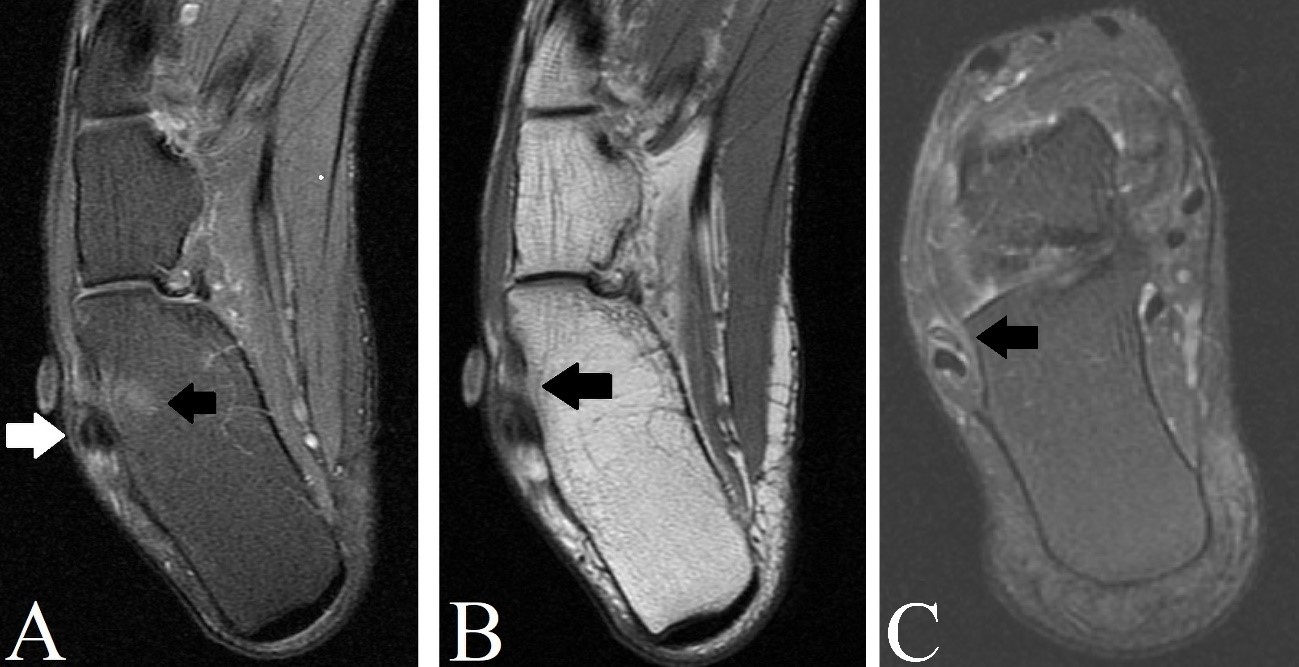
Figure 3: MRI in the axial section of the right ankle, T2 FAT SAT weighted-image (A) and DP weighted-image (B) demonstrating edema in the hypertrophied peroneal tubercle (black arrow) and tenosynovitis of the peroneal tendons (white arrow). In C, MRI in the oblique section of the right ankle in T2 FAT SAT weighted-image demonstrating marked tenosynovitis of the peroneal brevis tendon (black arrow).















