Introduction
False aneurysms of the Renal Artery (FRAs) usually originates from renal trauma or iatrogenic causes, such as vascular procedures (angioplasty and renal stenting), urological catheterizations or percutaneous renal procedures (biopsies, nephrostomies, nephroureterolithotomies and partial nephrectomy).(1-6)
The diagnosis of FRA can be incidental or due to hematuria, low back pain, abdominal pain, dizziness, syncope, hypotension or hypovolemic shock. The worsening of renal function is rare and is more frequent when there's a single kidney. The possible causes are the presence of blood clots in the excretory system (acute post-renal kidney injury) or the combination of hypotension and hypovolemia (acute pre-renal kidney injury).(7)
Due to the nature of the FRA wall, they have a high risk of rupture and should therefore be diagnosed and treated soon.(8)
The therapeutic options in the FRA are varied and related to the size of the FRA and clinical manifestations, ranging from the injection of echo-guided thrombin to treatment by endovascular or open surgery. Open surgery usually consists in nephrectomy because in most cases the vessels that are involved are small intra-parenchymal vessels and so the endovascular treatment is the only that can minimize the loss of kidney tissue. Recent developments in endovascular surgery have made embolization by superselective catheterization of the artery involved the treatment of choice. The rate of endovascular complications is low, with the rate of occlusion of the main renal arteria and consequent renal infarction being minimal.(9-11)
Objectives
To evaluate the experience of the CHUP’s angiology and vascular surgery department in the approach of renal artery pseudoaneurysms.
Methods and material
A retrospective review was undertaken using the clinical and imagiological records of 20 patients diagnosed with renal artery pseudoaneurysm from 2010 to 2018. SPSS version 21 was used for the treatment and analysis of the descriptive statistics (univariate and bivariate) , hypothesis tests and analysis of probability of accumulated survival.
Results
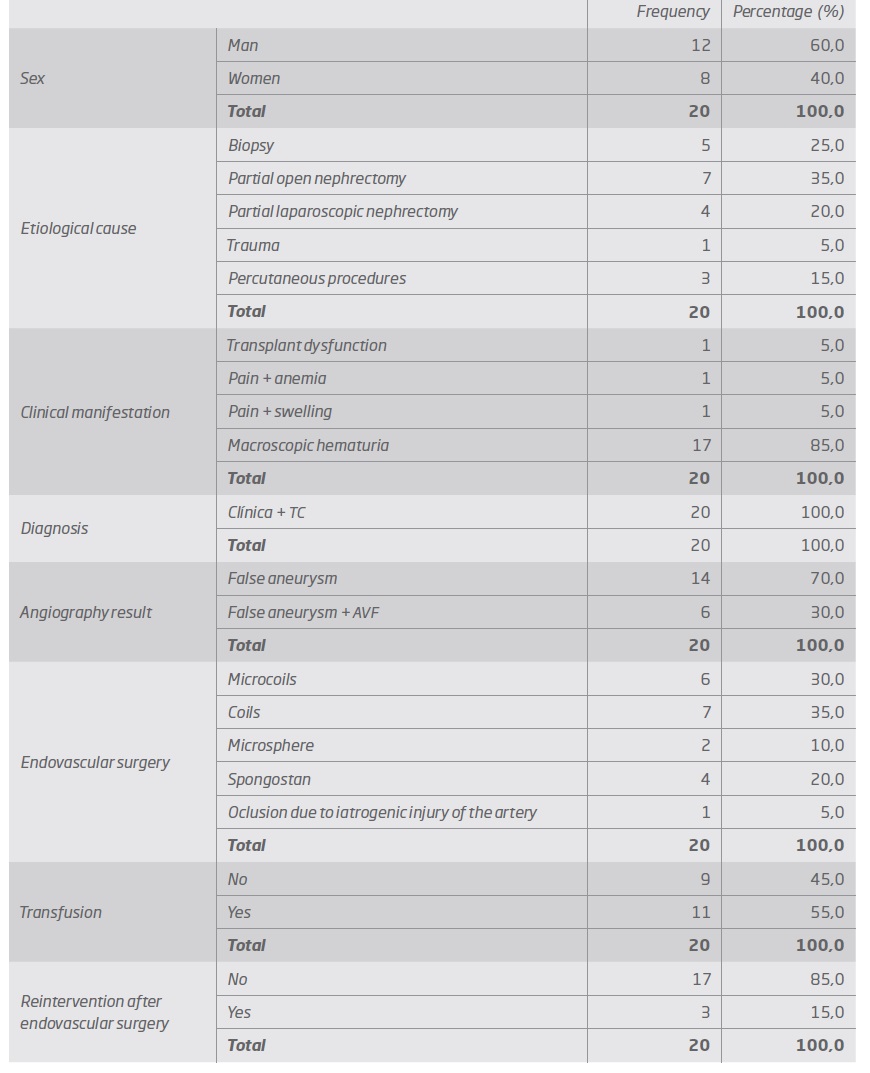
60% of the patients were men and the average age was 55.7 + -19.2 years, with at least 6 to 86 years old.
The etiological cause of FRA in 95% of the cases was iatrogenic due to an urological / nephrological procedure (35% due to open partial nephrectomy (OPN), 25% due to biopsies, 20% due to laparoscopic partial nephrectomy (LPN), 15% due to percutaneous procedures) and one case due to trauma.
The diagnosis was based on clinical suspicion (85% had macroscopic hematuria) and all the cases were confirmed with CT. In 30% of the cases, an association with AVF was observed.
The therapy performed in all cases consisted of embolization of the FRA feeding artery, with embolization with coils being the most used method (65% in total - 30% microcoils + 35% coils) (Table I)
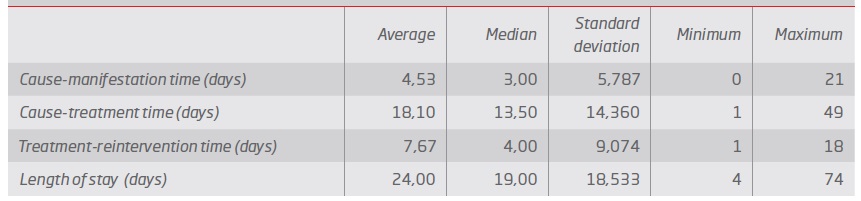
The time between the lesion and the clinical manifestation was 4.5 days, the time between the lesion and the treatment was 18.1 days. (Table II)
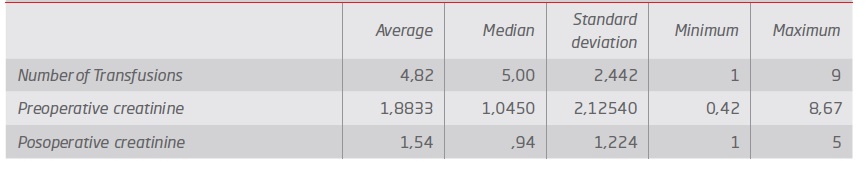
The transfusion rate was 55% with an average of 4.8 units of red blood cells and an average of length of stay of 24 days.
There was no statistically significant difference between pre and postoperative creatinine. (Table II and III).
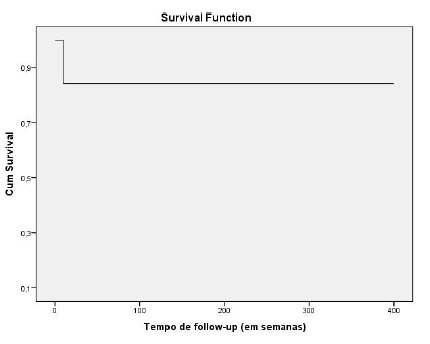
Mortality was 0%, the rebleeding rate (which occurred in the first two weeks) requiring a second embolization was 15% and the kidney salvage rate was 95% with an average follow-up time of 96 weeks. (Chart 1)
Discussion/ Conclusion
In our series, the average age at diagnosis was 55.7 years with a predominance of males (60%). Guo et al(12) reported an average age of 46.6 years and a male involvement of 63%.
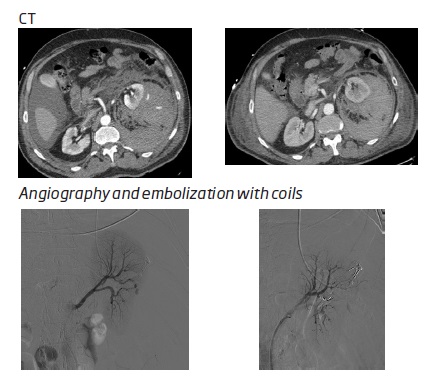
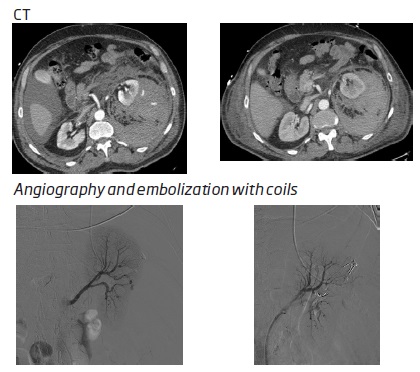
Partial nephrectomy (PN) was the most common etiological cause, 35% for OPN (open partial nephrectomy) and 20% for LPN (laparoscopic partial nephrectomy) (Figures 1 e 2). In the study by Guo et al(12), LPN represented 25.9% of the etiological causes. Zhu Y et al(13) published an incidence of FRA after LPN (4.26%) higher than after OPN ( 3.17%). In fact, in our study, we cannot calculate this rate but we believe that the reason why the percentage of FRA after OPN is higher is because the study is made with records between 2010-2018 and therefore the absolute total number of OPN done in this period is also much higher than absolute total number of LPN done in the same period. Renal biopsies were the etiological cause in 25% of our cases (Figure 3). In the study by Guo et al(12) renal biopsies represent 51.9% of the etiological causes, a value much higher than that of our series.
Percutaneous urological procedures (in our case, percutaneous nephrolithotomy-NLP) represented 15% of the etiological causes. In the study by Guo et al(12) this was the cause in 14.8% of FAR. Poyraz N et al(16) described 14 cases of FAR and 5 of AVF in 1609 patients undergoing NLP, with all patients presenting macroscopic hematuria or massive hematuria and all requiring blood transfusion. Coil embolization was the preferred treatment, with only two patients developing recurrence of hemorrhage and treated for further embolization.
In only one case (5%), the etiology was blunt kidney trauma (Figure 4). According to Ierardi AM et al(17) kidney injuries occur in approximately 1-5% of all trauma patients.
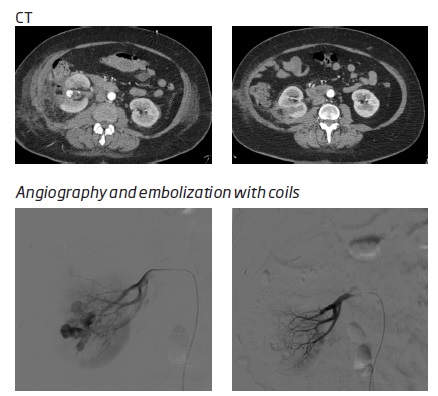
Figure 1 False right renal aneurysm, after conventional partial nephrectomy treated by embolization with coils
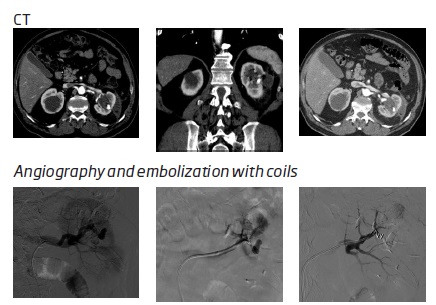
Figure 2 False left renal aneurysm with associated VAF, after laparoscopic segmental nephrectomy treated with embolization with coil
Endovascular surgery is currently the first therapeutic line that can prevent nephrectomy by up to 78%-83%,(18) although traditionally high-grade kidney injuries are corrected by conventional surgery.
The most common clinical manifestation of FAR was macroscopic hematuria that occurred in 85% of patients. According to the literature, 11.2 to 17.5%(19) of hemorrhages endanger the patient's life. The diagnosis of FAR in all cases was based on clinical suspicion and was confirmed by CT. According to Guo et al(12), the first exam to be performed in the clinical suspicion of FAR should be ultrasound, to avoid the contrast overload associated with CT. However, we believe that the CT it will always be necessary because it allows for diagnosis and surgical planning and is independent of the patient's biotype and of the technician who performs it.
Pitton M B et al(2) reported a rupture rate of 76.3% in FAR compared to 3.1% in true aneurysms, and there do not seem to be any predictive factors for rupture. Therefore, the literature argues that FRAs should be treated after being diagnosed, which is in line with our series in which all FARs were treated surgically.
In our series, the therapy performed consisted of embolization of the FAR feeding artery in all cases, with embolization with coils being the most used method. Mortality was 0%, the bleeding recurrence rate requiring a second embolization was 15% and the kidney salvage rate was 95%. There was no statistically significant association between the etiology of FAR and the number of transfusions and therapeutic reintervention. Ghoneim et al(22) reported that the success rate was 90 to 95% success(23,24) and that selective renal embolization does not cause obvious changes in the glomerular filtration rate, which is in accordance with our results (mean preoperative creatinine 1.9 and 1.5 with no no statistically significant difference).
The time between the injury and the clinical manifestation was 4.5 days, the time between the injury and the treatment was 18.1 days. The transfusion rate was 55% and the average length of stay was 24 days. Hongjie G et al reported lower values for the time between injury and treatment (3 days), with 88.9% of patients treated in the first 14 days. These long times and the need to carry out a large number of transfusions, make us suppose that a better knowledge of this pathology can improve these results. The urologist must be familiar with this clinical entity to make a quick diagnosis and promote an efficient treatment.