Background
The incidence of major vascular injuries after total hip arthroplasty (THA) reported is as low as 0.2% to 0.3%,1,2 with a higher occurrence of these in revision operations compared to primary ones.3 The most common vascular sequelae involve the external iliac artery with only a few cases reported in the literature.4 Due to subtle presentation, diagnosis of late vascular injuries after hip surgery is challenging, and the consequences of delayed treatment can be serious. In terms of pseudoaneurysm, the most frequent presentation is pain due to mass effect, particularly in cases of late diagnosis. Also, it may include symptoms of nerve compression, urological symptoms, thrombosis, edema and claudication due to ischemia.5 Less commonly, internal hemorrhage due to pseudoaneurysm rupture may occur.
Multiple mechanisms involved in vascular complications post THA have been described, such as entry of bone cement through a defective acetabulum into the pelvis causing thrombotic occlusion due to polymerization heat; intimate adhesion of artificial bone to the external iliac artery with subsequent wall rupture during replacement of the cup and intrapelvic cup migrations secondary to infection or mechanical loosening with consequent development of pseudoaneurysm.1,4 Usually, pseudoaneurysms are diagnosed based on imaging. The gold standard for diagnosis is conventional angiography, which is an invasive procedure. However, noninvasive diagnostic modalities such as ultrasonography, computed tomographic angiography (CTA) or magnetic resonance angiography should be included in the initial work-up, if possible.4 Although endovascular treatment of pseudoaneurysms may be preferred due to a reduction in operative risks,6 open repair may also be considered.7 Open techniques include pseudoaneurysm and artery resection associated with primary end-to-end anastomosis or graft interposition4 or, if the former is not feasible, pseudoaneurysm and artery resection associated with extra-anatomic vascular bypass with an autologous or synthetic graft.8,9 The choice of procedure must be made according to patient conditions, resources available and experience. Additionally, orthopedic intervention is frequently needed to prevent recurrence.
We present a case of a 65-year-old male patient in whom a false aneurysm of the external iliac artery developed 6 years after revision THA. The patient was managed with open repair and no complications were found after hospital discharge. This article demonstrates the importance of a regular and careful follow-up of patients submitted to hip surgery, in order to promptly identify late vascular complications.
The patient's consent for the publication could not be obtained since he died at the age of 70, due to an unrelated event.
Case report
An institutionalized, partially dependent 65-year-old male patient with a history of chronic alcoholism disorder was transferred to our emergency department from a primary care center due to sudden mass development on the right inguinal region associated with pain and fever starting two days before. No history of recent trauma was present. Inflammatory markers were elevated. All pulses were present bilaterally.
The patient had a prior history of right uncemented THA due to femoral neck fracture at the age of 57 (eight years before the index episode) and an additional operation for contralateral femoral neck fracture one year after. (Figure 1) Both occurred after an accidental fall from standing height. Three years following right THA, a revision operation with cementation of acetabular component was performed due to acetabular cup loosening following another fall.
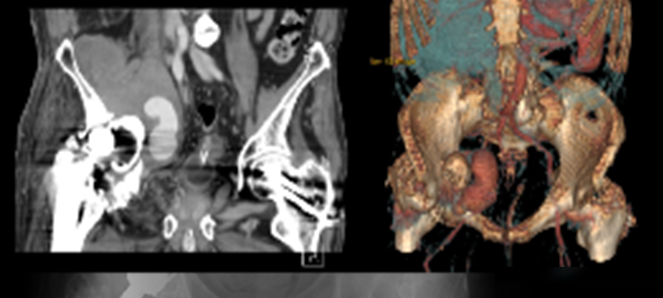
At admission, the patient performed the following exams: hip radiograph which showed right hip luxation, duplex ultrasonography which revealed right iliac fossa hematoma and venous diameter inferior to 2.5mm and CTA, which revealed a pseudoaneurysm of external right iliac artery approximately 10 cm in diameter and protruding acetabular cup (Figure 2).
The vascular surgery team performed urgent ligation and resection of the right external iliac artery and extra-anatomic bypass from left common femoral artery to right common femoral artery using a 6mm polytetrafluoroethylene (PTFE) graft on the day of admission. Additionally, the loosened protruding acetabular component was removed. Purulent material was sent to analysis and large spectrum antibiotic therapy was initiated (meropenem). An Escherichia coli sensible to all antibiotics was detected in wound drainage, with maintenance of antibiotic therapy.
Over the course of two weeks, there was a progressive decrease in purulent discharge and progressive healing. The patient was then transferred to the Orthopedics department. Removal of head and femoral stem and a Girdlestone procedure through Moore approach was then performed. Furthermore, fixation with 3 cables of extended femoral osteotomy using a transfemoral approach was done.
Right hip joint samples were collected and sent to microbiology, which revealed methicillin-resistant Staphylococcus aureus sensible to vancomycin and co-trimoxazole. Purulent drainage was seen on the distal third of wound during the first 10 days post orthopedic surgery, with gradual improvement after a three-week course of directed antibiotic therapy.
On discharge day, the patient was able to walk 60 meters with a stroller, hip flexion was limited to 60 degrees and no signs of wound infection were present. Pulses were palpable distally. At one-year the patient was pain-free, ambulatory with a walking aid and limping due to lower limb dysmetria. Maximum hip flexion was 70 degrees. There were no signs of recurrence of infection or further complications. Patient was lost to follow-up thereafter.
Discussion
Vascular injuries after THA are extremely rare events and commonly develop without symptoms, despite the possible development of severe complications.(10) If there is any suspicion of this complication, there should be a low threshold for imaging studies, shortly after the procedure or any time thereafter, to rule out possible vascular injury or other organ injury.2
The reported patient presented with a rapid growth inguinal tumefaction associated with pain and fever, six years after THA revision. Since the patient had a history of multiple falls due to excessive alcohol consumption and had abandoned follow-up, delayed diagnosis of hip prosthesis complications may have led to the present state. It was assumed, after initial diagnosis workup, that hip protrusion has developed over the years, resulting in pseudoaneurysm formation and later infection.
Concerning surgical treatment, even though ligation and resection are associated with significant risks, including major bleeding and damage to ureters adherent to artery wall,4 treatment of infected pseudo-aneurysms may include these, associated to an extra-anatomical grafting. Furthermore, the choice of arterial reconstruction with a synthetic or a venous conduit depends on extension of contaminated field and availability/quality of autologous graft. Also, patients who receive bypass surgery with a prosthetic conduit carry a higher incidence of graft infection and subsequent occlusion.9 In this case, the chosen technique was open repair with external iliac artery ligation and femoro-femoral crossover using PTFE, due to swiftness, lesion extension and contiguous orthopedic prosthesis infection. Moreover, autologous graft could not be used due to small diameter of the great saphenous vein (inferior to 2.5mm). The patient recovered ambulatory function, with no signs of complications described during follow-up.
Conclusion
With an increase of elderly population undergoing elective THA, it is important to be aware of possible late vascular complications, since there is a substantial risk of catastrophic consequences. This report advocates the need of patient education, clinician high index of suspicion and prolonged follow-up in patients who have undergone hip operations, in order to reduce morbidity and mortality associated with late vascular THA complications. Moreover, it is important to consider the different strategies and prepare adequately, since pathologic mechanism of vascular injuries and patient conditions are variable.