Introduction
The Corona Virus Disease of 2019 (COVID-19) has had a major impact in clinical practice across all areas of medical care. During the initial stage of the pandemic, several countries saw their elective surgical activity restricted, with one study estimating that 28 404 603 operations were canceled or postponed globally during the 12 weeks of the COVID-19 peak(1). Several algorithms were proposed trying to stratify surgery timing according to underlying condition(2-4). Recognition that patients presenting with simultaneous COVID-19 infection had significantly worse operative outcomes(5) increased the concern about ideal surgical timing. For Vascular Surgery, the American College of Surgeons proposed a triage system for vascular patients(6) to help establish the urgency of the underlying pathology and to aid in decision making.
During the mandatory confinement period most elective surgery in Portugal was canceled, in an attempt to reduce hospital infection rates, to preserve ICU beds to accommodate COVID-19 patients, to diminish the use of protective equipment in order to allocate it to emergency services and to increase the number of medics available to cover other critical activities during peak pandemic. Emergency service became largely dependent on COVID-19 screening, and referral even in this setting was consequently delayed. Furthermore, our general perception was that patients were reluctant to resort to medical aid, both in the emergency setting and as outpatient consultations because of concern of potential COVID-19 nosocomial infection. As a final result, patients presented later, and with more severe clinical pictures with outcomes being arguably worse.
Our department is a tertiary referral center serving a population of 1.285.600 people for all vascular activity, with an added 976.019 people when considering 24/7 emergent care (as accounted in data from 2017)(7). The purpose of this study was to evaluate surgical activity in our department, during the national emergency state and to compare it with the same period of the prior two years in order to conclude on whether the clinical presentations were different and if outcomes had changed.
Material and methods
The authors declare that they have followed the protocols of their center on the publication of patient data and comply with the Helsinki declaration on research ethics.
A retrospective analysis of the patient charts that underwent surgery in the months of March and April of the year 2020 (referred to as COVID Period - CP) was conducted and compared to the same period on the previous two years (referred to as Non-COVID Period - NCP). All of the patients admitted in this period of 2020 were through the emergency department or through urgent consultations. All patients had a COVID-19 test prior to or at the time of admission.
The primary endpoint was death at 30 days or during hospital stay and we analyzed the absolute number and proportion of patients treated per pathology (Aortic and iliac aneurismal disease - including thoracic, abdominal, iliac and thoracoabdominal aneurisms - arterio-venous malformations, cerebrovascular disease, peripheral arterial disease (PAD) of the lower limbs, PAD of the upper limbs, venous disease, deep venous system pathology, embolic acute limb ischemia - acute thrombotic limb ischemia is included in peripheral arterial disease of the lower limbs, since it is frequently difficult to adequately differentiate these acute events from those classified as chronic limb threatening ischemia due to coding - non-aneurismal aortic pathology, non-atherosclerotic arterial disease, peripheral arterial aneurysms, renal ischemia and renovascular hypertension, chronic kidney disease, tumors, vascular surgery complications, vascular trauma and visceral arterial pathology), admitted for Chronic limb threatening ischemia (grades 4 to 6 of Rutherford), submitted to amputation, amputation level (minor for toes or foot amputations, major for bellow and above the knee amputations), the type of surgery performed (endovascular, conventional or hybrid), the time of hospital stay (in days) and in-hospital re-intervention rate (any surgical procedure).
Statistical analysis was performed using the IBM SPPS Statistics 24 Software. Pearson's chi-squared test was applied to compare categorical data. The significance threshold was set at a p value of 0.05.
Results
There were 98 patients submitted to surgery in the CP, compared to 286 in the NCP with 133 patients submitted to surgery in 2018 and 153 submitted to surgery in 2019. There was no significant difference in the age of the patients between groups, median 70 years (17-98) in the CP and 69 (17-92) in the NCP (p=.13). There was a predominance of male patients in both groups, with 76% (74/98) of male patients in the CP and 70% (196/282) in the NCP (p=.26). All patients were tested for COVID prior to or at the time of admission and all but one were negative. Emergent operations were undertaken without COVID test results with presumptive precautions, with all tests being negative in those cases.
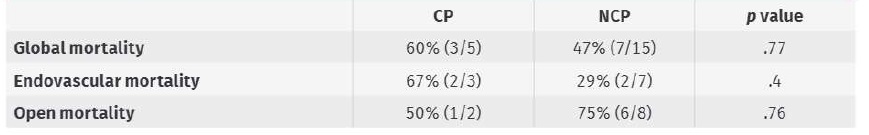
PAD of the lower limbs was the main cause of admission, corresponding to 75% (73/98) of patients admitted during the CP, compared to 48% (137/286) in the NCP, p=.02. PAD was the only pathology with a percentual and absolute increase in the CP (Figure 1, Table 1). The second most common cause of admission was Aortic and iliac aneurismal disease with 5% (5/98) of admissions in the CP compared to 13% (36/286) in the NCP, p=.05. All admissions in the CP corresponded to ruptured aneurysms, as opposed to 42% (n=15) in the NCP, p=0.2. The third most common cause was embolic Acute Limb Ischemia with 4% (4/98) of cases in the CP, similar to 6% (18/286) in the NCP, p=.4. Hemodialysis access complications also corresponded to 4% (4/98) of cases treated in the CP vs. 5% (15/286) in the NCP, p=.6. Cerebrovascular disease corresponded to 3% (3/98) of cases in the CP, a non-significant decrease from 7% (19/286) in the NCP, p=.2.
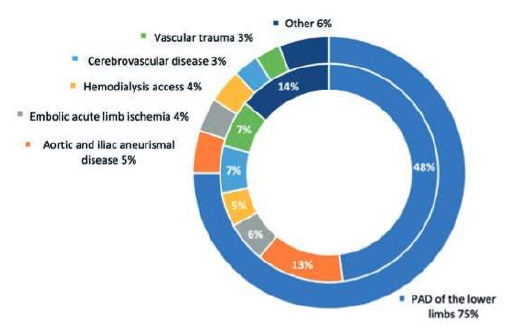
Figure 1 Patients treated according to pathology group in the CP (outer circle) and NCP (inner circle). “Other” represents groups with less than 3% of total admissions.
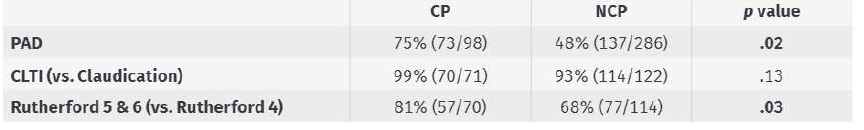
Among patients admitted for PAD, Chronic limb threatening ischemia (CLTI) represented 99% (70/71) of admissions in the CP, with a non-significant (p=.10) increase from 93% (114/122) in the NCP. There was however a statistically significant increase in Rutherford grades 5 and 6 at admission for patients with CLTI, with 81% (57/70) in the CP vs. 68% (77/114), p=.03 (Table 2).
There was no significant difference in amputation rate for patients treated with PAD, with 35% (25/71) in the CP and 40% (49/122) in the NCP, p=.49. There was a 13% increase in major amputations, 52% (13/25) of all amputations in the CP and 39% (19/49) in the NCP, which did not reach significance (p=.27).
For Aortic and iliac aneurismal disease there were no elective procedures during the CP. There were five urgent procedures, corresponding to three ruptured infrarenal abdominal aneurysms, one ruptured thoraco-abdominal aneurysm and one ruptured iliac aneurysm. There no asymptomatic patients identified with large thoracic or abdominal aneurysms (> 6.5cm) that needed urgent repair during the CP. Three patients underwent EVAR and two open surgery. There was a 60% (3/5) mortality rate (Table 2) during this period, 67% (2/3) for endovascular repair and 50% (1/2) for open repair. Mortality for urgent repair in the NCP was 47% (7/15), 29% (2/7) for endovascular repair and 75% (6/8) for open repair. The percentual increase in mortality from emergent endovascular repair during CP corresponded to two patients submitted to EVAR with very advanced age (92 and 98 years old). Despite the percentual increase there were no statistically significant differences for mortality in urgent aneurysm repair between groups (p=.77 - Table 3). There were 36 cases of Aortic and iliac aneurismal disease in the NCP, with 15 being urgent cases and the remaining elective cases that comprised TEVAR, aorto-iliac EVAR, and FEVAR, and open surgery repairs. Mortality for elective repair in the NCP was 5% (1/21). In the urgent repair group of the NCP two ruptured thoracic and 11 infra-renal abdominal aneurysms are included, as are one ruptured EVAR graft and one primary aorto-esophageal fistula. Seven patients underwent endovascular repair and eight open repair.
In the Hemodialysis access group, in the CP all the patients were treated for life-threatening access complications. No difference was observed between the CP (4% (4/98) in the CP vs. 5% (15/286) in the NCP, p=.6) and NCP in this category.
Among the three patients admitted for Cerebrovascular disease, two had symptomatic carotid stenosis (in the 14-day therapeutic window) and one had an asymptomatic high-grade carotid stenosis.
Overall, there was a decrease in proportion of conventional open surgery, with 43% (42/98) of cases on the CP vs. 57% (164/286) in the NCP, p=.04. Conversely, both endovascular and hybrid procedures increased - endovascular from 37% (107/286) in the NCP to 48% (47/98) in the CP, and hybrid from 5% (15/286) to 9% (9/98).
In-hospital reintervention rates was 18% (18/98) of patients in the CP and 16% (45/286) in the NCP, p=.58. There was no difference in 30-day or in-hospital mortality, 5% (5/98) in the CP against 5% (13/286) in the NCP, p=.88. There was also no significant difference in length of hospital stay, with median 10 (0-77) days in the CP and 7 (0-118) days in the NCP (p=.6).
Table 1 Absolute number of patients treated by category. Although the proportion of patients changed, the most frequently admitted remained the same
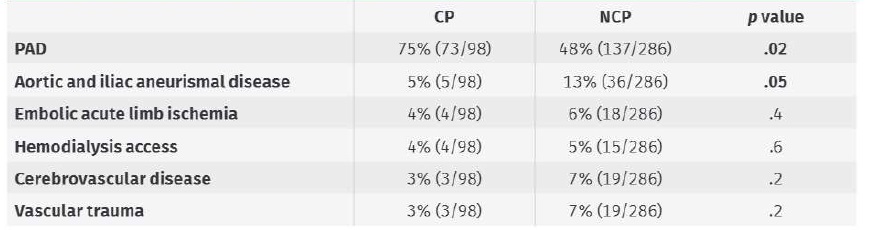
Table 2 Proportion of patients admitted with Peripheral Arterial Disease (PAD), Chronic limb threatening ischemia (CLTI) and Rutherford grades 5 and 6 in the COVID Period (CP) and Non-COVID Period (NCP). Percentage and partial and total number of patients per category is presented
Discussion
As it would be expected there was a reduction in the number of patients operated on, mainly because of severe restrictions to elective activity. PAD remained the main cause of admission, but the proportion of patients admitted for PAD increased, which can be explained both by lower admissions in other pathology groups, and by a slight increase in the absolute number of patients admitted in this group. Patients admitted for PAD were almost exclusively patients in CLTI, both before and during the pandemic, but there was an increase in grades 5 and 6 of Rutherford, which supports the hypothesis that patients were presenting later with more severe clinical pictures, and extensive wounds.
All other pathology groups, including the second and third most common causes showed a significant decrease in the number of cases, and constituted mainly emergency surgical cases, as represented by ruptured aortic aneurysms (second most common cause), embolic acute limb ischemia and life-threatening hemodialysis access complications (third most common causes).
The lack of difference in the Hemodialysis access group is explained by a low number of patients submitted to routine fistula creation in our institution with most interventions being related to complications or complex hemodialysis accesses.
Concerning Cerebrovascular disease, the lack of difference between the CP and NCP is explained by similar surgical criteria in both periods.
An international survey conducted by the university of Singapore reported that 91% of physicians replied that at least some if not all elective vascular surgery in their hospitals was canceled but that 92% were still performing emergency surgery(8). Emergency vascular surgery in the COVID-19 period was categorized by different articles(6, 9-11). In CLTI and acute limb ischemia, ruptured aortic aneurisms, trauma surgery, acute aortic syndromes, symptomatic carotid stenosis, acute mesenteric ischemia, symptomatic peripheral arterial aneurysms and vascular access for hemodialysis, endovascular procedures were favored over open repair whenever possible to shorten hospital and ICU stay. These data are in line with the surgical activity of our department during the same time period.
Given the increase of advanced grades of ischemia at presentation, it would be expected that a larger proportion of patients needed amputation surgery or at least reintervention, but that did not happen in our sample. Both amputation and major amputation rates had a non-statistically significant increase as did reintervention rate.
One study performed in the Netherlands with a similar design to ours reported a significant increase in patients admitted for CLTI with Rutherford grades 5 and 6 (comporting 90% of cases) but an equal increase in major limb amputations from 18 to 42%, p=.01(12). These results were in conformity with those of another study conducted in Italy, which reported an increase in major limb amputation of 50%(13).
Elective aortic and iliac aneurismal surgery did not happen during COVID-19 period and only ruptured aneurysms underwent surgery during this time. Despite a percentual increase in mortality in urgent aortic aneurysm repair, it did not reach significance. Ruptured aneurysms correspond to emergent cases that do not need to wait for COVID test results before admission to operating room. This fact and the approach protocol for this pathology in our department can explain the absence of differences in outcomes.
Conventional surgery decreased and hybrid and endovascular surgery increased, which can be related both to the nature of the pathology treated and to the global perception that endovascular procedures carry a lesser risk of COVID-19 transmission during surgery, both because of less frequent need for general anesthesia (and as such, intubation) and the avoidance of electric thermocautery which has been shown in some reports to increase the spread of viral particles(14). Being minimally invasive, endovascular approaches also have the advantages of a faster recovery time and less frequent need of ICU beds for post-operatory recovery and monitorization. However, length of hospital stay, and mortality also remained the same.
Our results confirmed the perception that patients did arrive in more severe states of ischemia and with more severe wounds, but that did not ultimately worsen prognosis.
Conclusions
Restrictions to non-urgent care and on elective procedures during the COVID-19 emergency state in our center manifested mainly in the type of pathology treated and the number of patients operated on. CLTI corresponded to the majority of admissions, in a higher proportion than in corresponding previous periods of time. The greater severity of the underlying pathology, manifested by more extensive wounds and advanced CLTI at presentation, did not increase mortality nor was reflected on significantly more major limb amputations.