Case report
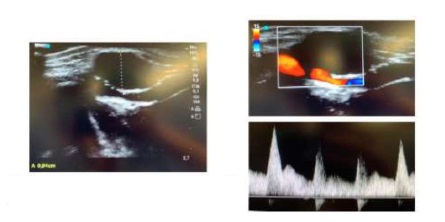
We report the case of a 44 year old healthy male, presenting with a 2 cm pulsatile, painless mass in the distal portion of the radial side of the forearm on the left wrist, with no previous history of trauma or percutaneous procedures. Doppler ultrasound (DUS) revealed a hypoechogenic mass involving the arterial wall that caused a lumen reduction of 50%. Lesions in other arterial segments were excluded using DUS. These findings were compatible with the diagnosis of ACD and patient was elective for surgery. The involved arterial segment was resected and an end-to-end anastomosis was performed. Pathology confirmed the presence of a cystic mass with mucinous content. During follow-up, the patient remained asymptomatic and DUS showed patency of the artery and no signs of recurrence.
Discussion
This rare entity should be suspected when a pulsatile mass is noted in the radial artery because an early diagnosis and appropriate management may prevent further complications.
ACD is characterized by the collection of mucinous material which accumulates in the adventitial layer of the vessels. The first case of this rare entity was reported in 1947, which involved the external iliac artery.(1) However, it affects predominantely the popliteal artery.(2) ACD may also involve other peripheral vessels, as the radial artery, but the percentage of reported cases in this location is limited to 2,5% of all ACD cases.(3)
To date, its etiology still has not been clarified. Several hypotheses have been proposed to explain its formation: cystic degeneration of the adventitia as a consequence of repetitive trauma(4,5); adventitial degeneration due to a systemic process; inclusion of mesenchymal cells within the adventitia(6,7,8); and development from a direct communication with an adjacent joint space(8).
ACD affects males predominantly, with a male to female ratio of 5 to 1, and patients are typically in their mid-40s. Some investigators have reported a slightly older age at diagnosis(9).
Pathology reveals that these cysts are filled with gelatinous mucoid material. A closer microscopic examination reveals a cuboid cell lining in the adventitial layer; atherosclerotic disease is absent.
The most common clinical presentation of ACD in the radial artery is as a newly detected asymptomatic pulsatile arterial mass. For this reason, the diagnosis of radial artery aneurysm/pseudoaneurysm should be excluded.
Apparently, the enlargement of the cyst is slow but progressive compression of the lumen can lead to arterial thrombosis with ischemic symptoms. In the radial artery, compression of nerve fibers has also been described, which may lead to presentation of paresthesias, pain, weakness or even thenar atrophy(10,11).
Diagnostic workup can involve angio-CT but current recommendations support DUS followed by MR or CT(12). DUS allows the evaluation of the cyst dimensions and the hemodynamic caractheristics of the vessel. Regarding diagnosis, these cysts should be differenciated from lipomas, fibromas or aneurysms. During follow-up, DUS is considered the first-line imaging for surveillance.
Treatment options are variable: nonsurgical management, cyst aspiration (percutaneous or open), angioplasty or surgical treatment. Surgical options include cyst incision and decompression, cyst resection alone or with repair with a patch (venous or synthetic) or reconstruction with a graft (venous or synthetic). The most common surgical option has been cyst resection and reconstruction with a reversed segment saphenous vein autograft(12,13).
When cystic ligation of the joint connection is performed as part of treatment, cyst recurrence has not been identified. On the other hand, leaving the articular branch has been related to failure of the procedure, leading to cyst reaccumulation. Recurrence or persistence rate of 9% has been reported, most of them occurred after less invasive techniques such as angioplasty or percutaneous aspiration(3).
In conclusion, although extremely uncommon, ACD of the radial artery should be suspected when a pulsatile mass is noted. An early diagnosis and appropriate management may prevent further complications.