Background
Healthcare workers (HCW) are at high risk of COVID-19 infection due to their professional exposure. Factors susceptible to increase the risk of nosocomial transmission include the lack of knowledge about this emerging novel respiratory virus, especially in the early stages of the pandemic, heavy workload with prolonged and frequent contact with patients, inadequate usage or lack of personal protective equipment, and poor infection prevention and control measures.1
It is estimated that, in Europe and North America, HCW could represent around 14% of reported COVID-19 cases,2 with a higher burden of cases and deaths in the older age groups. Transmission to HCW has been documented in various settings, such as care provision but also staff rooms. Additionally, some evidence suggests differential risk by occupation, with general practitioners and nursing specialty among the most affected.3 However, to date, there are few published data on COVID-19 infections in HCW, as well as limited evidence on the burden, risk, and risk factors. Additional challenges to the understanding of COVID-19 in the health workforce arise from differences in reporting and testing strategies among countries, the lack of standardized definition and classification of HCW, or non-systematic reporting of confounding variables.3
As the pandemic unfolds, healthcare and public health capacities are being stretched to an unprecedented level, highlighting the need for sustainable surge capacities. The impact of COVID-19 on HCW is not limited to morbidity and mortality, but psychosocial consequences are also widely acknowledged.4 At the health facility level, COVID-19 infections in HCW could enhance nosocomial transmission and outbreaks among staff and non-COVID-19 patients. Finally, at the level of the health workforce, COVID-19 infections may lead to depletion of crucial human resources, particularly during surge times.
In this context, protecting HCW is an essential element of a response strategy to COVID-19. The description of epidemiological and clinical characteristics of COVID-19 in HCW is an important step towards a better understanding of the burden and risk faced by the health workforce. Ultimately, such evidence is needed to inform decisions related to surveillance and prevention strategies.
Therefore, we conducted a retrospective observational cohort study to describe the characteristics of HCWs infected by COVID-19 during the first months of national surveillance in Portugal between January and May 2020. Our analysis provides a snapshot of COVID-19 in HCWs in the early stage of the epidemics. We conclude with recommendations to improve the surveillance and knowledge gaps in COVID-19 infections among the health workforce.
Methods
COVID-19 surveillance data
Since January 2020, COVID-19 is a mandatory notifiable disease in Portugal. All suspected cases and laboratory results are reported through the web-based platform of the National Epidemiological Surveillance System (SINAVE). We extracted surveillance data from SINAVE as of May 31st, 2020.
A confirmed case of COVID-19 is defined as any individual with a positive test result (RT-PCR) for SARS-CoV-2, independently of symptoms or signs. Until March 8th, the testing criteria was an epidemiological link with a confirmed case or recent travel history to affected areas, and the presence of fever, cough, and/or shortness of breath. Between March 9th and March 25th, the criteria expanded to hospitalized patients with severe pneumonia and no other apparent causes. From March 26th, it further included all cases of acute respiratory syndrome with cough or fever.5
The HCW status is a binary variable in the notification form of COVID-19 suspected cases. Additional information on the type of occupation is reported optionally in a free text field. We considered variables of interest referring to demographic characteristics of individuals (professional groups, age, sex, and region), clinical presentation (i.e., signs and symptoms) and pre-conditions, hospitalization, and setting of infection.
Study population and period
The study population comprised all individuals with notification of COVID-19 and a laboratory result reported through SINAVE as of May 31st, 2020, that were explicitly identified as HCW, and excluding individuals outside the main working-age groups (i.e., < 18 years old or > 69 years old), and those not professionally active (e.g., medical leave, retirees).
Analysis
We checked data for inconsistencies and missing values. We created age groups from the age in years reported at the time of notification. We codified the occupation of HCW and the potential transmission settings from ‘free text’ fields (i.e., occupation, self-reported epidemiological link). Hospitalization was a binary variable, but admission to the Intensive Care Unit (ICU) was retrieved from a ‘free text’ field referring to the type of service where the patient was admitted.
The denominator used to calculate the proportion of HCW among all the notifications of COVID-19 was the sum of the previous HCW notifications and all the other notifications explicitly identified as not being HCW, reported through SINAVE as of May 31st, 2020, with the same exclusion criteria.
For each variable of interest considered in the descriptive analysis of confirmed cases in HCW, we reported absolute numbers and percentages. Percentages were calculated by omitting missing values, and the proportion of missing values for a given variable was systematically reported.
Data cleaning and analysis were conducted in R software v. 4.0.0.
Results
As of May 31st, there were 24,067 notifications of HCW. Out of these HCW notifications, 3,912 (16.3%) were confirmed cases.
In total, 131,344 notifications of both HCW and non HCW meeting the inclusion criteria were reported during the study period, of which 19,806 confirmed cases and 111,538 non-cases (negative). The proportion of HCW among all these notifications (both confirmed and non-cases) was 18.3% (24,067/131,344). This proportion remained similar when stratifying by case status: HCW represented 18.1% (20,155/111,538) of all non-cases and 19.8% (3,912/19,806) of all confirmed cases.
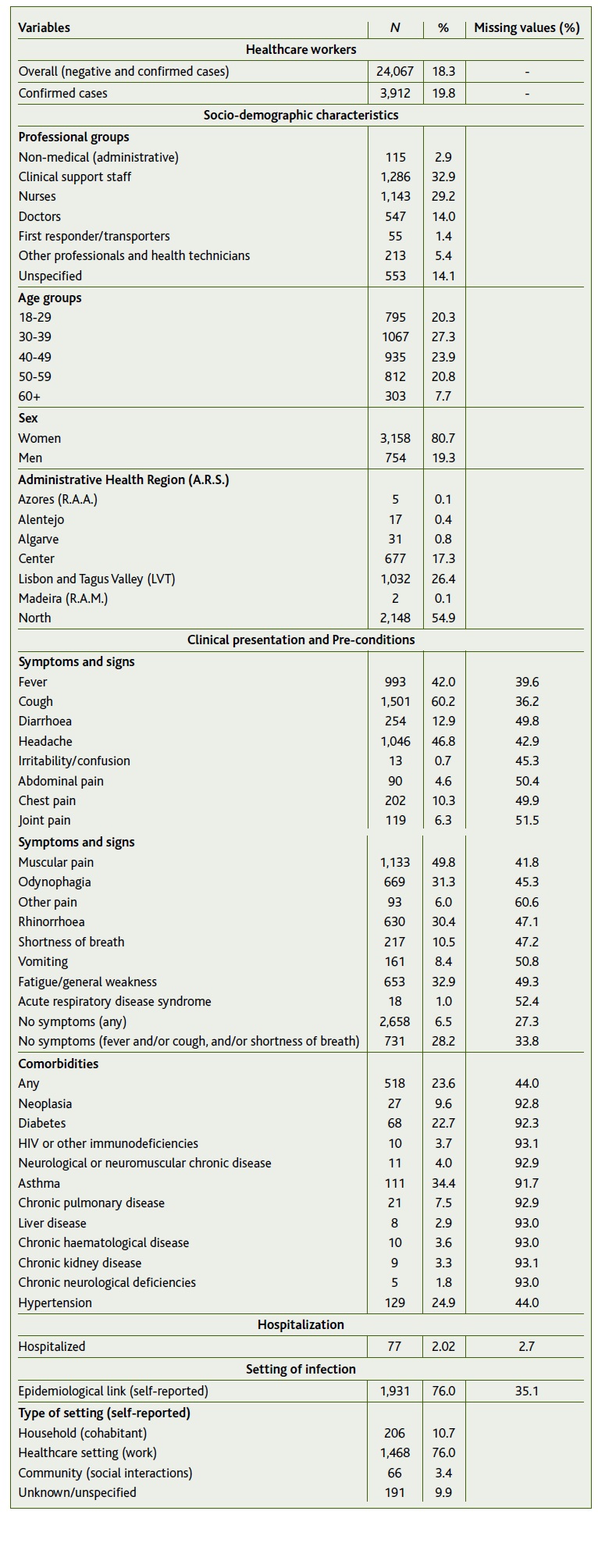
The rest of this analysis focuses on the 3,912 HCW who were confirmed cases (Table 1).
TABLE 1 Characteristics of healthcare workers, confirmed cases of COVID-19, in Portugal, SINAVE (January-May 2020)
Socio-demographic characteristics
The majority of HCW were women (80.7%). The median age was 40.0 years old (interquartile range: 31-51 years). The proportion of each age group was around 20%, except > 60 years old (7.7%)*.
A third (32.9%) of HCW were clinical support staff (e.g., auxiliaries), 29.2% nurses, and 14.0% doctors. Other professionals and health technicians (e.g., physiotherapist, nutritionist, pharmacist, social assistant, etc.), non-medical health professionals (e.g., secretariat, accounting, informatics and communication technologies, etc.), and first responders/transporters were the least represented with 5.4%, 2.9 %, and 1.4%, respectively. It was not possible to identify the occupation of 14.1% HCW.
Place and time
The first confirmed case in Portugal was reported on March 2nd, 2020. From then, the number of cases increased to reach the first peak around the 23rd-26th of March. The temporal distribution of HCW appeared similar to that of the general population (Figure 1).
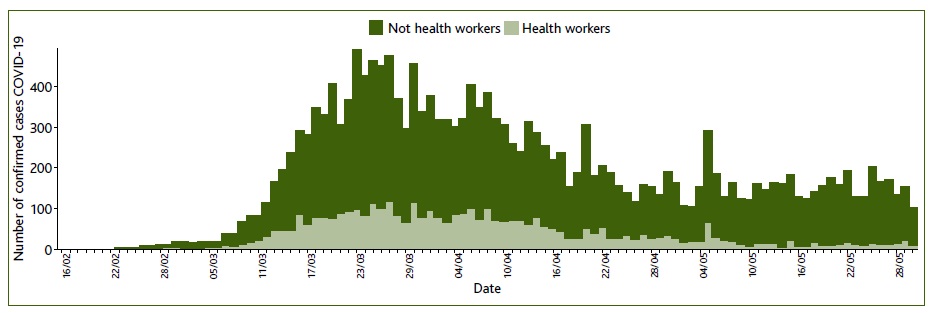
Figura 1 Number of daily confirmed cases by date of symptom onset or date of notification in healthcare workers and non-healthcare workers, Portugal (January-May 2020).
The spatial distribution of cases in HCW also consistently reflected the most affected areas during the study period, with half (54.9%) of them were reported from the North region, a quarter (26.4%) from Lisbon and the Tagus Valley (LVT), and 17.3% from the Center region.
Clinical presentation and pre-conditions
The most frequent symptoms reported at the time of notification were cough (60.2%), muscular pain (49.8%), headache (46.8%), fever (42.0%), fatigue/general weakness (32.9%), odynophagia (31.3%), and rhinorrhoea (30.4%). A total of 731 (28.2%) HCW did not present any symptoms of fever, cough, or shortness of breath, while 186 (6.5%) did not report any symptoms and signs.
A total of 77 (2.02%) were hospitalized, of which at least six (7.8%) were admitted to the Intensive Care Unit. Half (45.5%) of the hospitalized cases were aged 40 years old or more, and at least half presented one or more preconditions.
Overall, close to a quarter (23.6%) of HCW had a precondition. The most frequent were asthma (34.4%), hypertension (24.9%), and diabetes (22.7%).
Settings of infections
The majority of HCW (76.0%) did report an epidemiological link (i.e., contact with a COVID-19 confirmed case or person with COVID-19-like symptoms). The majority referred to the professional healthcare setting (76.0%). Out of those, a third (30.9%) referred to nursing homes or long-term care facilities. Additionally, 206 (10.7%) of HCW reported contact in the household and 66 (3.4%) in the community. The potential setting of infection was not specified for 9.9%.
These settings varied across the different professional groups, such that non-medical health professionals, first responders/transporters, and other professionals and health technicians reported more household contacts, whereas healthcare setting contacts were more frequently reported among medical and clinical support staff (nurses, medical doctors, auxiliaries).
Discussion
During the first months of national surveillance of COVID-19 in Portugal (January-May 2020), 3,912 HCW were notified as COVID-19 confirmed cases. This number could be underestimated as mild and asymptomatic infections are less likely to be tested, and thus reported. Additionally, it is possible that non-medical staff (e.g., secretariat, administration) were not recorded as HCW, and unless the information on the occupation was mentioning a health-care setting, it was not possible to identify them as professionals of the health sector.
Overall, HCW represented 19.8% of all confirmed cases in both HCW and non HCW as of May 31st, 2020. This proportion falls within the range of values observed in other countries (e.g., from 4% in China to 32% in Ireland).3,6-9 Notwithstanding, international figures are not directly comparable, but likely vary with testing rates and strategies or the time period considered. Yet, according to ECDC, as of early May 2020, the overall proportion of HCW among COVID-19 confirmed cases in 15 European countries was 23.2%,7 similar to that observed in Portugal.
An important point to consider is the likelihood of being tested among HCW versus the general population. If HCW are more likely to be tested, then they might be over-represented compared to the general population, particularly for mild and asymptomatic cases or cases that do not fit the testing criteria. We argue that this bias is relatively limited, considering that, in practice, testing widely occurred outside the testing criteria, and Portugal has been known to have a high and sustained testing rate.
Socio-demographic characteristics of HCW positive to SARS-CoV-2 reflect the characteristics of the health workforce in Portugal, specifically the high proportion of women, the lower proportion of older age groups, and the distribution of the different professional groups.11
The presentation of the disease appeared congruous with previous observations in HCW regarding the predominance of mild illness, and the lack of specificity of respiratory symptoms.10,13-15
The spatial and temporal distribution of cases in HCW consistently followed the trends of the epidemic in the general population. Infections in HCW could have increased with the number of infected patients, however, such dynamics might also indicate that HCW were infected in the community. Nonetheless, the majority of HCW reported an epidemiological link, mostly in healthcare settings. This suggests a high awareness of their exposure to COVID-19, even though the epidemiological link is a self-reported variable that could as much reflect the different perception of the risk as to the true exposure. Surveillance data were not precise enough to differentiate between care-provision to COVID-19 patients, opportunistic exposure in the healthcare setting, or contact with infected colleagues. Despite these limitations, the data were consistent with other observations of COVID-19 in the health workforce, suggesting that HCW are highly exposed to nosocomial infections.8,15
Overall, this descriptive analysis is dependent upon the completeness and quality of surveillance data. We cannot exclude minimal misclassifications of the HCW status or other variables. The completeness was relatively low, and optional ‘free text’ fields (e.g., other symptoms, type of epidemiological link, occupation) were not standardized.
Recommendations and conclusion
This descriptive analysis does not pretend to draw any conclusions on the burden, risk, or risk factors of COVID-19 among HCW in Portugal. Rather, it provides a snapshot of infected HCW reported through the national surveillance system. The characteristics of HCW infected by COVID-19 in Portugal were consistent with observations from other countries. Further analyses were limited by the low completeness and lack of detail of surveillance data.
This paper highlights the importance of improving routine surveillance of COVID-19 among HCW. As a starting point, efforts should be made to routinely report the number and proportion of HCWs infected by COVID-19. Moreover, surveillance forms could include variables on the type and place of occupation (e.g., type of health facility, direct contact with the patient, care provision/medical procedures). In addition, incentives should be provided to increase the completeness and quality of the data through the reporting process (e.g., mandatory or zero reporting, validation rules), but also training and feedback to stakeholders, including the health workforce. Additionally, specific surveillance systems among HCW can provide important insights on COVID-19 in the health workforce.
Ultimately, our contribution urges for further data and studies about COVID-19 among HCW. At a time when HCW will be dealing more routinely with COVID-19, such evidence is crucial to protect the health workforce and reduce in-health-facilities transmission by informing strategies of occupational safety and infection and prevention control.
Acknowledgments
We thank Dr Rodrigo Marques for his outstanding contribution to data collection and epidemiological surveillance. We thank all the clinicians, laboratories, and public health workers who participate in the surveillance of COVID-19. We acknowledge all the health workers involved in the response to the pandemic in Portugal and beyond. We thank the Directorate-General of Health COVID-19 Task-Force members.















