Introduction
Peripheral artery aneurysms (PAAs) represent 18% of all aneurysms.1,2 Upper extremity aneurysms are even rarer compared to other PAAs. In this subgroup, isolated true axillary artery aneurysms (AxAAs) are extremely rare (0.5-1% of all PAAs).1,3 Even if rarely symptomatic, they can evolve to a condition of upper limb disability and even irreversible ischemia with limb loss.2,4-6 Prompt diagnosis and treatment can avoid development of ischemic complications and limb loss or aneurysm rupture.5,6
Open surgical resection (OSR) followed by graft interposition is widely accepted as the first choice AxAA treatment. Endovascular exclusion with covered stents and, in selected cases, embolization has been reported as an alternative approach.2,5,6 Nevertheless, only case reports are available and long-term results are unknown. Thus, the best management of such aneurysms is still under debate.1 We present two clinical case reports of isolated AxAAs, treated successfully with OSR.
Case report
Case 1
A 23mm asymptomatic right saccular AxAA was detected in a 78-year-old man with a known thoracoabdominal aneurysm, who previously underwent endovascular repair due to an infrarenal aneurysm. Apart from chronic kidney failure and chronic coronary artery disease with concomitant dual antiplatelet therapy (DAPT) with acetylsalicylic acid and clopidogrel, the patient did not present any other comorbidities nor history of previous trauma or infections.
The physical examination revealed palpable ulnar and radial pulses, while neurological deficits of the upper extremity were not present. A pulsatile mass was palpable and localized in the right axillary cavum, but axillary fremitus was not identified. A computed tomography angiography (CTA) showed no suggestive signs of thoracic outlet syndrome (TOS). Resection and end-to-end interposition of an 8mm polyester graft was performed under general anesthesia (Figure 1). Due to a small anastomotic leak, surgical revision was performed. The patient was discharged on the seventh postoperative day and resumed DAPT. At one year follow-up, the patient was free of any complications, remaining with a patent arterial reconstruction and upper limb outflow.
An end-to-end interposition polyester graft is visible. Published with the kind permission of St. Franziskus Hospital
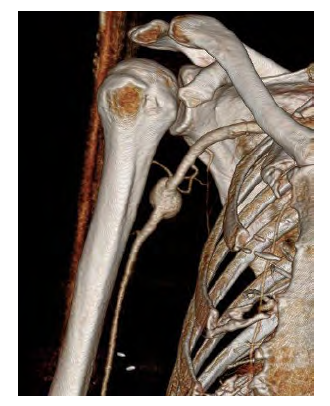
A 53-year-old-woman, with previous right breast cancer, surgically resected one year before (tumorectomy) and submitted to radiotherapy and ongoing hormone therapy (Tamoxifen) was identified at an oncological follow-up consultation with a right axillary mass on physical examination. Previous trauma or iatrogenic causes were excluded from her clinical history. She was asymptomatic regarding ischemic or neurological signs. A Duplex ultrasonography followed by a confirmatory CTA showed a 25mm sacular AxAA (Figure 2). No suggestive signs of TOS were depicted on the CTA.
A 25mm aneurysm of the right axillary artery is visible
The patient was submitted to OSR under general anesthesia, followed by interposition with an inverted great saphenous vein (GSV) graft through end-to-end anastomosis. A postoperative magnetic resonance angiography showed a patent reconstruction (Figure 3).
The postoperative course was uneventful and she was discharged at the fifth day on single antiplatelet therapy (acetylsalicylic acid). She presented at one year follow-up in good clinical condition and the US-scan confirmed complete patency of her right arm arteries.
Reconstruction of the axillary artery with a venous interposition graft is visible
Discussion
This report describes two cases of patients with axillary artery aneurysms treated with surgical repair. The first patient was an elder male with an axillary aneurysm probably with an age-related degenerative etiology, given the previous history of aneurysm disease. The second case regards a young woman with previous history of ipsilateral breast cancer.
AxAAs are rare compared to other PAAs.5 Moreover, considering that such aneurysms usually involve both the axillary and subclavian artery, the number of isolated AxAAs are even more rare1,5 with isolated AxAAs being usually pseudoaneurysms subsequent to trauma or iatrogenic punctures. True AxAAs are often associated to a history of previous blunt trauma or develop in consequence to repetitive extrinsic compressions (such as in TOS) or prolonged traction on the arm which lead to chronic stress to the arterial wall.3,5 Additionally, systemic (atherosclerosis) and connective tissue disorders (such as Marfan syndrome) can cause multiple aneurysms or isolated aneurysms affecting the axilliary artery8 as other causes include mycotic etiologies.7
In the female patient we reported presenting with an AxAA after previous ipsilateral breast cancer, radiotherapy was performed as a standardized cycle of six week after surgical excision of her breast cancer. Despite intraoperatively there were no signs of aggressive scar tissue explaining a mechanical cause for the development of the aneurysm, vasculitic cell-base damage due to radiation cannot be excluded.10 Unfortunately, a histological analysis of the aneurysm wall was not conducted.
AxAA treatment is still debated, but, according to the literature, OSR remains the first choice.1,2 Indication for repair is established for asymptomatic AxAA with diameters > 2cm, or in the presence of aneurysm-related symptoms (upper limb ischemia, embolization, pain or nerve compression symptoms).1
Surgical repair consists in resection and graft interposition or arterial ligation and subsequent bypass in a side-to-side/side-to-end configuration.1 While autologous graft (GSV) is preferred due to a reduced risk of infection, there is no evidence supporting this preference over other conduits such as Polytetrafluoretylene, polyester (Dacron) or biological grafts.9 Some authors discourage the use of arm veins, because their thinner wall may be prone to degeneration and rupture.2
Senarslan et al. reported two cases of isolated AxAAs in octogenarian patients; one patient was treated with aneurysmectomy and biological graft (Omniflow) interposition which remained patent at the sixth month of follow-up; the second patient underwent aneurysmectomy and GSV interposition which remained patent at one-year follow-up.9 In the female patient the choice of a GSV was taken because of age but also to diameter matching with the inflow/outflow arteries. The other patient received the biological graft, due to mismatch between the native 10mm-diameter axillary artery and the 3 to 4mm diameter GSV.
The axillary artery is regarded as a non-stenting zone, given the range of movement of the upper limb which with the effect of the costo-clavicular outlet can lead to arterial compression, torsion and kinking. Nevertheless, this represents also a challenge for surgical grafts too. Given the risk of stent fracture and ischemic complications, stenting should be specially avoided in in young active patients, practicing sports with repetitive movements shoulder movement.6
Surgical complications cannot be neglected, in particular wound infections, nerve lesions, bleeding and lymphocele are well described risks. During tissue dissection damage of median nerve and brachial plexus can occur, especially in case of massive bleeding or presence of extensive scar tissue. Other complications described in the literature are upper limb ischemia subsequent to post-surgical graft occlusion or embolization and cardiac complications.6 In one of our patients a surgical revision was necessary because of an anastomotic leak leading to a slightly prolonged hospital stay. Other less frequent complications are pneumothorax, chylothorax and oesophago-pleural fistula.6
Endovascular treatment is an alternative therapeutic option employing covered stent-grafts to obtain complete aneurysm exclusion specially reserved for patients unfit for open surgery and general anesthesia. Epstein et al. described a case of a 96-year-old woman with a 9x8 cm aneurysm treated via endovascular exclusion with stent-graft as a palliative treatment of her compressive symptoms, but only one-month long patency was reported.4 Van der Horst et al. described one case of an emergent axillary artery embolization with plugs, in a setting of ruptured AxAA. Their technical choice was due to the impossibility to perform an endovascular exclusion with a stent-graft, given the vessel tortuosity and the lack of an appropriate sealing zone. During the post-operative course, the compressive symptoms fully recovered after rehabilitation treatment.6 Nevertheless, complications related to endovascular treatment such as endoleaks, pseudoaneurysms, in-stent stenosis or occlusion and stent fracture have been reported, and long-term data is lacking.6,7
In conclusion, in our report, surgical repair of axillary artery aneurysms was associated with good short and mid-term results. Larger cohorts or registries are necessary to evaluate the different treatment modalities and their performance in the long-term.