INTRODUCTION
Psoriasis is a chronic, immunoinflammatory, cutaneous disease characterized by epidermal hyperplasia, accelerated keratinocyte evolutionary cycle, and inappropriate immune activation. Its distribution is universal with similar involvement between the sexes. It has two incidence peaks: between 20 and 30 years of age and after 50 years.1
This condition affects approximately 2% of the population. Its clinical presentation is varied, but psoriasis vulgaris occurs in 85% to 90% of patients with the disease. These have a high frequency of comorbidities, as well as a significant impact on health-related quality of life due to skin appearance and adverse effects of medications.2
Although psoriasis is classically linked to the development of cutaneous erythematous desquamative plaques, increasing evidence supports its recognition as a multisystem chronic inflammatory disease with multiple associated comorbidities, such as metabolic syndrome, cardiovascular and cerebral disease, psychosocial effects, alcohol abuse, psychiatric disorders.3-5
The great impact of psoriasis on the patient's quality of life is evident in the aspects of physical and mental health similar to other diseases such as cancer, arthritis, coronary artery disease, and diabetes.6,7These patients show higher rates of depression, anxiety and suicidal ideations as well as alcohol abuse, smoking and sexual dysfunction, which are often unrecognized or ignored. These comorbidities are more prevalent in female patients with severe disease, associated psoriatic arthritis, and previous psychiatric illness.8-10
A significant association was found specifically between major depressive disorders and psoriasis, primarily related to immune mechanisms and the action of inflammatory cytokines such as tumor necrosis factor (TNF)-alfa, interleukin-1 (IL-1), IL-2, IL- 10, IL-6, IL-8, prostaglandin E2 and C-reactive protein.11 In particular, TNF-alfa has been identified as a proinflammatory cytokine that induces depression even in patients with no history of mental illness. In addition, its highest blood levels were found in patients with suicidal ideations.12
Anti-TNF drugs, such as adalimumab, etanercept and infliximab, used for the treatment of psoriasis have been associated also with the improvement of psychiatric comorbidities.12 It is difficult, however, to ascertain whether the beneficial effect observed from the use of anti-TNF drugs is due to a direct effect into the pathophysiology of depression or secondary to improvement of the cutaneous and joint lesions and consequent improvement of the quality of life.
The dermatologist should always evaluate the social, emotional and psychological aspects when managing patients with psoriasis. If these items are addressed in patient care, quality of life, prognosis and therapeutic response may be
improved.13 Therefore, this study aims to determine the prevalence of anxiety and depression disorders in patients with psoriasis vulgaris diagnosed in the Dermatology outpatient clinic of State University of Pará, Brazil, as well as to explore their relationship with disease severity, treatment options and clinical response to treatment.
MATERIAL AND METHODS
Observational and cross-sectional study with a quantitative approach, performed in a dermatology outpatient clinic. The occurrence of depression and anxiety disorders in patients diagnosed with psoriasis vulgaris was analyzed.
Data collection took place after approval of the project by the Marco Health Center School from the State University of Para, Brazil Ethics and Research Committee (opinion number: 2 451 002, approved on December, 2017) in compliance with the guidelines on human research of the Helsinki Declaration and the National Health Council Resolution 466/2012.
The aim was to apply internationally validated scores to patients diagnosed with psoriasis vulgaris, namely questionnaires such as GAD-7 and PHQ-9 for screening of anxiety and depression disorders that were administered in a single moment.
The PHQ-9 score is an internationally validated instrument containing nine questions that allows screening, measuring the severity and monitoring depressive disorders.
Scores greater than 10 have a sensitivity and specificity of 88% for major depression. Scores above 5, 10 and 15 represent mild, moderate and severe conditions, respectively.14,15
The GAD-7 score consists of seven questions. It is validated and has proven efficiency for screening and monitoring the severity of signs and symptoms of generalized anxiety disorder. It has a sensitivity of 89% and a specificity of 82%. As in PHQ-9, scores above 5, 10 and 15 also represent mild, moderate and severe conditions, respectively.16
PASI was calculated and patients were evaluated according to disease duration and the therapy: topical, methotrexate or immunobiological treatment.
This is a convenience-sampled study, which included all consecutive patients who attended to the dermatology outpatient clinic after the beginning of the research, of both sexes, over 18 years, with confirmed clinical diagnosis of psoriasis vulgaris and who agreed to participate in the research by signing the informed consent form.
The sample characterization information was obtained from a database prepared using Microsoft® Office Excel® 2013 software. The sample was evaluated by descriptive statistics, through frequency distributions (absolute and relative), measures of central tendency (arithmetic mean) and variance (standard deviation).
To assess the overall distribution of the sample, the chi-square test of adherence was used. For the evaluation of distribution between groups (gender, employment status and education), the chi-square independence test or the G test were used. To evaluate quantitative variables between groups, Student's t-test or Mann-Whitney test (for two groups) and one-way ANOVA or Kruskall-Wallis (for more than two groups) were used.
All statistical inference was performed using the software BioEstat and Graphpad Prism 6, considering significant a p-value ≤ 0.05.
RESULTS
Ninety patients with the diagnosis of psoriasis vulgaris were included. There was a predominance of female patients with 56 women (62.2%) and the predominance of the age group of 51 to 60 years in 52.2% of participants. Most patients had a high education level (mostly high school), were employed and non-users of alcohol or tobacco (Table 1).
Table 1 Demographics of the group of patients with psoriasis vulgaris.
| Demographics | n | % | p-value |
|---|---|---|---|
| Sex | |||
| Male | 34 | 37.78 | Chi-square |
| Female | 56 | 62.22 | 0.0269 |
| Total | 90 | 100.00 | |
| Age | |||
| 18 to 30 years | 7 | 7.78 | Chi-square |
| 31 to 40 years | 14 | 15.56 | <0.0001 |
| 51 to 60 years | 47 | 52.22 | |
| >60 years | 22 | 24.44 | |
| Total | 90 | 100.00 | |
| Schooling | |||
| Elementary school | 28 | 31.11 | Chi-square |
| High school | 42 | 46.67 | 0.0160 |
| University education | 20 | 22.22 | |
| Total | 90 | 100.00 | |
| Employed | |||
| Yes | 60 | 66.67 | Chi-square |
| No | 30 | 33.33 | 0.0022 |
| Total | 90 | 100.00 | |
| Smoking | |||
| Yes | 4 | 4.44 | Chi-square |
| No | 86 | 95.56 | <0.0001 |
| Total | 90 | 100.00 | |
| Alcohol | |||
| Yes | 10 | 11.11 | Chi-square |
| No | 80 | 88.89 | <0.0001 |
| Total | 90 | 100.00 |
Disease duration varied between 2 months and 67 years (mean: 11.59 +/- 8,11). PASI score was below 10 in 68 patients (75%) at the time of the survey and 22 patients (24.44%) had a PASI above 10. Out of the 90 patients enrolled, 41 (45.56%) used only topical treatment,28 (31.11%) used oral methotrexate and 21 (23.33%) used immunobiological agents (Table 2). Among those who used immunobiological agents, 100% used an anti-TNF drug, either adalimumab or etanercept.
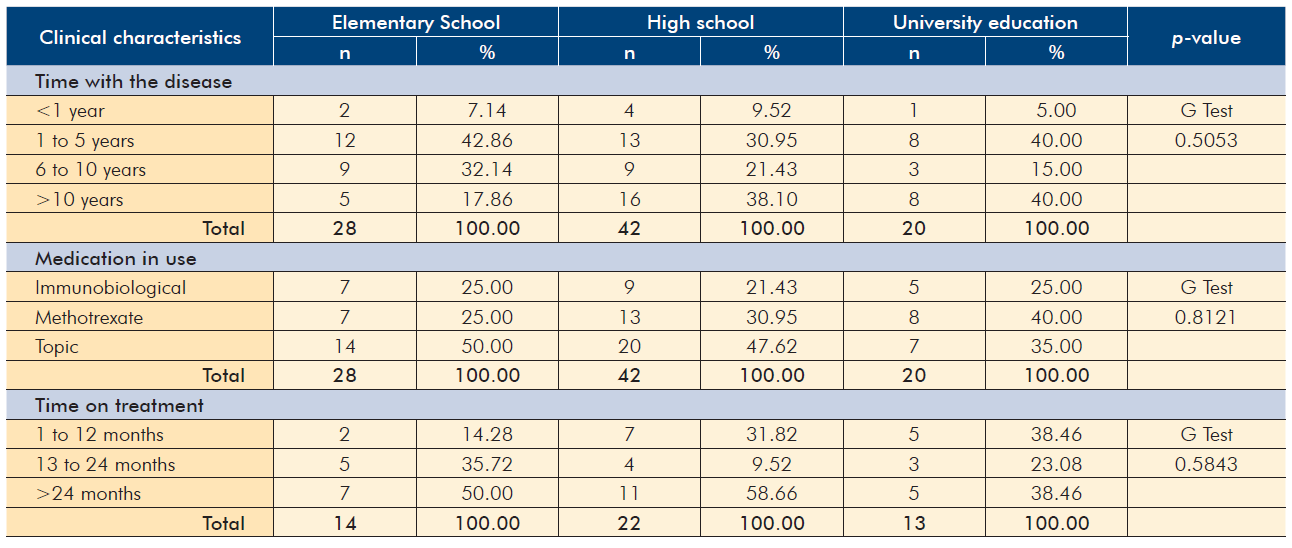
Tables 2 and 3 demonstrate that there was no statistically significant association between the clinical characteristics (disease duration, medication in use and time on treatment) and, respectively, gender and schooling of the patients.
Table 2 Clinical characteristics of the whole group of patients with psoriasis vulgaris in a Dermatology Clinic and by gender.
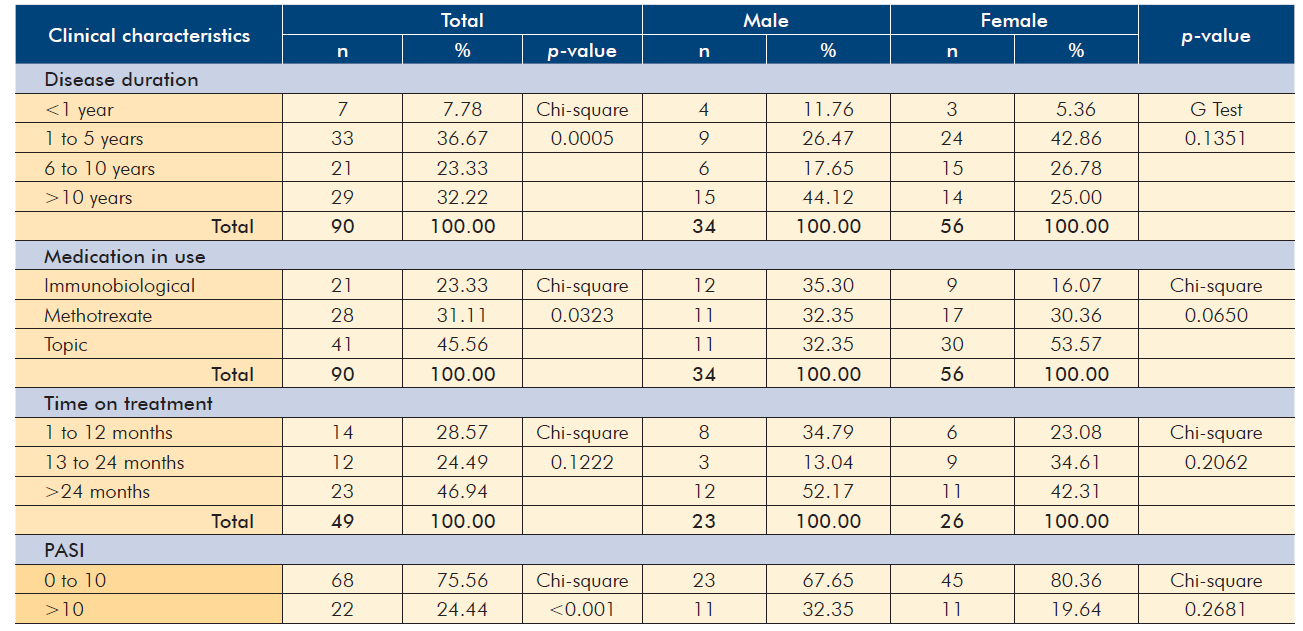
Table 3 Clinical characteristics according to the schooling of patients with psoriasis vulgaris in a Dermatology Clinic.
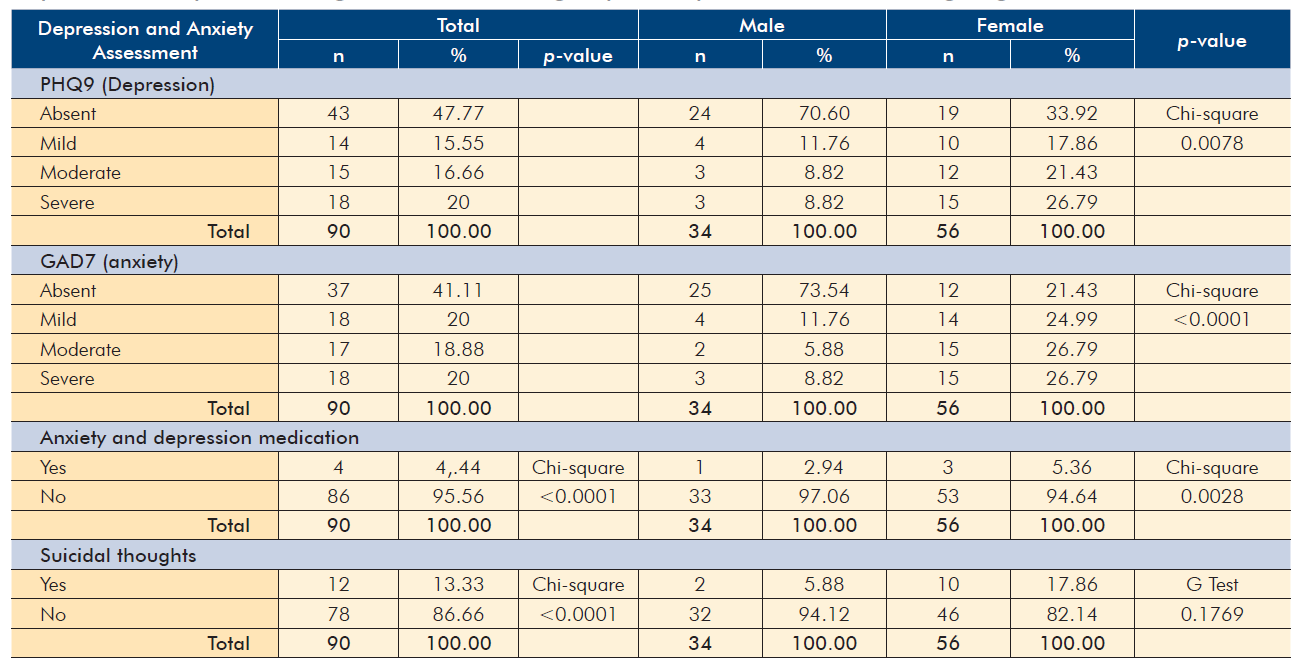
Furthermore, the prevalence of depression and anxiety was verified according to the PHQ9 and GAD7 questionnaires.
Regarding the PHQ9 score, 47 patients (52.23%) had some degree of depression, 14 (15.55%) of them had mild depression, 15 (16.66%) moderate and 18 (20%) severe.
Regarding the GAD7 score, 53 patients (58.89%) had some degree of anxiety disorder, 18 (20%) of them had mild symptoms, 17 (18.88%) moderate and 18 (20%) severe.
Eighty six patients (95.56%) out of the 90 studied were not treated with any drugs intended for depressive or anxiolytic disorders. The prevalence of suicidal thoughts in patients with Psoriasis in this clinic was 13.33 % among the 90 patients studied. Statistically significant association was found between the prevalence of depression and anxiety and the female gender, a fact that is not correlated with the PASI score.
The tests for association between qualitative variables - Chi-square and G Test - demonstrated that there was no statistically significant association (p > 0.05 in all situations) between the prevalence of anxiety and depression and employability or the academic education of patients. In addition, the categorization of the age group in relation to the presence or absence of depression and anxiety demonstrated that no group had statistical strength either. There was no statistically significant correlation between the PASI score and the presence of depression (p = 0.4868) or anxiety (p = 0.2122) (Fig. 1).
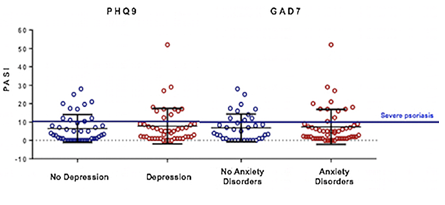
Figure 1 PASI score did not correlated with the presence of depression (p = 0.4868, T Test) or anxiety disorders (p = 0.7544, T Test) according to PHQ9 and GAD7 scores, respectively.
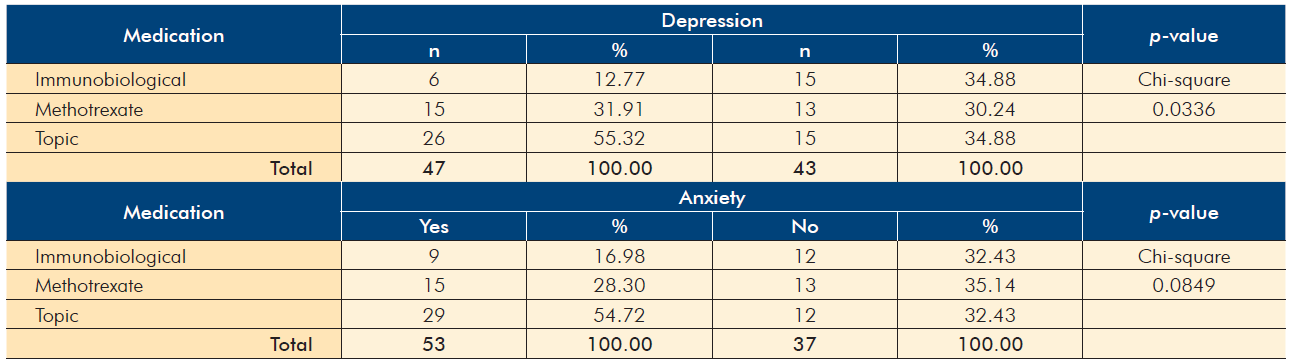
We found a significantly lower prevalence of depression in patients using immunobiological agents (p=0.0336). Depression was observed in 6 out of 21 patients treated with immunobiological agents (28.6%) whereas it occurred in 15 out of 28 (63.6%) and 26 out of 41 (63.4%) under methotrexate or topical drugs, respectively (Table 4).
DISCUSSION
The association between psoriasis and mental health aspects is already well established due to social stigmas and chronicity of the disease.17 Feelings of rejection, guilt and shame are the main aspects of stigmatization, correlated with the intensity of pruritus, stress, depressive symptoms and quality of life.18 Although psoriasis is associated with alcohol drinking and smoking habits, in this study no association was found.19
A recent systematic review has shown that psoriasis patients have a higher risk of anxiety symptoms (approximately 82.8%), generalized anxiety disorder (33%) and depressive symptoms (68%). Other psychiatric symptoms such as sleep disorders, sexual dysfunction, and personality disorders are also frequently reported. The prevalence of suicidal ideation in psoriasis is between 2.4% - 9.7% and commonly occurs in the context of depression.20 These data are in agreement with the results found in this study, with the prevalence of anxiety and depression of 58.89% and 52.23%, respectively, and with the percent of the patients with suicidal ideations (13%).
Although anxiety and depression disorders are classically related to the severity of psoriasis, both ours and other studies showed that there is no relationship between the severity of the clinical picture evaluated by the PASI and the occurrence of these psychiatric comorbidities.12 In agreement with the findings of this research, in which there was no statistically significant relationship between the presence of anxiety and depression and the variables such as age, unemployment, education and even with PASI values above 10, all patients may have a similar risk and should be screened for signs and symptoms of depression and anxious mood.12 Strober et al in 201821 reported the association of depressive symptoms with a low educational level, which was not observed in this study.
In addition, the author describes no gender difference, which is contrary to the results of this study, in which females showed a higher association with depression and anxiety (Table 5).
Table 5 General assessment of levels of depression and anxiety, use of medication for depression and anxiety in patients with psoriasis vulgaris, in the whole group of 90 patients and according to gender.
Within this investigative scenario, new hypotheses for the risk of depression and anxiety were raised. Psoriasis, as a chronic and inflammatory disease, has long been interpreted as a multisystemic morbidity, not just limited to the skin. It was hypothesized that a pathophysiologic mechanism mediated by inflammatory cytokines, with special attention to TNF-alpha, acts directly in the central nervous system,22 and that targeting these cytokines with specific treatment also improves these comorbidities.
The PSOLAR Cohort Study, which involved approximately 12 000 psoriasis patients in 16 different countries receiving immunobiological, phototherapy and conventional systemic therapies such as methotrexate, acitretin, cyclosporine. And corticosteroids,21 demonstrated that treatment with immunobiologicals reduced the risk of depressive symptoms (RR 0.76; 95% CI 0.59-9.98) compared with conventional systemic therapy (RR 1.05; 95% CI 0.71-1.54). These results are in agreement with the data of the present research. In addition, the incidence rates of depressive symptoms were significantly lower than those in other groups, demonstrating an incidence of 3.01 per 100 patient/year (95% CI, 2.73-3.32), 5.85 per 100 patient/year (95% CI, 4.29-7.97) and 5.70 per 100 patient/ year (95% CI, 4.58-7.10) for biological, phototherapy, and conventional therapy, respectively.
Emerging research suggests that there is a link between the pathophysiology of psoriasis and depression. Proinflammatory cytokines such as TNF-α and IL-17 are present in both psoriasis and depression. Other chronic inflammatory diseases such as systemic lupus erythematosus and Crohn's disease are also associated with psychiatric comorbidities, reinforcing this link between pathophysiology and opening new horizons to the potential of targeted therapies for psoriasis.23,24
Genetic studies provide additional information, as genetic polymorphism of TNF-α (rs1799724, a single nucleotide polymorphic variation), which would selectively increase TNF-α expression in certain anatomical areas of the cortex, occur in depressed patients.25 This highlights that TNF-α may have a significant role in the pathogenesis both of psoriasis and of depression and as a possible target in the treatment of a certain group of patients, particularly those who carry this genetic polymorphism.
Given the relation between psoriasis and depression, the dermatologist will have to be prepared to recognize the patient's mental and emotional states and provide a type of psychological support to his patient, starting with a highly effective doctor-patient relationship, stress management resources and even psychopharmacological and psychological therapies. In many cases there will be a need to integrate with professionals in Psychology and Psychiatry to address specific
cases of these specialties.26
CONCLUSION
Psoriasis is a multisystemic chronic disease associated with several comorbidities, such as depression and anxiety. Out of the 90 psoriasis patients of this study, 52.23% have some degree of depression and 58.89% some degree of anxiety with no statistical significance related to education, employability, age or PASI score above 10 and only a greater correlation with the female gender and a lower prevalence among patients who are under anti-TNF-alfa treatment.
TNF-α, is pointed as one of the main causes of the inflammatory response in the CNS, triggering the neuropsychiatric comorbidities, therefore opening doors for using this type of immunobiologics in the treatment of psoriasis and these comorbidities as a better choice for such patients.