Challenges of teaching anatomy to medical students
The main challenges faced when teaching modern anatomy rely on the vast amount of information needed to be learned in face of the progressive reduction of dedicated anatomy teaching time over the last decades at medical universities. These challenges highlight the importance of optimizing the limited amount of time to teach and learn the essential and clinically relevant anatomy. Defining the essential or ground base anatomy concepts is also a matter of debate. More so, varied teaching methods to overcome these challenges have been proposed.1-15.Three different dimensions of learning have been identified: deep, superficial and strategic.1,3,15. Deep retention on knowledge relies on continued study with multiple resources and complementary information that allows consolidation of concepts and integration of information leading to long-lasting retention of knowledge. Superficial learning is based on memorization of concepts in a random and isolated manner, without integration and linkage of ideas, leading to short-lasting retention of knowledge. Strategic learning relies on evaluation-driven retention of knowledge.1-7,15) The first contact that medical students have with anatomy teaching could be a superficial one, to be consolidated in the following years. This sequential teaching of anatomy through the different years of medical school using different approaches and perspectives would allow a retention of knowledge, with integration of more information.2,8,15 This continued teaching of anatomy throughout medical school years would allow a more efficient learning with a vertical approach top-down, revisiting anatomy in the clinical years.1-11,15 This vertical teaching of anatomy would be based on different approaches: descriptive anatomy in the initial year, clinical and radiological anatomy in the second year, topographic and dissection anatomy in the last clinical years of medical school to foster deep acquisition of knowledge.4,5 The best way to teach anatomy is based on multiple teaching resources as dissected specimens, cadaveric dissection, 3D plastic models, radiological anatomy, and digital platforms (Figure 1). The goal of this study was to describe the performance of a newly created curricular unit called clinical and imaging anatomy to second year medical students to complement the anatomical teaching of basic anatomy taught during the first year of medical school.
Teaching of anatomy and radiology at NOVA medical School throughout the years
Before the curriculum reform of the medicine course established in 2011/2012 at NOVA medical school, anatomy was taught during the first two years of medical school with two curricular units spanning over the whole year (four semesters) with a total of 336 hours.2 Teaching methodology was based on descriptive and systematized anatomy, with 2 sessions (on in each year) of two weeks dedicated to cadaveric dissection. During each year, anatomy was taught over a period of 28 weeks. In each week, there were two theoretical classes of 50 minutes and two practical classes of 110 minutes. Since the curriculum reform put into place in 2011/2012, anatomy has been taught differently at NOVA medical school:
Descriptive and systematized anatomy of bones and joints, muscles, organs, cardiovascular and nervous system of the whole body: curricular unit of anatomy taught during the first year, first semester, 13 ECTS (European Credit Transfer System), 112 hours - taught by the Anatomy Department.
Anatomy of the central nervous system, curricular unit of fundamentals of neurosciences during the second year, first semester, 8 ECTS, 29 hours - 9 hours dedicated to anatomy taught by the Anatomy department.
Clinical and radiological anatomy, curricular unit of clinical and imaging anatomy (whole human body except central nervous system taught previously), second year, second semester, 8 ECTS, 72 hours - teaching integrated between the anatomy and radiology departments.
Optional curricular units - cadaveric dissection of the trunk during first year, second semester and cadaveric dissection of the head and neck, back and limbs, second year, second semester, each curricular unit with 30 ECTS and 30 hours - taught by the anatomy department.
To face the time constraints for anatomy teaching at NOVA medical school, a new teaching approach and format was adopted, using different modalities of teaching, different teachers with different backgrounds, at different timepoints during the first two years of medical school. Radiology and anatomy teaching were merged in the second year of medical school, to enhance the anatomical concepts introduced during the curricular unit of anatomy during the first semester of the first year. The use of radiology to enhance anatomy teaching has been thoroughly described in medical schools throughout the world.1,4,12-23 The European Society of Radiology has suggested a specific curriculum to optimize teaching of anatomy and radiology during the initial years of medical school.24-26
The curriculum reform of the medicine course established in 2011/2012 at NOVA medical school also led to the extinction of a curricular unit of radiology taught during the fourth year of medical school. Since then, teaching of radiology at NOVA medical school is only mandatory during the curricular unit of clinical and imaging anatomy (second year, second semester), focusing on introducing imaging techniques, image interpretation and radiological anatomy. This could be viewed as insufficient, given the fundamental role of radiology in modern medicine, to diagnose, triage, guide therapeutical decisions and prognostic considerations. At present, the first module of radiology teaching, suggested by the European Society of Radiology,26 is provided at NOVA medical School with the curricular unit of clinical and imaging anatomy. However, the second module of radiology teaching suggested by the European Society of Radiology, focusing on the different pathologies is not structured at NOVA medical school. There is a limited cooperation of radiology teaching with the curricular unit of medicine during the third year of medical school and an optional curricular unit of clinical radiology taught at the fourth year, second semester of medical school.
Organization of the curricular unit clinical and imaging anatomy, second year, second semester, NOVA medical school
The teaching staff comprises three different departments: anatomy, radiology and neuro-radiology. Radiology and neuro-radiology professors are hired specialized consultants and residents. Anatomy professors comprise a variety of different physicians with multiple medical specialities, including specialized consultants and residents. Imaging with radiologists and neuro-radiologists comprises 2/3 of the whole curricular time (48 hours), whereas anatomy comprises the remainder 1/3 (24 hours), totaling to 72 hours for direct contact teaching, with 32 hours of theoretical classes and 40 hours of practical classes spanning over 14 weeks (Table 1).
Table 1: Overall organization of the curricular unit clinical and imaging anatomy along the second semester of the second year of the NOVA medical school.
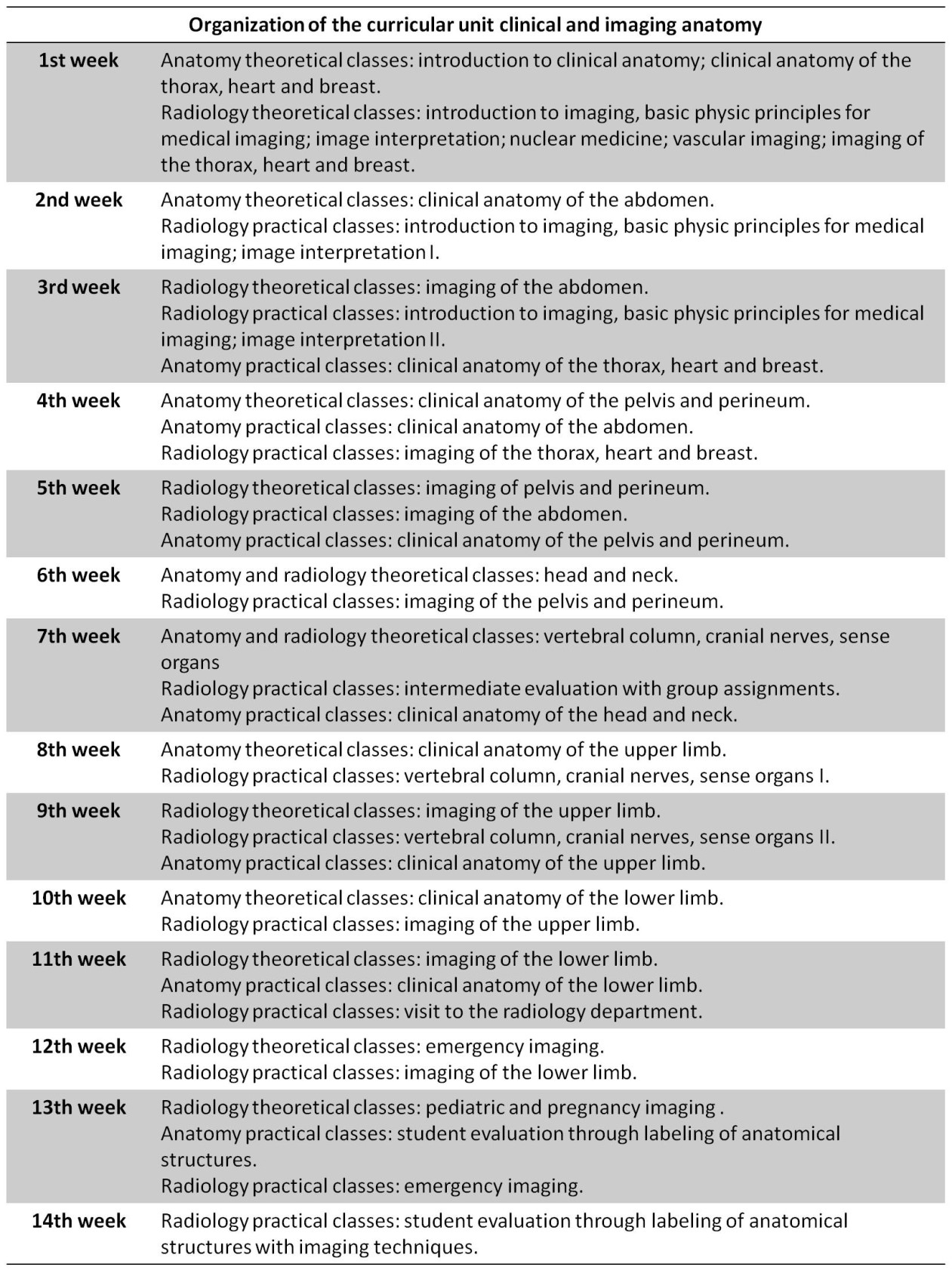
As recommended by the European Society of Radiology (ESR), all theoretical and practical classes were pre-recorded and available before the actual class date,26 allowing students to prepare all class contents beforehand. This allowed time optimization, using the time with the teaching staff for questions and discussion over the study contents, increasing the interaction between teachers and students.26 This approach was very well received among students. All study contents were based on the recommended book references,27-30 digital platforms31-33 and specific contents for more detailed concepts.34-42 Student evaluation was divided into practical evaluation (50%) and final written exam (50%). Practical evaluation was divided into 3 parts: a group assignment (30%); written test of anatomy (35%) and radiology (35%). The group assignment was based on literature research covering specific clinical scenarios where radiological anatomy was relevant. This group assignment was presented during the 7th week of classes. The written tests were performed during the 13th (anatomy) and 14th (radiology) weeks of classes, where students had to label anatomical and radiological images. The final written exam comprised 80 multiple choice questions.
Performance of the curricular unit clinical and imaging anatomy, NOVA medical school between 2012-2020 and improvement strategies.
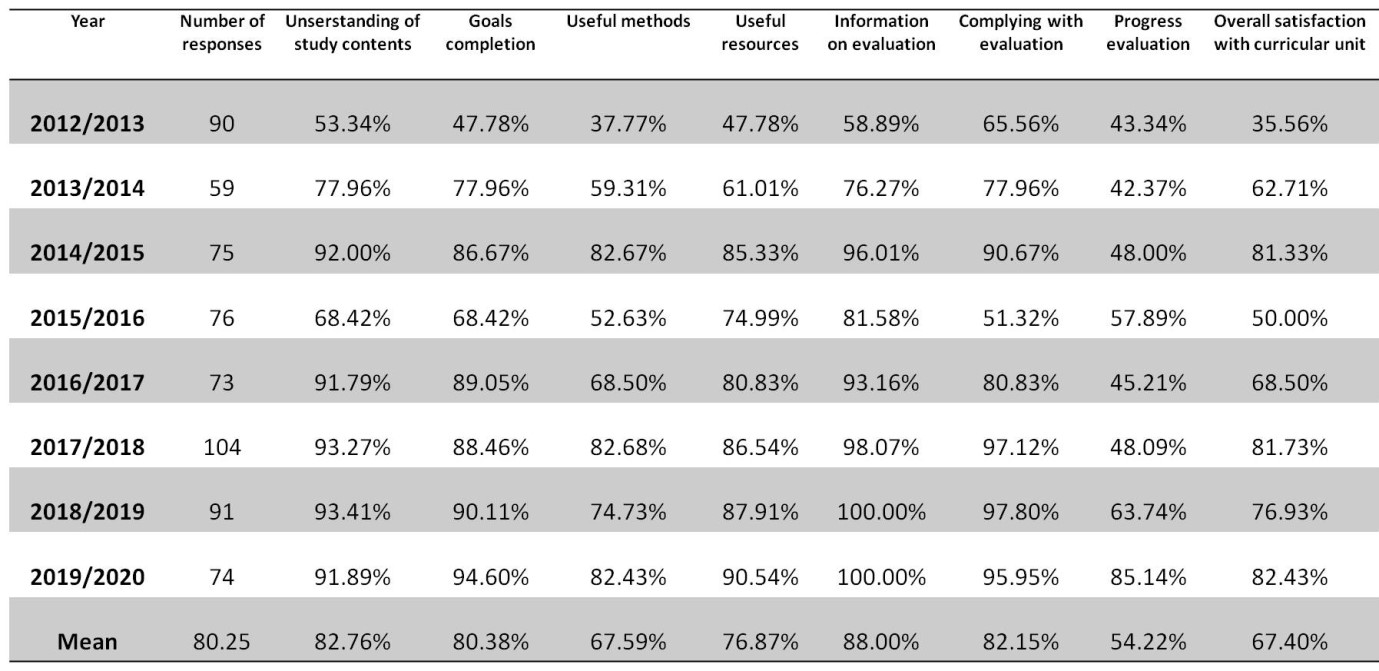
The analysis on the performance of the curricular unit clinical and imaging anatomy was performed since its creation in 2012/2013 until 2019/2020, based on the student´s responses to institutional questionnaires (REIT.DGQ.PR.04) from NOVA University. Institutional review board approval was obtained (115/2021/CEFCM) for the publication of these results. The questionnaires evaluated the student´s perspectives on the organization, structure and performance of the curricular unit (form NMS.CP.FOR.04/NMS.GQ.PR.04). The mean proportion of students responding to the questionnaires was 28% (mean of 80/288 students responded), which is above the designated threshold of 20% to be considered representative (NMS.CP.PR.01.01). The performance of the curricular unit was based on the comprehension of study subjects, goal completion, adequate teaching methodologies and resources, teaching methods, individual progression over the semester, and overall satisfaction (Table 2). Multiple organizational components had to be improved since 2012 to enhance the academic performance of the curricular unit. The greatest challenge was related to the coordination between anatomy and radiology departments. In the initial years, 25% of students responded that the organization of the curricular unit could be improved. This led to a strategic and combined effort of coordination between teaching staff and departments that led to consistently improved outcomes since 2016. The remainder evaluated parameters were well rated, with 5%-15% of students considering that the program, contents, curricular unit duration, articulation with other curricular units, teaching methods and resources, study references, and interest of study contents needed to be improved. The vast majority of students considered the duration of the curricular unit adequate (93.06%) and agreed that the study contents were relevant for future medical practice (95.14%). During the last four years it was possible to consistently achieve study contents comprehension rates above 90% and goal completion rates above 85% (Table 2). During the year 2019/2020, the mean student’s satisfaction rate was 4.4 (scale of 0 worse to 6 best), which was considered adequate by the institutional quality department.
Table 2: Student evaluation on the performance of the curricular unit clinical and imaging anatomy from 2012-2020.
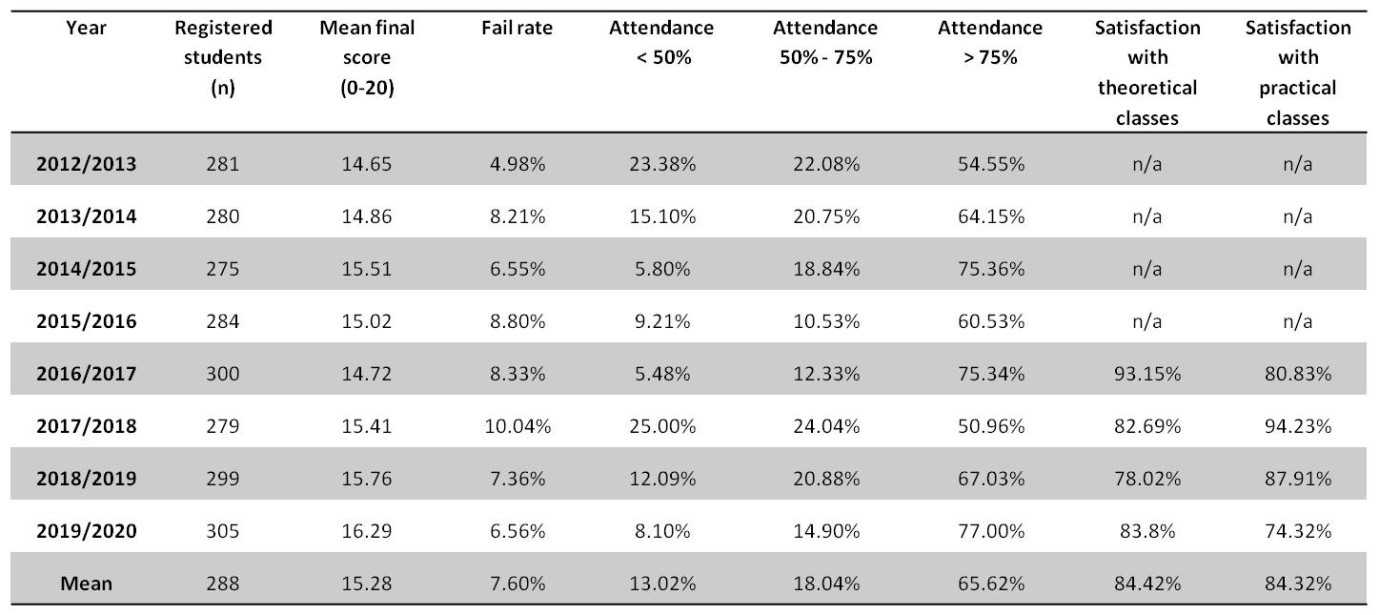
The academic performance of the curricular unit is presented in Table 3. The number of registered students varied between 275 - 305 and the final mean scores between 15 and 16 on a scale from 0-20. The global fail rate was inferior to 10%. These aspects were considered adequate by the institutional quality department. According to regulation NMS.CP.PR.01.01, a curricular unit is considered adequate when the fail rate is < 25%. The class attendance rate improved with the “blended-learning” (combined online and onsite lectures and classes), with an increase in attendance to theoretical classes that were available online. Overall, the mean satisfaction rate with the theoretical and practical courses was 84% (Table 3), also considered adequate by the institutional quality department.
Conclusion
Increasing the efficiency of anatomy and radiology teaching for medical students, considering existing time restraints, might be achievable through different approaches and using a vertical method of teaching throughout the medical school years. Such teaching will potentiate deep acquisition of knowledge, allowing a better understanding and retention of study concepts, minimizing superficial learning based on memorization without comprehension. Methods to teach more and better anatomy and radiology, using less time are reviewed. The specific example of the curricular unit clinical and imaging anatomy from NOVA medical school is reviewed from 2012 - 2020, highlighting the performance of teaching anatomy through imaging. Over 90% of students considered the teaching time adequate (72 hours) and that the study contents were relevant for the future medical role. The global satisfaction rate with the curricular unit and teaching classes was > 75%. Teaching anatomy through imaging was considered well succeeded by > 85% of students. To achieve these performances, a better coordination was required between radiology and anatomy departments. Basic anatomy and radiology concepts were acquired by second year medical students. However, anatomy and radiology teaching need to be further developed during the last clinical years of medical school to enhance learning and understanding of key anatomical and radiological concepts. Also, the importance of imaging within modern medicine, needs to be reflected in the last years of medical school, with dedicated time to teach clinical radiology.