Introduction
Underlying atherosclerosis in abdominal arteries is a common situation in aging patients with polymorbidities. However, it also occurs in younger people with other etiologies such as prothrombotic coagulation abnormalities or arterial dissection1.
Atherosclerosis of the mesenteric arteries can remain asymptomatic for a long time and manifests when an acute medical or surgical event occurs. This insidious natural history happens because the organism adapts itself by collateral circulation, and symptoms only become evident if a precipitating factor befalls2. Examples of precipitating factors are low arterial blood flow resulting from heart failure, dehydration, or complete arterial occlusion by in situ thrombosis or embolization.
When intestinal surgery is needed, the suspicion and confirmation of poor visceral irrigation preclude a different treatment schedule that includes arterial revascularization before the gastrointestinal procedure3. By this way, we can provide the ideal therapy with excellent surgical results and good patient quality of life.
On this subject, two cases are presented in which the close collaboration between general surgery and vascular surgery have led to successful therapy outcome.
Clinical-case 1
A 48-year-old female patient was admitted to the emergency department with hypogastric abdominal pain accompanied by nausea and postprandial vomiting. These complaints arose in the past year with a gradual increase of severity in the last 15 days before resorting to the hospital. In her history, she mentioned cardiovascular risk factors (smoking, hypertension, hyperlipidemia). The workup performed revealed leukocytosis, elevated lactate, and Computed Tomography (CT) images compatible with occlusion of the superior mesenteric artery (SMA) and stenosis of the celiac trunk associated with thickening of the intestinal walls, without signs of pneumatosis. She underwent exploratory laparotomy with SMA thrombectomy, retrograde open mesenteric stenting (ROMS) at the artery ostium, and closure of the SMA arteriotomy with the saphenous vein. Intraoperative, 40 cm of proximal jejunum and 20cm of distal ileum were viable, and the remaining intestine overall showed signs of poor perfusion but without evidence of necrosis. For that reason, a second-look laparotomy was scheduled for the following day. In the postoperative period, the patient started an infusion of unfractionated heparin. On relaparotomy, ischemia progression was visible, which required extensive enterectomy with jejunoileal anastomosis (preserving 60 cm of the jejunum and 20 cm of the ileum). She maintained the heparin, which was later changed to low molecular weight heparin. The postoperative period was initially performed in an intensive care unit. It was necessary to control renal dysfunction, hypertension, acute intestinal failure, and central venous catheter sepsis. She was discharged 51 days after the operation.
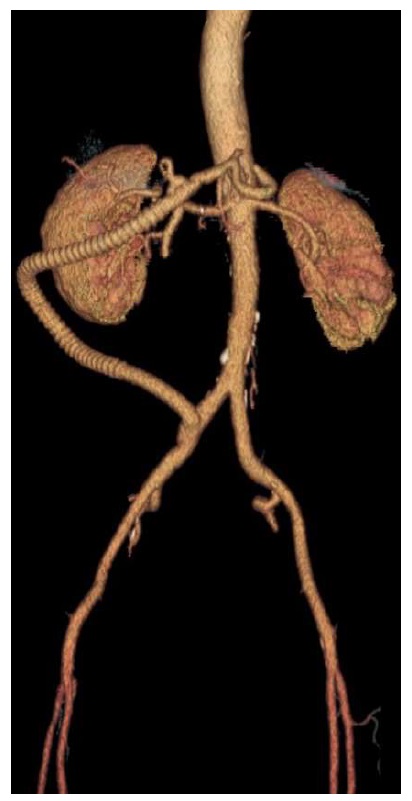
In the following three months, she tolerated food well. However, she needed to resort to the hospital again due to a one-month history of postprandial vomiting and abdominal pain worsening in the last 15 days. A CT angiography (CTA) was performed, showing a SMA stent thrombosis, compromised distal flow, and thickening of the small bowel with a stenosis in the preview entero-enteric anastomosis (figure1).
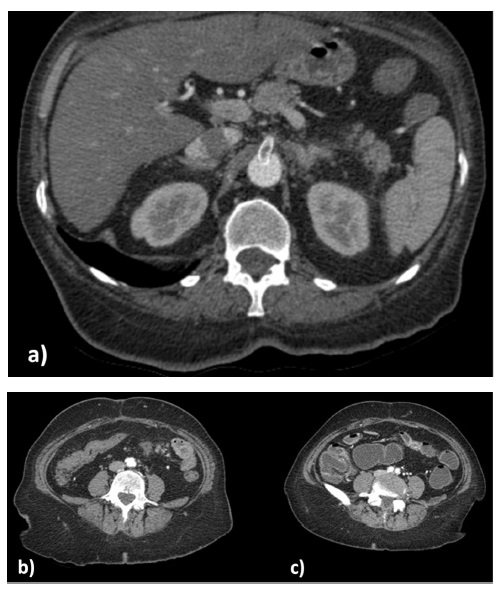
Figure 1 a) SMA stent thrombosis; b) inflammation and edema of intestinal wall; c) stenosis of 5 cm ileon extension.
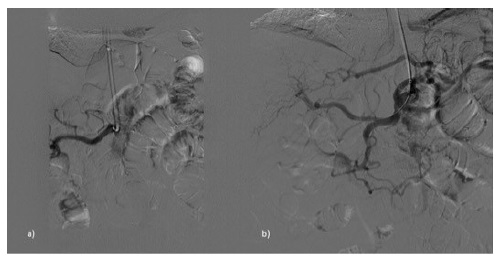
She underwent an iliohepatic bypass with an 8mm PTFE graft (figure 2). Postoperatively, there was a suspicion of vascular prosthesis infection; however, the patient fully recovered under antibiotic treatment. She was discharged after 51 postoperatively days. A study of prothrombotic factors was performed only with the JAK2 V617F mutation being identified.
At one-year follow-up, she was asymptomatic without ileal stenosis identified in the CT scan.
Clinical-case 2
A 76-year-old-man was proposed for revascularization due to chronic limb-threatening ischemia (CLTI) with rest pain on the right foot. CTA showed significant aortoiliac and femoropopliteal disease. The patient did not have clinical conditions for major aortic surgery or anatomical conditions for endovascular treatment. He was submitted to a right axillofemoral bypass with a sequential popliteal bypass. He needed two blood transfusion units (one during the procedure). Due to the suspicion of nosocomial respiratory infection, the patient completed one week of antibiotic therapy with piperacillin + tazobactam.
At the time of discharge (26 days after the admission), he was clinically stable, apyretic with decreasing inflammatory markers, and surgical wounds with good healing without inflammatory signs.
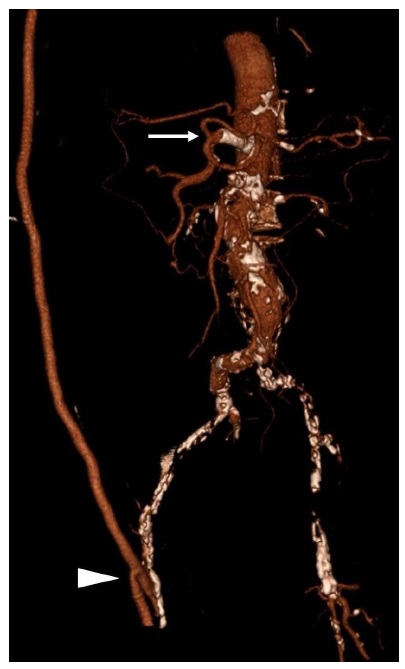
He was readmitted to the hospital 32 days after the discharge with abdominal pain, vomits, and constipation. Physical examination revealed abdominal pain and tenderness to palpation. CT scan showed ileum adhesion to a thickened cecum; the celiac trunk had a severe degree of stenosis, and the SMA was occluded. Analytically presented leukocytosis and an elevated c-reactive protein. He initiated antibiotic therapy (piperacillin + tazobactam) and parenteral nutrition. Seven days later, he was submitted to a celiac trunk primary stenting with a balloon-expandable stent (figures 3 and 4). Five days after the vascular procedure he was submitted to a right colectomy with segmental enterectomy by colorectal surgeons (figure 5). The postoperative period was uneventful, and he was discharged on the ninth day after the surgical procedure. At a 6-month follow-up, the patient remains without any gastrointestinal symptoms.
Discussion
Atherosclerosis in splanchnic arteries (the celiac trunk, superior mesenteric artery, or the inferior mesenteric artery) is relatively common in older age groups4. Due to the redundancy of the blood supply in the mesenteric territories and the fact that atherosclerosis usually has a slow progression with the development of an extensive network of collateral arteries, the patient can be asymptomatic for a long time. In severe cases, usually when two or more of the mesenteric vessels are affecting the patient can present with postprandial abdominal pain and severe malnutrition. When an acute medical or surgical event occurs (i.e., heart failure, dehydration, or complete arterial occlusion by in situ thrombosis or embolization), the patient can present with acute or acute-on-chronic mesenteric ischemia a much dreaded, and often lethal complication usually associated with bowel infarction1,2,5.
The suspicion of underlying atherosclerosis in the splanchnic arteries is fundamental for planning and resolving the present clinical cases.
Symptomatic patients with CMI should be treated without much delay because of the higher risk of progression to acute mesenteric ischemia. It is estimated that symptoms of CMI are previous present in 43% of patients who develop acute mesenteric ischemia (AMI)6. This aspect was illustrated in our first case. The diagnosis of chronic mesenteric ischemia is made belatedly, although the patient was symptomatic, leading to an acute and severe event. The patient already manifested symptoms of chronic mesenteric ischemia such as abdominal pain and vomiting that worsen and lead to dehydration and complete arterial occlusion by vascular thrombosis. In the second event of this patient, the diagnosis of mesenteric vascular insufficiency and SMA occlusion was timelier, which allowed an effective vascular procedure without the need for an extensive enterectomy.
On the other hand, in asymptomatic patients with colorectal surgery planned, the need for prior revascularization must also be considered. This clinical scenario is what happened in the second case. The patient was asymptomatic, but the low arterial blood flow leads to an intestinal obstruction caused by cecum wall ischemia. In this case, the diagnosis of intestinal obstruction provoked by cecum wall ischemia was also not the first hypothesis. However, it helped the suspicion of severe atherosclerosis and lower limb revascularization, which led to planning celiac artery revascularization before right colectomy with two enterectomies. It is estimated that 25% of patients admitted for lower extremity arteriography have significant stenosis of the mesenteric arteries7.
Vascular surgery is a crucial point in the treatment plan of these two patients with mesenteric ischemia. Despite the growing bibliography on this subject, many controversies persist regarding the optimal vascular treatment8,9. These controversies include the type of surgical repair endovascular vs. open bypass (antegrade/ retrograde) and the number of arteries that should be treated (single- vs. multiple-vessel reconstruction)10. Regardless of the complexity of the vascular intervention, the mesenteric revascularization was essential in both cases.
The procedure was made in the emergency room by an open approach in the female patient: superior mesenteric artery (SMA) thrombectomy and retrograde stent placement at the occlusion site. The procedure was only partially effective, and four months later, she presented SMA thrombosis at the stent level. Maybe the presence of the JAK2 V617F mutation contributed to the new thrombotic event11. In this phase, the solution to the problem was made with an open ileohepatic bypass. A resolution of ischemic ileal stenosis occurs without the need for enterectomy. This way, it was possible to avoid another intestinal surgery and the risk of short bowel syndrome. In the man patient submitted to a right axillofemoral bypass with a sequential popliteal bypass already with CMI and the need for gastrointestinal revascularization before colorectal surgery; the option was the celiac trunk primary stenting. This solution allowed a safe and effective elective colorectal intervention.
Conclusion
Chronic mesenteric ischemia associated with atherosclerosis of splanchnic arteries can be a considerable problem with harmful consequences, especially if its existence is not suspected. This pathology is often underdiagnosed by the lack of attention from attending physicians, given that the symptoms progress slowly. An active investigation must be performed whenever the patient has symptoms or has several risk factors and needs gastrointestinal surgery. When severe atherosclerosis is diagnosed, the revascularization before gastrointestinal surgery may provide excellent results. Two cases on this subject are reported showing that close collaboration between general surgery and vascular surgery is essential for a successful therapy outcome.