Introduction
Chronic periaortitis is a rare disease that includes a set of idiopathic disorders characterized by inflammation and fibrosis in the retroperitoneal space around the aorta and iliac arteries(1). It includes idiopathic retroperitoneal fibrosis (the non-aneurysmatic form), inflammatory abdominal aortic aneurysm, in which there is no ureteral involvement, and perianurismatic retroperitoneal fibrosis, associated with fibrous tissue deposition around an abdominal aortic aneurysm, which may result in ureteric blockage(2). The pathophysiological mechanism is still not completely understood but there seems to be an immune-mediated inflammatory process(3).
Despite its idiopathic forms, chronic periaortitis and retroperitoneal fibrosis can be associated with autoimmune diseases, neoplasms, drugs, infections or radiotherapy(4,5). Little is known about the possible development of this complication after correction of abdominal aortic aneurysms (AAA) using endovascular aortic repair (EVAR) or after treatment of aortoiliac occlusive disease with percutaneous transluminal angioplasty (PTA) and stent or stent-graft implantation.
Methods
Search methods
A systematic search of original articles was carried out by the first two authors in the MEDLINE database, about the development of inflammatory periaortitis after EVAR or aortoiliac stet/stent-graft deployment. The search was conducted on 24th September 2020, using MEDLINE database through PubMed with the following query: ("aortitis"[MeSH Terms] OR "aortitis"[All Fields]) AND ("fibrosis"[MeSH Terms] OR "fibrosis"[All Fields]) AND endovascular[All Fields] AND ("aorta"[MeSH Terms] OR "aorta"[All Fields] OR "aortic"[All Fields]) AND ("stents"[MeSH Terms] OR "stents"[All Fields] OR "stent"[All Fields]).
Article inclusion
Only articles written in English were used. The first two authors evaluated all searched titles and abstracts selecting to full text-review those that report one or multiple cases of patients who developed chronic periaortitis after the implantation of aortic endoprostheses or aortoiliac stents in which a causal relationship can be inferred.
We also thoroughly review the bibliographic references of the selected articles and additional articles that met the inclusion criteria were included. We exclude articles in which patients were submitted to EVAR for treatment of inflammatory abdominal aortic aneurysms.
Data analysis
This systematic review was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA)(6). Patient characteristics, condition to treat, type of treatment, devices used, time to chronic periaortitis development, and the subsequent treatment are extracted from the articles reviewed.
Results
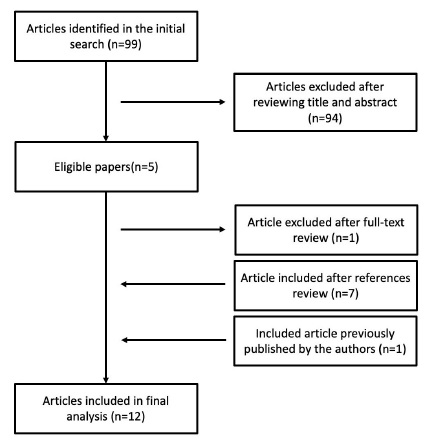
In our MEDLINE search, we identified 99 abstracts published. After a review of the title and abstract, 94 references were excluded. All articles found were single case reports. Of the 5 studies selected based on title and abstract 1 article was excluded because it reported a case in which chronic periaortitis was present before treatment by EVAR. After an exhaustive review of the references of the selected articles, 7 more articles were included. Bearing in mind that we recently published our experience of two patients who developed retroperiotoneal fibrosis after implantation of aortoiliac stents, we decided to include this paper in our review.
Chronic Periaortitis after EVAR
According to our systematic review, we identified 7 articles published about the development of chronic periaortitis after EVAR corresponding to simple clinical cases (Table 1).
Table 1 Characteristics of patients who developed chronic periaortitis after endovascular treatment of abdominal aortic aneurysm with endoprosthesis

AAA - abdominal aortic aneurysm; CIAA - common iliac artery aneurysm
All cases referred to infrarenal abdominal aortic aneurysms, with atherosclerotic etiology. All the patients were men with ages ranged from 59 to 78 years. All patients were treated with EVAR using a bifurcated stent-graft and in one patient an additional bell-bottom technique was used to treat a right common iliac artery aneurysm.
From the preoperative imaging study with Computed Tomography (CT) angiography, none of the cases presented any evidence of inflammatory aortic wall thickening. Routine preoperative inflammatory parameters measurement (c-reactive protein and erythrocyte sedimentation rate) was performed in all patients, whose results were in the normal range.
The type of stent-graft used was wide-ranging. In five patients endoprostheses composed of woven polyester were used and in two other patients, the endoprostheses used had an expanded polytetrafluoroethylene (ePTFE) covering. Regarding the material of the stents, in most cases, the composition was nitinol. OIne of the endoprosthesis is composed of stainless-steel stents (Zenith® endoprosthesis). Cases of stent-grafts with supra and infrarenal fixation were published.
The time to develop chronic periaortitis was as short as 8 days (immediate postoperative period), lasting up to 17 months after the procedure. Clinical manifestations included mainly abdominal or lumbar pain. In four of the documented cases, there was urethral involvement with hydronephrosis. Two of these required a decompression procedure (urethral stent) and in one patient the outcome was nephrectomy. In all patients, medical treatment was initiated and included the use of corticotherapy, tamoxifen or a combination of the two. The duration of treatment varies from 5 months to more than one year.
Chronic Periaortitis after stent / stent-graft implantation for treatment of occlusive arterial disease
According to our research, we only identified two cases of periaortitis that developed after the implantation of stents / stent-grafts in the aortoiliac sector. We also add two cases recently published by our group(18). All cases concern patients with intermittent claudication resulting from aortoiliac occlusive arterial disease. Two patients were men and two were women aged between 45 and 67 years. Two patients underwent kissing stenting of the aortic bifurcation and two single stenting of the left common iliac artery. Different devices were used, from nitinol stents to stent-grafts (ePTFE and woven polyester covering). The time to presentation since the procedure ranged from 2 months to 3 years. In only one of the cases, obstructive hydronephrosis was observed, requiring urethral stent placement. Medical treatment consisted of corticotherapy in three of the cases. The other patient did not initiate medical treatment, presenting a benign clinical evolution.
Discussion
De novo periaoritis is an extremely rare complication after EVAR or stents/stent-grafts implantation for occlusive aortoiliac arterial disease, with only a few cases described in the literature.
An inflammatory abdominal aortic aneurysm is part of chronic periaortitis spectrum and it is estimated that corresponds to about 5% of all abdominal aortic aneurysms (19). In this type of abdominal aortic aneurysm, the inflammatory process usually regresses after either endovascular or surgical treatment(20,21), although the regression seems to be more frequent after open surgery when compared to EVAR(22). What we present here is the opposite, the development of de novo periaortitis and retroperitoneal fibrosis after EVAR for non-inflamatory AAA treatment or stent/stent-graft deployment in the aortoiliac sector in patients without evidence of periaortic or systemic inflammation in the preoperative study.
Because the symptoms are nonspecific this may be an underreported entity. In the case of post-EVAR periaortitis, one explanation is that in many cases the elevation of inflammatory markers can be attributed to post-implantation syndrome. It has been hypothesized that periaortitis after EVAR could be a more severe form of this complication.
All the cases following EVAR correspond to male patients aged between 59 and 78 years. In the case of aortoiliac stenting for occlusive arterial disease, the age range was lower (45-67 years). In this group, two of the four patients were females. This male predominance is similar to that observed for idiopathic retroperitoneal fibrosis, with a male to female ratio reported of 2-3: 1 and a peak incidence between 40 and 60 years old(23). However, this can also be explained because AAA are more frequent in men and these are more often submitted to EVAR.
In the case of periaortitis after EVAR, it appears that this complication can occur with different types of endoprosthesis. In five cases the graft material consists of woven polyester: Talent®, AneuRx®, Endurant® and Endurant II® from Medtronic" (Medtronic AVE, Santa Rosa, CA, USA) and the Zenith® endoprosthesis (William Cook, Brisbane Australia). In 2 cases, the endoprosthesis used was an ePTFE graft: Gore excluder® (W. L. Gore and Associates, Flagstaff, Ariz). Most of these stent-grafts are made up of nitinol stents, however, it was also found that this complication developed with an endoprosthesis made of stainless-steel stents - Zenith® device (William Cook, Brisbane Australia). In the same way, in the treatment of occlusive disease, the development of periaortitis was also observed with different devices.
Table 2 Characteristics of patients who developed chronic periaortitis after endovascular treatment of intermittent claudication due to aortoiliac occlusive disease
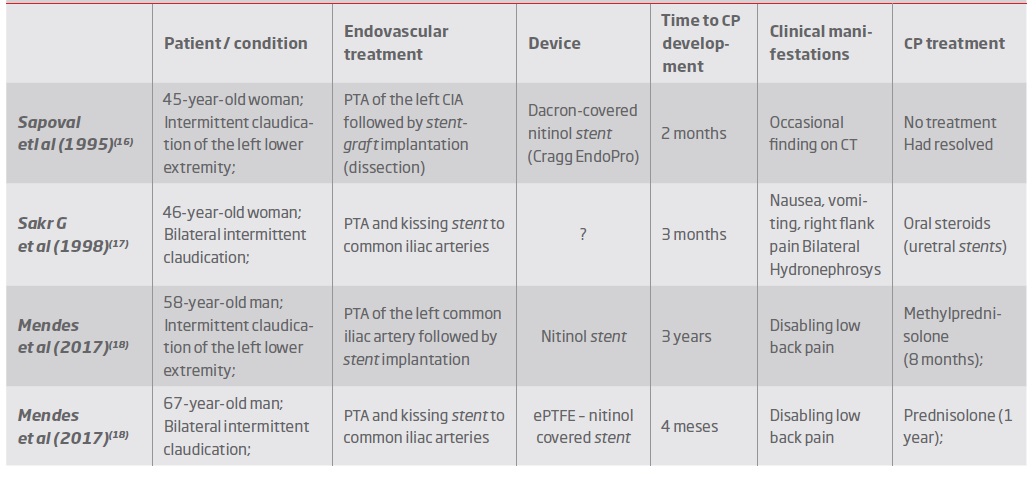
PTA - percutaneous transluminal angioplasty; CIA - common iliac artery.
In the case of the development of periaortitis after EVAR, it is interesting to note that the two cases with the earliest clinical presentation (8 days and 2 months) were patients treated with Gore excluder® endoprostheses.
The exact mechanism of these patients’ secondary periaortitis, to our knowledge, remains unknown. Some studies have shown that chronic periaortitis could be the result of an abnormal reaction to antigens contained in atherosclerotic plaques in the abdominal aorta. It could thus be hypothesized that stent/stent-graft deployment by interfering with the integrity of the arterial wall, could expose these antigens and trigger the inflammatory response(24).
In most cases this complication developed between several months to years after the implantation of the endoprosthesis, and in only one of the cases it manifested in the immediate postoperative period with lumbar pain and lower limb swelling(14). Most patients had low back or abdominal pain associated with constitutional symptoms (low fever, anorexia and fatigue).
Concerning the treatment of idiopathic cases of retroperitoneal fibrosis, the first goal is to reverse ureteral obstruction, when present, and protect kidney function. Medical therapy should be started as soon as possible to reverse the inflammatory phase, leading to the resolution of symptoms and the normalization of acute phase reagents(2).
Patients were treated with steroids and tamoxifen. The rationale for the use of tamoxifen was the fact that its effectiveness has been demonstrated in cases of idiopathic retroperitoneal fibrosis(25). However, a recent randomized clinical trial showed that prednisolone is more effective than tamoxifen in preventing recurrences of idiopathic retroperitoneal fibrosis.(26), reason that may explain the fact that in the most recent published articles only corticosteroids were used. It is interesting to note that the use of corticotherapy, tamoxifen or a combination of the two allowed the complete resolution in all cases.
Before starting treatment, it is essential to exclude an infectious process from the endoprosthesis. Adequate image and laboratory investigations are essential. Patients should collect blood cultures to rule out infection. CT signs suggestive of infection include the presence of peri-prosthetic air, collections in the aneurysmal sac and ectopic gas(27). The use of white blood cell scintigraphy could also be important since, unlike in the case of infection, there is no uptake in inflammatory periaortitis(15).
Four patients presented with acute kidney injury resulting from hydronephrosis due to urethral obstruction requiring urinary diversion or ureteral stenting. One patient even needed to perform a nephrectomy. Similarly, in cases of idiopathic periaortitis, urethral involvement is the most frequent complication(1).
Conclusion
The development of periaortitis and retroperitoneal fibrosis is an extremely rare complication of EVAR or aortoiliac stent / stent-graft implantation. This complication can occur with different types of endoprosthesis and stents. The demography appears to be similar to that described for idiopathic retroperitoneal fibrosis. The delay from the procedure to the onset of inflammation is highly variable. Early treatment appears to be essential to avoid long-term renal impairment. Therapeutic regimens with corticotherapy and tamoxifen, similar to those used in idiopathic retroperitoneal fibrosis, appear to be effective. It is important to exclude infection before starting treatment.