INTRODUCTION
The COVID-19 pandemic has had a major worldwide impact, even though we still know little about this disease.
Along with the typical respiratory symptoms of viral infections, various cutaneous manifestations have also been associated with SARS-CoV-2, so Dermatology has made na enormous contribution to this pandemic.1
Two main studies described more than 50% of cutaneous manifestations appearing after hospitalization,2,3
Lesions were mostly a skin rash (>70%) affecting mainly the trunk and upper limbs, which was only mildly pruritic and self-limited (2-5 days duration). But a wide range of skin manifestations has been associated with COVID-19: petechial, erythematous, urticarial, vesicular eruptions, transient livedo reticularis, Raynaud phenomena, annular, erythema-multiforme and chilblain-like lesions.4-9
Getting to know SARS-CoV-2 manifestations and its pathogenesis is one of the cornerstones of investigation since it directs the study of possible treatments. Furthermore, it is of utmost importance to raise awareness of COVID-19 skin manifestations as primary manifestations.
CASE REPORT
A 84-year-old male was taken to the emergency department (ED) as he was found lying on the floor of his home with associated sphincter incontinence. His clinical history was notable for dyslipidemia, hypertension and an ischemic stroke. Since 2016, he had thrombocytopenia of unknown cause. He was under daily treatment with amlodipine 5 mg, furosemide 80 mg, and simvastatin 20 mg. No drug allergies were reported.
At the ED, he had a 7-point Glasgow Coma Scale, was hypothermic (tympanic temperature 29.9ºC) and had purulent respiratory secretions which needed to be aspirated.
There were no acute findings on brain computed tomography (CT) scan or electroencephalogram. He had leucocytosis (14.2 x 109/L) with neutrophilia (12.72 x 109/L), lymphocytopenia (0.47 x 109/L), thrombocytopenia (104 x 109/L), high C-reactive protein (4.43 mg/dL) and D-dimers (671 ng/dL). A chest radiography showed bilateral hilar reinforcement and areas of hypotransparency already present in previous exams. Chest CT showed bilateral thickening of the bronchial walls, an area of parenchymal densification in the apical segment of the right upper lobe, and fibro-atelectatic areas in the lower lobes. A nasopharyngeal swab for SARS-CoV-2 was negative. He was then admitted to a medical ward with the diagnosis of community-acquired pneumonia and hypoxemic respiratory insufficiency.
The patient completed 5 days of azithromycin 500 mg IV and 8 days of ceftriaxone 1000 mg IV with recovery of consciousness, resolution of respiratory failure and normalization of imaging and analytical parameters, except for thrombocytopenia.
Nevertheless, on day 7 of hospitalization, with no associated respiratory distress or other relevant systemic symptoms, he developed a non-pruritic symmetric maculopapular rash on the trunk and arms, next to axillary folds, with red confluent erythematous lesions that extended to the shoulder and flexures. On the following day, cutaneous lesions progressed to the cervical region and upper trunk (Fig. 1), subsequently stabilizing until resolution within 7 days of onset. Lower limbs, face, palmoplantar regions and mucous membranes were spared. Concomitantly, a second SARS-CoV-2 nasopharyngeal swab was positive and there was a slight increase of inflammatory serum parameters, namely leukocytes (10.4 x 109/L), neutrophils (7.95 x 109/L) and C-reactive protein (7.47 mg/dL), but prothrombin time, activated partial thromboplastin, renal, hepatic and thyroid function tests, antinuclear (ANA) and anti-neutrophil cytoplasmic antibodies (ANCA) were normal or negative. Two other patients in the same ward, with no exposure to antibiotics, had a similar rash and has a positive nasopharyngeal swab for SARS-CoV-2.
For the differential diagnosis of this patient a non-immediate drug eruption related to the antibiotics and a viral exanthema related with SARS-CoV-2 infection were considered.
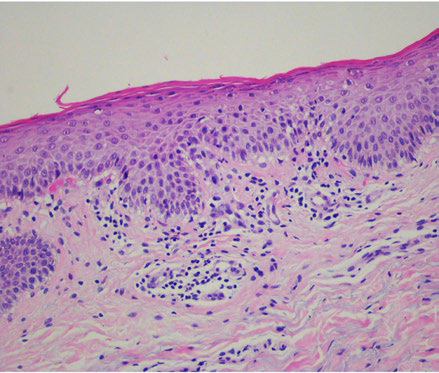
A punch biopsy performed on the patient’s right arm showed mild parakeratosis, focal spongiosis and lymphocyte exocytosis. Vasodilation was seen in the upper dermis with a predominantly perivascular lymphocytic infiltrate, no eosinophils and very rare extravasated red blood cells.
There were no signs of vasculitis (Fig. 2). Immunohistochemistry revealed almost exclusively T cells, predominantly CD4+, with only mild expression of CD8+.
The rash resolved in a week with no specific treatment and the patient recovered fully from COVID-19 only with supportive therapy. Six weeks after recovery, a patch test with several systemic antibiotics, including azithromycin and ceftriaxone at 10% pet (Chemotechnique Diagnostics, Vellinge Sweden), performed according to the ESCD recommendations, 10 was negative on day 2 and day 4.
DISCUSSION
A symmetric maculopapular rash of the neck, trunk and upper limbs, occasionally also with a flexural distribution, that appears concomitantly with the identification of SARS-CoV-2 in the nasopharyngeal mucosae has been described by other authors11 and may be the initial manifestation of the viral infection. However, in this case, we cannot absolutely exclude the pathogenic role of the antibiotics taken for bacterial pneumonia, even though negative patch tests and the scarcity of eosinophils in the skin biopsy make it unlikely. Otherwise, as reported for Epstein-Barr virus and cytomegalovirus, the simultaneous viral infection and antibiotic intake may have enhanced the cutaneous rash.
Pathophysiology of these cutaneous lesions in COVID-19 is still unknown. A skin biopsy showing vasodilation and a perivascular infiltrate of CD4+ T cells in the upper dermis with a slight epidermotropism has been shown in other viral exanthema and is similar to the ones found in other skin biopsies from COVID-19 patients.6,12
SARS-CoV-2 has been widely suspected as the aetiology of different cutaneous manifestations in infected patients, with maculopapular and urticarial exanthema mostly associated with an indolent course with minimal or even absent fever or respiratory symptoms. However, patients and health professionals are not fully aware that exanthema may be an initial manifestation of the infection, and that these patients are likely contagious.
In summary, maculopapular exanthema has been described in patients who tested positive for SARS-CoV-2, but more studies are needed to clear the pathomechanisms involved in exanthema from this virus. Exanthema should raise an early suspicion for this infection and the awareness of the medical staff may contribute for an early diagnosis and prevention of transmission.