Introduction
A solitary fibrous tumor (SFT) is a rare neoplasm of mesenchymal origin accounting for <2% of all soft tissue tumors, most often found in the pleura, where it was first described by Klemperer and Rabin in 1931.1,2SFT has been reported in extrathoracic locations, including in the retroperitoneum, deep soft tissues of proximal extremities, abdominal cavity, head, and neck.1,3,4,5,6,7However, breast SFT is extremely rare, with just a few cases reported in the literature.1,6
Breast SFT may be found incidentally on screening exams or as the palpable lump of slow-growing and painless.3,6It is usually seen in females between 38 to 88 years (mostly around 50 years old), with variable tumor size (from a few millimeters to several centimeters).3,4Diagnosis depends on imaging features, but confirmatory diagnosis is possible only with histology and immunohistochemical study.5
We present a case of a solitary fibrous tumor of the breast with its radiological and histopathological features.
Case Report
The 49-year-old woman presented with a complaint of a palpable lump in her right breast. She denied any other symptoms, such as pain, nipple discharge, or skin changes. She had no family history of breast cancer and her medical history was unremarkable.
On physical examination, there was a painless soft mass located in the right upper outer quadrant of the breast, measuring approximately 3-4 cm. There were no palpable axillary or supraclavicular lymph nodes.
Mammography revealed an oval circumscribed mass in the right breast, without calcifications, measuring 3.6x2.8x1.5 cm (figure 1).
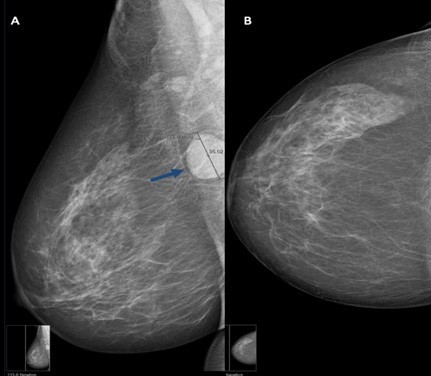
Figure 1: The mediolateral oblique view shows a well-circumscribe, oval mass (arrow) in the upper quadrants of the right breast, deeply located (A). On craniocaudal mammography, the mass is not visualized due to its superior and deep location, close to the axillary region (B).
On ultrasound, this corresponded to a well-defined hypoechoic nodule, with internal and peripheral vascularity on color-Doppler evaluation, and with the longest axis parallel to the skin surface (figure 2). No axillary adenopathies or other breast nodules were observed.
Core-needle biopsy was performed, and the diagnosis of the solitary fibrous tumor was suggested. The patient underwent surgical excision of the breast nodule.
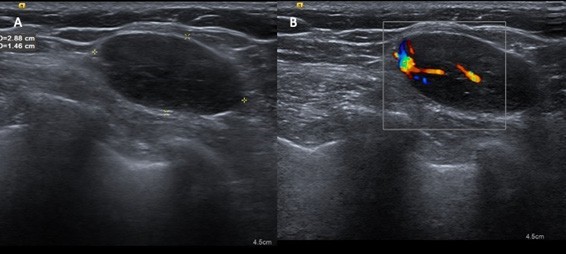
Figure 2: Ultrasound shows an oval hypoechoic mass, with regular margins and the longest axis parallel to the skin surface, in the upper outer quadrant of the right breast (A). The nodule presents central and peripheral vascularity on color-Doppler evaluation (B).
The surgical specimen consisted of a well-defined mass showing a fine fibrous capsule (figure 3A). Histological examination showed a well-defined proliferation of cells with ovoid to spindle-shaped nuclei, haphazardly arranged within a collagenous stroma with alternating hypercellular and hypocellular areas (“patternless” pattern). Cells showed mild to moderate atypia. Blood vessels with branching configuration were also seen (figures 3B and 3C).
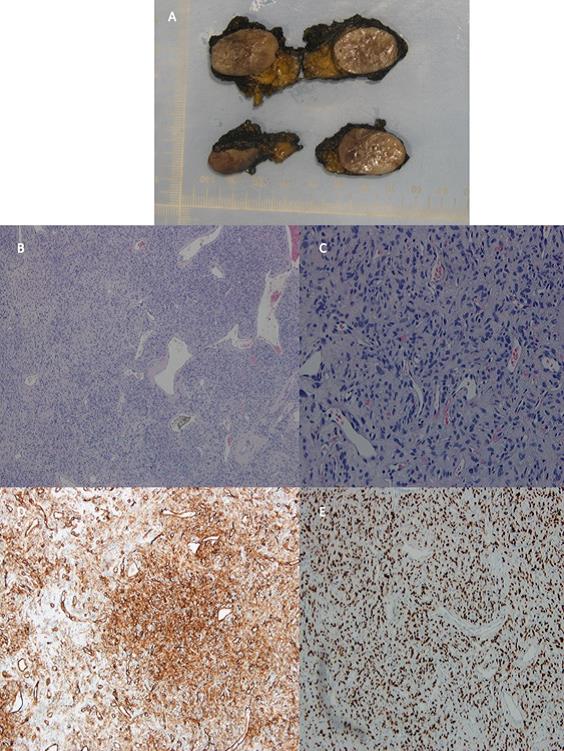
Figure 3: Surgical specimen shows a well-defined mass with a fine fibrous capsule (A). Histological examination shows branching blood vessels and tumoral mesenchymal cells, which are haphazardly arranged with alternating cellularity (hypocellular on left and hypercellular on right) (B) (H&E, x40). Tumor cells have ovoid to spindle-shaped nuclei, without significant atypia, mitotic activity, or necrosis (C) (H&E, x200). Immunohistochemical study reveals a strong positivity for CD34 (D) (CD34, x100) and diffuse nuclear STAT6 expression (E) (STAT6, x100).
In the immunohistochemical study, the neoplastic cells were diffusely positive for CD34 and STAT-6 (figures 3D and 3E), in the absence of expression of cytokeratins (AE1/ AE3) and actin. Mitosis, nuclear pleomorphism, necrosis, and hemorrhages were absent.
Based on the morphological and immunohistochemical features, the final diagnosis is a solitary fibrous tumor of the breast, without features of malignancy.
Discussion
Solitary fibrous tumors of the breast are a rare clinical entity.5 Most of the SFT described in the breast are histologically benign with an indolent clinical course, but cases of malignancy have been reported.1,3It typically presents as a single, painless, and slow-growing nodule.1,2,4Although SFT can occur at any age, it is mainly seen in patients in their 50s (as in this case).5
SFT can incidentally be found on screening tests or manifest as a palpable mass.3 On mammography, the typical finding is a well-circumscribed mass.1 On ultrasound, it appears as a hypoechoic mass with smooth echostructure and vascularization in the color-Doppler evaluation.1 Therefore, radiological assessment usually shows benign features. The most common benign breast tumors are fibroadenoma and fibrocystic disease, but SFT should enter in the differential diagnosis of a single breast tumor with benign imaging characteristics.3 The imaging findings of breast SFT are not pathognomonic, so a definitive diagnosis requires histological examination and immunohistochemical analysis.1,5,7Histologically, STF shows overlapping characteristics with other mesenchymal lesions, and excision of the lesion is often required to reach a final diagnosis.3,5It is characterized by the presence of alternating hypercellular and hypocellular areas, in which neoplastic cells may adopt spindle to ovoid morphology with little cytoplasm.6
The immunohistochemical study is essential for definitive diagnosis. SFT tumor cells are characterized by strong and diffuse positivity for CD34 (90-95%) but are negative for Actin, cytokeratins (AE1/AE3), and hormone receptors.1,3,5,6However, this expression may be seen in a wide variety of mesenchymal tumors.6
Recently, a new highly sensitive and specific marker for SFT has been identified.6 This tumor is associated with a translocation with NAB2-STAT6 gene fusions, which leads to STAT-6 nuclear expression.1,3,5,6,7Thus, the anti-STAT6 antibodies became a specific marker, which makes the final diagnosis of SFT (as in this case).5,6
Tumors with histological features of malignancy and large dimensions have been associated with a high rate of local recurrence and metastasis.3,6
Complete surgical resection is the gold standard of treatment for SFT.1 Chemotherapy and radiotherapy have shown limited efficacy in cases of locally advanced tumors or those with distant metastases.5 Although SFT cases usually follow a benign course, a close follow-up is recommended.2,5
In conclusion, breast TFS is an extremely rare clinical entity, with few cases reported in the literature. Imaging findings on mammography and ultrasound are non-specific, and definitive diagnosis requires histological evaluation and immunohistochemical study. Histology may show overlapping characteristics with other conditions, with STAT-6 being a sensitive and specific marker that makes the definitive diagnosis. Surgical resection is the gold standard treatment. Although most have a benign and indolent clinical course, long-term follow-up is recommended.















