INTRODUCTION
Non-melanoma skin cancer (NMSC) represents the most common type of cancer in caucasians, with an incidence that has been steadily increasing worldwide. Basal cell carcinoma and squamous cell carcinoma (SCC) account for the majority of NMSC cases.1,2The most commonly affected anatomic regions are sun-exposed areas like the head and neck, although a large proportion are located on the limbs.3 Extension of the disease will determine the most suitable treatment approach. Multiple treatment strategies are available for localized disease, from wide surgical excision - usually the most common treatment - to Mohs micrographic surgery, cryosurgery or radiotherapy. However, when facing a locally advanced and/ or widespread disease, with clinical and histopathological features associated with bad outcomes, surgical excision with adequate free margins may not be appropriate, leading to serious loss of limb function or even limb amputation.4
Isolated limb perfusion (ILP) is a well-established technique used for the treatment of unresectable tumors of the extremities.2,4It was first introduced in clinical practice by Creech and Krementz, in 1957, in New Orleans, United States of America, in a patient with in-transit metastases of malignant melanoma, who achieved a complete response.5 Nowadays, ILP is mainly used for the treatment of in-transit metastases of malignant melanoma and advanced soft tissue sarcomas of the extremities.4,6However, recent studies have shown ILP’s efficacy in rarer tumours confined to the extremities - locally advanced SCC, cutaneous lymphomas, Merkel cell carcinomas and desmoid tumors.7 ILP has proven to be a safe and effective limb-saving strategy without the systemic toxicity of conventional chemotherapy.4
CASE REPORT
We present the case of a 69-year-old female patient with a history of kidney transplant 10 years before, on immunosuppressive therapy with prednisolone, mycophenolate mofetil and everolimus.
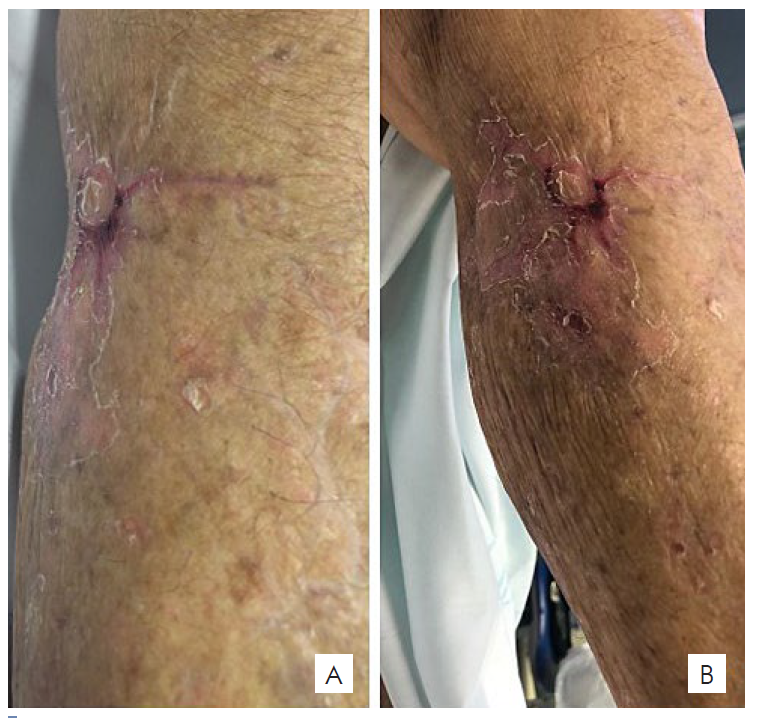
The patient was admitted to the Dermatology Department with a 6-month history of a growing ulcerated nodule on her lower right leg, measuring 5 cm. Wide surgical excision was performed followed by closure with a full-thickness skin graft. Histopathology revealed a completely excised, invasive, moderately differentiated SCC, without perineural or lymphovascular invasion. Four weeks later, multiple erythematous-violaceous papules begin to erupt on the lower right leg in a linear pattern. Enlarged homolateral inguinal lymph nodes were also noticed on clinical examination. Skin and lymph node biopsies were performed and were positive for cutaneous and lymph node metastases of SCC, respectively. Staging PET-CT showed hypermetabolic activity in these locations. On re-evaluation, 4 weeks later, the lesions had evolved to 3-4 cm, exophytic, ulcerated, haemorrhagic nodules, located on the anterior and posterior surface of the lower leg (Fig. 1). Given the regional spread of the disease with locoregional metastases, the patient was treated with ILP, consisting of a combination of melphalan and TNFα. An iliac perfusion was performed with temperatures ranging from 39.5ºC to 40ºC, using 90 mg of melphalan (10 mg/L limb volume) and 1 mg of TNFα. Inguinal and ilio-obturator lymph node dissection was performed at the same time, without immediate intercurrences. A total of 11 lymph nodes were excised, 10 of which had metastases from SCC.
As soon as 1 week after the procedure, partial disease regression was noticed, with a reduction in lesions size and erythema (Fig. 2A) with more significant reduction recorded at week 4 (Fig. 2B). Complete resolution of all in-transit metastases was observed at week 12, leaving only a residual scar on the anterior surface of the leg (Fig. 3). The patient did not experience any local or systemic toxicity. Nevertheless, 4 months later, systemic progression of the disease was reported on the PET-TC, showing hypermetabolic activity at multiple locations. Unfortunately, the patient died 4 months later.
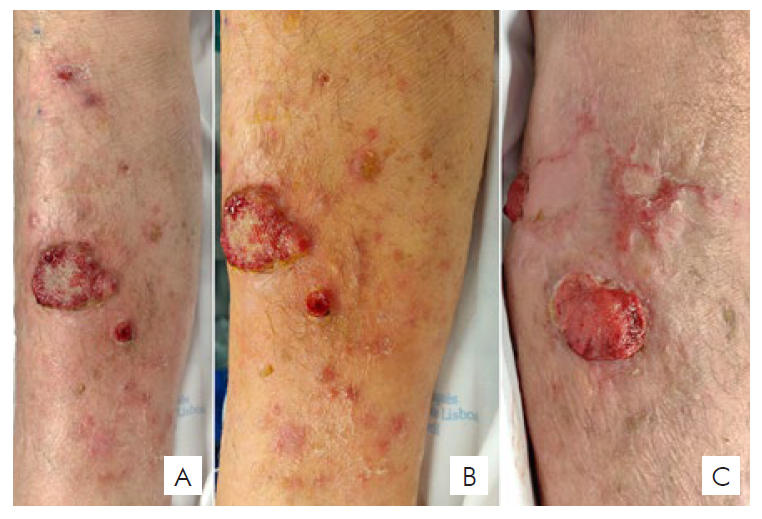
Figura 1 Multiple erythematous and violaceous papulonodules covered with haemorrhagic crusts, located on the anterior (A, B), lateral and posterior (C) aspect of the right lower leg.

Figura 2 One week post-procedure - reduction in size and erythema of the cutaneous lesions (A); Four weeks post-procedure - 1x1 cm erosion on the anterior aspect of the right lower leg with complete resolution of the remaining lesions (B).
DISCUSSION
SCC accounts for most non-melanoma skin cancer-related metastatic disease and deaths.8 Once an invasive/aggressive SCC is diagnosed, it must be staged as the risk for metastases is reported to be approximately 49 and 2 to 3 times higher in immunosuppressed individuals.10 Cutaneous in-transit and regional lymph node metastases are the most common metastatic presentation.8 Treatment modalities described for advanced SCC at any site include conventional cytotoxic chemotherapy, newer systemic therapies, radiotherapy and combinations of these modalities.4 The ILP technique has been extensively described. Its purpose is to allow local administration of high-dose chemotherapy while minimizing serious systemic side effects.3,11
Briefly, after heparinization, the surgeon identifies and cannulates the main vessels of the limb, in this case the right iliac vessels, which were clamped proximally. With the use of an extracorporeal circulation pump, chemotherapy with melphalan and TNFα is infused into the limb. The technique is based on the synergistic antineoplastic effect of chemotherapeutic drugs and high temperature,7 which should be maintained between 38°C and 40°C, measured with two thermometers placed in subcutaneous tissue and muscle. Systemic and regional toxicity should be assessed during perfusion with radiomarked albumin infused on the systemic circulation and a gamma probe.2,7,11,12
Several reports show excellent response rates with TNFα and melphalan- ILP for both malignant melanoma in-transit metastases or locally advanced soft tissue sarcomas.3,6,7However, there is not much evidence on its efficacy when it comes to non-melanoma skin cancer, such as SCC. Veld et al recently reported a case series of 30 patients with locally advanced SSC treated with ILP. The overall response rate was 81%, with 16 patients having a complete response (59%). Limb salvage rate was 80% and the overall 2-year survival was 67%. The authors suggest that ILP should be considered as an option in patients with locally advanced SCC.4 Belgrano et al report two patients with SCC submitted to ILP, with disease stabilization in one patient and a complete response in the other. However, both experienced local progression of the disease within 4-7 months.7
In this case of a SCC with locoregional metastases, the regression of all in-transit metastases was considered an indicator of a successful outcome, mitigating the need for limb amputation. However, despite its regional efficacy, ILP is unlikely to have a great impact on survival, as shown in several large prospective studies on melanoma and locally advanced soft tissue tumors.6,13,14The widespread disease observed later in this patient might have been a result of systemic metastases that were undetected by imaging and clinical evaluation.
In conclusion, in this patient, ILP was an effective and well tolerated limb-saving palliative treatment. However, it did not have any impact on the overall prognosis. This technique can be regarded as a therapeutic option in the management of multiple, locally advanced, drug-resistant tumors of the limbs, when surgical therapy is not feasible.