Introduction
Peripheral arterial occlusive disease (PAOD) is a prevalent disease, affecting more than 200 million patients worldwide.1) This disease is a major cause of limb loss and it is responsible for functional incapacity and impaired quality of life.2)
Recently published studies on PAOD have revealed marked sex disparities in patient selection and treatment outcomes. Female patients tend to be older at the time of invasive treatment, have worse peri-operative morbidity and mortality rates, and they are also less likely to be taken optimal pharmacological treatment (OPT) at long-term follow-up, compared to male patients.3-10
Wang et al conducted a systematic review and meta-analysis about the effect of gender on outcomes after lower extremity revascularization, and they reported that female patients had an increased risk of death, need of amputation, cardiac events, and strokes after vascular interventions, compared to male patients.11) In fact, in a recent retrospective study with a population of 1 164 497 patients from 11 different countries, Portugal was highlighted as one of the countries with greater sex discrepancies related to PAOD treatment. The proportion of female versus male treated patients was the lowest in Portugal with only 23.1% (95% CI 22.4-23.9) of the patients treated for PAOD being women. Portugal was also the country with the higher ratio of female patients treated with endovascular procedures, with a sex difference of +14.90% (68.1% women vs. 53.2% men). In Portugal, there was a significantly lower proportion of female patients presenting with intermittent claudication and a higher proportion of octogenarians, compared to male patients. All these findings point to a discrepancy on the selection of female patients to PAOD treatment.8
The aim of this study was to analyze sex specific differences in the treatment of symptomatic PAOD, concerning different variables, in a single university hospital center, in Portugal.
Methods
Data on treatment of symptomatic PAOD patients from October 1st, 2020, to December 31st, 2021, were collected from clinical registries from a single university hospital center in Portugal.
Different variables were analyzed dichotomized by sex, such as differences in age, comorbidities, presentation (Leriche-Fontaine classification II, III or IV), treatment modality, mean length of hospital stay, and pharmacological treatment for PAOD at the time of invasive treatment. Differences in post-operative outcomes (90-day mortality and 90-day need of a major amputation) were also assessed. The comorbidities evaluated were history of hypertension, coronary artery disease, arrhythmia, valvular heart disease, cardiac insufficiency, dyslipidemia, diabetes, chronic renal disease, hemodialysis, stroke/transient ischemic attack (TIA), myocardial infarction, obesity, smoking (current or former), alcoholism (current or former), and chronic obstructive pulmonary disease (COPD). Treatment modalities included open surgical revascularization (OSR), endovascular treatment, hybrid surgery (revascularization combining open surgery techniques and endovascular interventions), primary major amputation, secondary major amputation, primary minor amputation, and secondary minor amputation. For the pharmacological treatment, we analyzed if the patients were taking antihypertensive drugs, statins, antiplatelet drugs and/or anticoagulant drugs.
This study was a retrospective analysis of longitudinal inpatient and outpatient data. Inclusion criteria were patients with ≥40 years; symptomatic PAOD patients with a Leriche-Fontaine classification degree II, III or IV; only patients treated with elective procedures; with a hospital stay for PAOD treatment between October 1st 2020 and December 31th 2021.
Descriptive statistics were used to describe the sample characteristics presented as frequencies, mean ± standard deviation (SD), as appropriate. Normality of the data was assessed using the Kolmogorov-Smirnov test. Independent t-tests (or its equivalent nonparametric test, depending on the normality of the data distribution), Fisher exact test and chi-square test (for categorical variables) were used to compare sample characteristics among the sex groups. Statistical analyses were conducted using the IBM Statistical Package for Social Sciences (SPSS) software v28, with the significance level set at 0.05.
Results
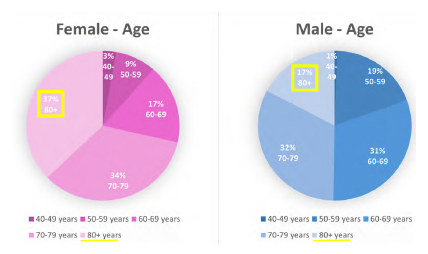
A total of 220 patients, 15,9% female and 84,1% male, were treated for PAOD, in the selected period. The mean age of this population was 70,2 years. Female patients were significantly older, with a mean age of 73.8 ± 11,2 years versus 69.5 ± 9,9 years in male patients (p=0.018). The proportion of octogenarians was also higher in the female group (37.1% versus 17.3% in the male group) (p=0.010). (Figure 1)
Graphic presentation of the age groups, dichotomized by sex. Proportion of octogenarians is highlighted with a yellow square.
Comorbidities distribution was similar between the two sex groups, except for known smoking history that was significantly more prevalent in men with PAOD, compared to women (49.7% male versus 8.9% female; p<0.001, Table 1)
Table 1 Characteristics of patients treated for DAOP from October 1st 2020 and December 31th 2021, dichotomized by sex
| Characteristic | Females | Males | P value |
| Mean age | 73.8 ± 11,2 years | 69.5 ± 9,9 years | 0.018 |
| Octogenarians | 37.1% | 17.3% | 0.010 |
| Hypertension | 68.6% | 66.5% | 1.000 |
| CAD | 17.1% | 23.2% | 0.516 |
| Arrhythmia | 17.1% | 14.1% | 0.602 |
| Valvular heart disease | 11.4% | 7.0% | 0.275 |
| Cardiac insufficiency | 8.6% | 12.4% | 0.589 |
| Dyslipidemia | 40.0% | 44.3% | 0.583 |
| Diabetes | 60.0% | 55.7% | 1.000 |
| Chronic renal disease | 34.3% | 20.4% | 0.207 |
| Hemodialysis | 22.9% | 10.8% | 0.111 |
| Stroke/TIA | 11.4% | 9.2% | 0.771 |
| Heart attack | 14.3% | 13.5% | 1.000 |
| Obesity | 11.4% | 11.9% | 0.796 |
| Smoking | 8.9% | 49.7% | <0.001 |
| Alcoholism | 2.9% | 8.1% | 0.480 |
| COPD | 0% | 3.8% | 0.605 |
Table presentation of the mean age and comorbidities, dichotomized by sex. CAD: coronary artery disease; TIA: transient ischemic attack; COPD: chronic obstructive pulmonary disease
A lower percentage of women were treated for intermittent claudication (Leriche-Fontaine classification II in 3% of women versus 6% of men) and they were more often treated at a more advanced stage of the disease with trophic lesions (Leriche-Fontaine classification IV in 91% of women versus 74% of men) (p=0.088, Figure 2)
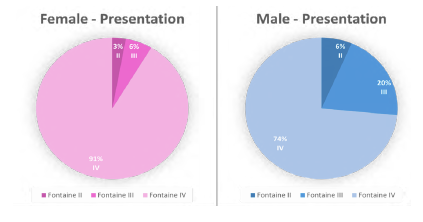
Figure 2 Clinical presentation of patients treated for DAOP, from October 1st 2020 and December 31th 2021.
Graphic presentation of the clinical presentation grade according to the Leriche Fontaine classification system, dichotomized by sex
The anatomic pattern of the lesions were similar between both genders, without significant differences (aortoiliac or aortoiliac with femoropopliteal lesions in 20.0% versus 24.6% (p=0.56), femoropopliteal lesions in 45.7% versus 46.4% (p=0.94), and tibioperoneal or femoropopliteal with tibioperoneal lesions in 34.3% versus 29.0% (p=0.56), for women versus man respectively).
Female patients were more frequently treated with endovascular procedures (40% versus 26% treated with OSR), with the opposite occurring for male patients (42% treated with OSR versus 32% treated with endovascular procedures). Hybrid surgery was performed in 8% of the female versus 5% of the male patients. Primary major amputation was significantly more frequently performed in women with PAOD than men (14% versus 3%; p=0.010, Figure 3).
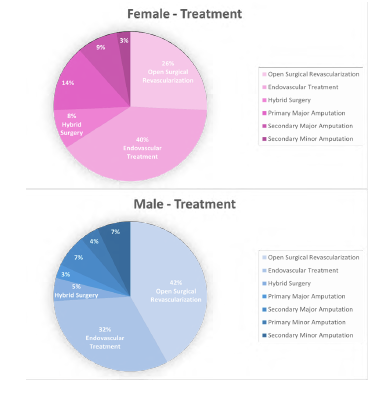
Figure 3 Treatment modalities for patients treated for PAOD, from October 1st 2020 and December 31th 2021, dichotomized by sex
Women were less likely to be taken statin as part of PAOD OPT (only 65.7% of female patients were taking this medication, compared to 77.8% of male, with a total difference of -12.1%) (p=0.134, Figure 4).
Length of hospital stay was similar between the two sex subgroups and the total mean duration of hospitalization was 15 days. 90-day mortality rate was significantly higher in women (17.1% versus 6.5% in men; p=0.045). Although female patients had a higher percentage of secondary major amputations at the time of data extraction (9% versus 7% in male patients), they seemed to have a lower 90-day major amputation rate after revascularization (5,7% versus 11,4% in men; p=0.545, Table 2)
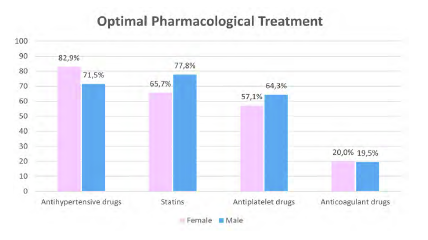
Figure 4 Optimal pharmacological treatment of patients treated for PAOD, from October 1st 2020 and December 31th 2021, dichotomized by sex.
Graphic presentation of the optimal pharmacological treatment, dichotomized by sex
Table 2 Statistical analyses of the results of patients trated for PAOD, from October 1st 2020 and December 31th 2021, dichotomized by sex
| Characteristic | Females | Males | P value |
| Leriche-Fontaine | |||
| II | 3% | 6% | 0.088 |
| III | 6% | 20% | |
| IV | 91% | 74% | |
| Intervention | |||
| Endovascular | 40% | 32% | 0.245 |
| OSR | 26% | 42% | 0.135 |
| Hybrid | 8% | 5% | 0.403 |
| Primary major amputation | 14% | 3% | 0.010 |
| Primary minor amputation | 0% | 4% | 0.588 |
| Secondary major amputation | 9% | 7% | 1.000 |
| Secondary minor amputation | 3% | 7% | 0.188 |
| Medical treatment | |||
| Antihypertensive drugs | 82.9% | 71.5% | 0.397 |
| Statins | 65.7% | 77.8% | 0.134 |
| Antiplatelet drugs | 57.1% | 64.3% | 0.338 |
| Anticoagulant drugs | 20,0% | 19,5% | 0.813 |
| Postoperative outcomes | |||
| 90-day mortality rate | 17.1% | 6.5% | 0.045 |
| 90-day major amputation rate | 5.7% | 11.4% | 0.545 |
OSR: open surgery repair.
Discussion
The results of this retrospective observational study agreed with findings from previous published articles, as they highlighted significant sex discrepancies in PAOD treatment.
Women with PAOD tend to present at an older age and at a later stage of the disease, compared to their male counterparts.5,8,9,12,13) In our study population, we found that women were significantly older with a mean age of 73.8 years at the time of treatment, there was a higher proportion of octogenarians in the female group and most women were offered treatment at a more advanced stage of the disease. However, this difference seems to be related to women being older at time of treatment, since a subgroup analysis of the octogenarians showed that the majority of both male and female patients were treated at Leriche-Fontaine classification stage IV with trophic lesions (88.9% versus 92.3% respectively), with none treated for intermittent claudication in both subgroups. Other articles also found similar disparities in PAOD clinical symptoms at presentation between both genders.8,12,13) In a study with a population of 18 742 patients with PAOD, Sigvant et al reported that men were more frequently revascularized for intermittent claudication than women, who presented more often with ischemic rest pain or trophic lesions.14) In a recently published meta-analysis, with a study population of 1 929 966 patients, Porras et al concluded that women with PAOD present more often with rest pain and atypical leg symptoms, and less often with intermittent claudication.15
On the other hand, it has been shown that men with symptomatic PAOD although younger, have a higher burden of cardiovascular comorbidities compared to women.16) In our results, there were no significant differences in the prevalence of comorbidities between both sexes, but female patients were less often current or former smokers. In a study of 26 750 endovascular procedures for PAOD, Ramkumar et al also found that women were less likely to have a history of smoking.12
Another sex discrepancy in PAOD, discussed in prior investigations, is the chosen treatment modality, with women being consistently less likely to undergo OSR when compared to men.3,5,8,12-14) Accordingly, we found that in our center, female patients tend to be revascularized with endovascular interventions, opposite to male patients that were more often treated with OSR. Although we can only hypothesize about possible explanations for these findings, the fact that women are more frequently older at time of treatment and at a more advanced stage of the disease could be a reason for the preferential selection of endovascular treatment, which is less invasive. In fact, the anatomic pattern for the peripheral arterial lesions seemed to be a non-significant factor to justify these disparities between genders.
The OPT recommended for PAOD include lipid lowering drugs, antihypertensive drugs (if history of hypertension) and antiplatelet drugs.17,18) In a longitudinal study, Peters et all found that OPT for PAOD was less prescribed for female patients, specially statins, with prescription rates of 56.2% for men and 49.8% for women.9) A higher proportion of cardiovascular comorbidities diagnosed in men and less awareness for the diagnosis of PAOD in women, could be a reason for higher prescription rates of statins to male patients in outpatient care.9,16 We found that women in our cohort were also less likely to be taken lipid lowering drugs with a prescription rate of statins of 65.7%, compared to 77.8% of male patients, with a gap of -12.1% between both groups.
Results about sex disparities in outcomes after PAOD treatment have been contradictory in previous studies. Some studies showed a tendency for worse outcomes at short-term follow-up after treatment for female, compared with male patients. However, better long-term outcomes for women have also been reported.5,19,20) We analyzed mortality rates and major amputation rates as post-operative outcomes with a follow-up period of 90 days, and we found that female sex was associated with higher post-operative mortality rates, but lower major amputation rates. Higher mortality rates in women could be explained by their advanced age and disease stage at time of treatment. Lower major amputation rates after revascularization for females could be associated with women being more likely submitted to primary major amputation, lowering the need of major amputation in the post-operative period.
In a recent published article with data from 11 different countries, Behrendt et al highlighted Portugal as one of the countries with more significant sex discrepancies in PAOD treatment, with women being less likely revascularized with OSR, less likely treated for intermittent claudication, and older with higher proportion of octogenarians. Although the heterogeneity between both sex groups, these findings point to a patient selection bias for PAOD treatment in Portugal. Our results, based in data collected from a single hospital center in Portugal, were in agreement with these statements with similar differences found between both genders.
Further research is warranted to better understand the role of patient sex in PAOD treatment and to establish the influence of sex discrepancies on choice of treatment modalities and post-operative outcomes.
This retrospective study has some limitations. Firstly, our sample size was small which could make it more difficult to determine with certainty if a particular outcome is a true finding. Secondly, the heterogeneity and different mean age between both sexes could have interfered with the results. Finally, data were extracted retrospectively from clinical records, and it could have been missed information (for example, missed data from smoking habits or other comorbidities).
Conclusion
In this retrospective study from a tertiary center in Portugal, evidence was found for remarkable sex discrepancies in the treatment of PAOD. Women were significantly older, significantly less like to have smoking history, significantly more likely to be submitted to primary major amputation and had significant greater mortality rates at 90-day follow-up. Women also showed a tendency to be treated at a more advanced stage of the disease, more frequently with endovascular procedures than OSR, and seemed to be less likely taken statins as part of OPT. This study brings awareness to the scientific medical community for sex disparities in the management of patients with PAOD. Future research is needed to better understand the impact of selection sex bias in PAOD treatment outcomes and to understand possible underlying reasons for these sex discrepancies and differences in practice.
Acknowledgements: None
Conflicts of interest: None
Funding: None