Introduction
Endovascular mechanical thrombectomy (MT) changed acute ischaemic stroke (AIS) management and has been considered the standard of care for patients with proximal anterior circulation occlusion.1,2 When timely used, MT reduces the percentage of ischaemic territory,9 reduces the severity of disability over the range of the modified Rankin scale, and leads to higher rates of functional independence.10 MT improves outcome across a range of subgroups including the elderly, patients not receiving alteplase, and patients who present later than 300 minutes from symptom onset.1 The rates of intracranial haemorrhage and intracerebral haematoma are no higher with endovascular thrombectomy than with best medical therapy alone, and mortality risk did not significantly differ between groups.1,9-11 Therefore, MT improves functional independence, without increase in mortality.3,4
Despite its advantages, about 20% of patients treated with MT do not have a successful recanalization (Thrombolysis in cerebral infarction (TICI) 0 or 1), leading to poor clinical outcome.2,5,6 Little is known about the reasons for failed recanalization attempts6 and there are no guidelines on how to treat these patients when such failures occur.2
We present a case of acute ischaemic stroke of the anterior circulation due to occlusion of the common carotid artery successfully submitted to surgical thrombectomy after failed MT.
Case report
A 43-year-old autonomous male patient presented to the emergency room with sudden onset pain on both lower limbs. He had previous history of diabetes mellitus, hypertension, dyslipidaemia, and heart failure with a prior echocardiogram showing intraventricular thrombi (due to poor therapeutic compliance). Physical examination showed skin pallor on both lower limbs and a prolonged capillary refill time; he had diminished femoral pulses and absent popliteal and distal pulses on both limbs. Lower limb doppler ultrasound (DUS) revealed the presence of thrombus on both superficial femoral arteries. Computed tomography angiography (CTA) of the abdomen, pelvis and lower limbs corroborated with previous findings on DUS and revealed also hypodense areas of the spleen and superior pole of right kidney, consistent with ischemic infarcts.
Patient was submitted to a successful bilateral femoral thromboembolectomy and started non-fractioned heparin drip. On the second day post-op non-fractioned heparin was switched to low molecular weight heparin (adjusted to weight and renal function) as the patient remained stable and lower limb perfusion was not threatened.
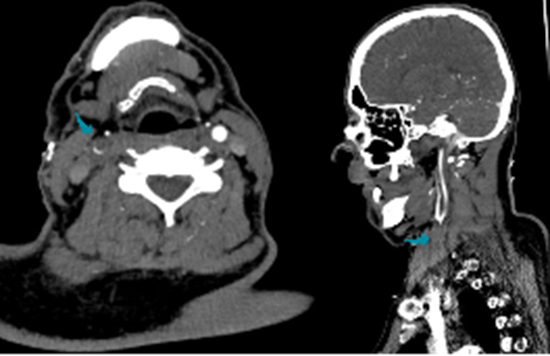
n the fifth postoperative day he developed sudden depression of cognitive status with Glasgow coma scale of 7 and left side hemiplegia, of brachial predominance. CTA revealed an occlusion of brachiocephalic trunk (BCT), right subclavian artery (SA) and common carotid artery (CCA), preserving its branches (Figure 1). Head CT showed no early signs of cerebral infarction.
Axial (left) and sagittal (right) view showing brachiocephalic trunk occlusion (blue arrows)
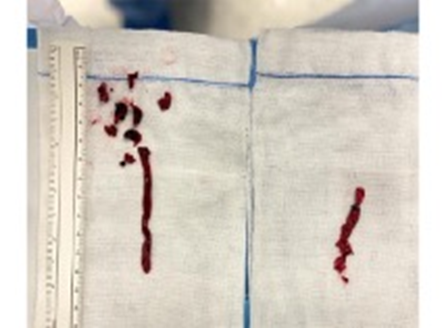
MT, performed by interventional neuroradiology, was unsuccessful (occlusion reached and passed with microwire however stent retriever failed): TICI 0. After multidisciplinary discussion, and about 6 hours after MT attempt, the patient was admitted to the vascular surgery operating room and underwent urgent surgical thrombectomy via right CCA and axillary artery: after right ICA control, and heparinization with a bolus of 5000 IU of unfractioned heparin (UFH), a clamp was placed at its origin to prevent cerebral embolization. Additional UFH administration was performed according to intraoperative anti-clotting time (ACT) monitorization (ACT target of 250 seconds). Cerebral perfusion was monitored intraoperatively using the INVUS® system. Thrombectomy of the right SA, BC trunk and right CCA was successfully performed with a large amounts of thrombi extraction, obtaining adequate inflow (Figures 2 and 3). Post-operatively, a continuous heparin drip was maintained to achieve an aPTT of 50 to 70 seconds.
Thrombi removed from the brachiocephalic trunk and right common carotid artery (left) and right subclavian artery (right)
Three-dimensional reconstruction of before (left) and after (right) surgical thrombectomy
Post-op CT angiography showed small residual thrombus on the BC trunk and head CT showed recent right anterior thalamocapsular ischemic injury. A transthoracic echocardiogram confirmed intraventricular thrombi as the embolic source. The patient’s mental status and left sided motor function recovered progressively over time. Antithrombotic therapy was switched back to enoxaparin 60mg bid at the 2nd postoperative day. The patient was discharged from the hospital 25 days with a modified Rankin score of 2. At three-month follow-up, the patient remains well on anticoagulation with warfarin.
Discussion
As previously mentioned, up to 20% of patients do not have a successful recanalization after MT. This is associated with poorer outcomes and higher incidence of functional dependency, with only half of patients achieving good functional outcomes.2
Most patients without initial reperfusion maintain persistent occlusion without or with minimal recanalization at 24 hours.7 This is true regardless of intra-arterial tPA use, suggesting that clots not responding to MT also show low response rates to intravenous thrombolysis and spontaneous clot lysis.7
Reasons for reperfusion failure in MT are heterogeneous.7Main reasons are: difficult anatomical access, and hard/resistant occlusions - reflecting hard clots.6 When stent retrievers are deployed, the most common reason for failure is the inability to retrieve/dislocate the thrombus.7 Some authors hypothesize that the resistance of fibrin-rich clots to thrombectomy may be related to their mechanical properties, as they are stiffer than red blood cell-rich clots, resulting in a different interaction with the thrombectomy device.1,12
The composition of a thrombus is highly dependent on its source and aetiology.2 Cardioembolic thrombi have higher proportion of fibrin and white blood cells, which may be due to the longer time it has to mature in the heart chamber before embolization.2 This is associated with an increased degree of organization, making thrombi more resilient to mobilization.2,8 Hence, thrombus aetiology will influence the composition, rigidity, and friction of the clot and has been demonstrated to impact on the chances of a successful recanalization.6 The literature on thrombus burden (and successful MT recanalization) has not been able to show such a linear relationship; however, larger and more proximally located thrombi tend to have lower recanalization rate.2
In conclusion, the low rate of recanalization and poor clinical outcome after MT failure underlines the need for alternative rescue approaches. Surgical thrombectomy could represent a lifeline. More studies are needed to corroborate its efficacy in patients with anterior circulation’s AIS.