Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.16 no.3 Lisboa set. 2020
CLINICAL CASE
Iatrogenic injury of the subclavian artery treated percutaneously with arterial closure device
Lesão iatrogénica da artéria subclávia tratada percutaneamente com dispositivo de encerramento arterial
Inês Antunes1, Carlos Pereira1, Gabriela Teixeira1, Carlos Veiga1, Daniel Mendes1, Carlos Veterano1, Henrique Rocha1, João Castro1, Rui Almeida1
1 Serviço de Angiologia e Cirurgia Vascular, Centro Hospitalar do Porto, Porto, Portugal
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Subclavian arterial puncture is a relatively frequent complication of attempted placement of central venous catheters (CVC). The placement of a CVC in the artery is rarer, but with potential serious complications especially in its withdrawal. Anticipating these complications, control of potential bleeding in catheter withdrawal is usually performed by surgical or endovascular approach with endoprosthesis release. Our goal is to present the treatment with a percutaneous arterial closure device.
Materials / Methods: Presentation of a clinical case of a CVC placed in the subclavian artery treated with a percutaneous arterial closure device.
Results: A 51-year-old man hospitalized for acute myocardial infarction. On the first day of hospitalization, the introduction of a CVC into the right subclavian vein was attempted. In view of the suspected intraarterial position, CT angiography scan demonstrated that the CVC had been introduced into the subclavian artery with a point of entry proximal to the passage under the clavicle and with a path to the brachiocephalic trunk. Hypocoagulation with UFH was initiated given the risk of pericateter thrombosis and embolization. The use of percutaneous closure device ProGlide® was planned using the CVC pathway. As predictable difficulties for this option was the long CVC path to the arterial entry point, raising questions about the extent of the suture mechanism of the device and the progression of nodes in this path. Under fluoroscopic control, an angioplasty balloon was progressed until the CVC point of entrance for temporary bleeding control in case of ProGlide® failure; in which case the procedure would be completed with a covered endoprosthesis; the subclavian artery had a diameter of 12 mm and was ipsilateral to a brachiocephalic fistula. It was decided to retrograde puncture the fistula and progress the balloon to the subclavian artery. The rigid guide wire was then placed through the CVC and the CVC removed. Two Proglide® closure devices (positioned at 10 p.m. and 2 p.m.) were released. The complete resolution of clinical and imaging hemorrhage was verified.
Discussion/Conclusions: Placement of CVC in the subclavian artery is a potentially serious complication since its removal can be complicated with severe haemorrhage. Depending on the point of entry, there may be additional complexities due to the proximity of the vertebral and carotid arteries. In this case we left open several hypotheses (endovascular and ultimately surgical), but our preference was ad initium the percutaneous introduction of closure device given the feasibility, simplicity, less aggressiveness, non-interference with the vertebral ostium, and lower cost compared to a covered endoprosthesis.
Keywords: Central venous catheter; iatrogenic lesion; subclavian artery injury; percutaneous arterial suspension device
RESUMO
Introdução: A punção arterial subclávia é uma complicação relativamente frequente da tentativa de colocação de cateteres venosos centrais (CVC). A colocação de um CVC na artéria é mais rara, mas com potenciais complicações graves sobretudo na sua retirada. O controle da potencial hemorragia na retirada do CVC é habitualmente realizado por abordagem cirúrgica ou por via endovascular com libertação de endoprótese. O nosso objetivo é apresentar o tratamento com recurso a dispositivo de encerramento arterial percutâneo.
Materiais/Métodos: Apresentação de um caso clínico de um CVC colocado na artéria subclávia tratado com dispositivo de encerramento arterial percutâneo.
Resultados: Homem de 51 anos internado por enfarte agudo do miocárdio. No primeiro dia de internamento foi tentada a introdução de um CVC na veia subclávia direita. Perante a suspeita de posição intra-arterial foi realizada angio TAC que demonstrou que o CVC havia sido introduzido na artéria subclávia com ponto de entrada proximal à passagem sob a clavícula e com trajeto até ao tronco braquiocefálico. Foi iniciada hipocoagulação com HNF dado o risco de trombose pericateter e embolização. Foi planeada a utilização de dispositivo de encerramento arterial percutâneo Perclose ProGlide® utilizando o trajeto do CVC. Como dificuldades previsíveis para essa opção estava o longo trajeto do CVC até ao ponto de entrada arterial, levantando questões de alcance do mecanismo de sutura do dispositivo e da progressão dos nós nesse trajeto. Sob controlo fluoroscópico foi colocado retrogradamente um balão intra-arterial para controle temporário de hemorragia em caso de insucesso com o ProGlide®; nesse caso o procedimento seria completado com endoprótese recoberta. A artéria subclávia tinha um diâmetro de 12mm, e era ipsilateral a uma FAV úmero cefálica pelo que se optou por puncionar retrogradamente a FAV e progredir o balão para a artéria subclávia. Foi então colocado fio guia rígido pelo CVC, este foi retirado e libertaram-se dois dispositivos de encerramento Proglide® (posicionados às 22h e 14h). Constatou-se a resolução completa da hemorragia clinica e imagiologicamente.
Discussão/Conclusões: A colocação de CVC na artéria subclávia é uma complicação potencialmente grave uma vez que a sua remoção pode ser complicada com hemorragia de difícil resolução. Dependendo do ponto de entrada, podem ainda haver complexidades adicionais pela proximidade das artérias vertebral e carótida. Neste caso deixamos em aberto várias hipóteses de recurso (endovascular e em último caso cirúrgico) mas a nossa preferência foi ad initium a introdução percutânea de dispositivo de encerramento dadas a exequibilidade, simplicidade, menor agressividade, não interferência com o óstio da vertebral, e também menor custo comparado com uma endoprótese recoberta.
Palavras-chave: Cateter Venoso Central; lesão iatrogénica; lesão da artéria subclávia; dispositivo encerramento arterial percutâneo
Introduction
Improvements in life expectancy and intensive care have leaded to an increase in the number of patients receiving central venous catheters (CVC)(1). CVC may be inserted in the internal jugular, subclavian or femoral veins.
CVC placement is a risky procedure. Most of the complications are mechanical associated with the puncture of contiguous structures (pleura, nerves, arteries, esophagus). Inadvertent arterial puncture with a low-gauge needle is usually benign and occurs in about 5% of the cases(2).
The subclavian veins are considered safer for long-term catheter use. But the insertion of the CVC at this location is technically more challenging. There are lots of possible complications during the insertion of a subclavian vein CVC such as pneumothorax, hemothorax, nerve injury and hematoma. An unusual but potentially very serious complication is the inadvertent deployment of the CVC in the subclavian artery. Iatrogenic trauma to the subclavian artery can cause severe bleeding, false aneurysm, arteriovenous fistula, arterial dissection, embolism, or thrombosis. These arterial traumatisms can be approached conservatively with CVC removal and external compression (which is very difficult in the setting of the subclavian artery because of the inability of perform a proper compression, which may be complicated by difficult to control and even life-threatening bleeding) or through endovascular or surgical interventions.
In the present paper we report a clinical case of use of the Perclose Proglide® closure device (Abbott Vascular, Santa Clara, CA, USA) to remove a CVC inserted in the right subclavian artery.
Clinical Case
A 51-year-old man hospitalized because acute myocardial infarction. On the first day of hospitalization, the deployment of a CVC into the right subclavian vein was attempted.
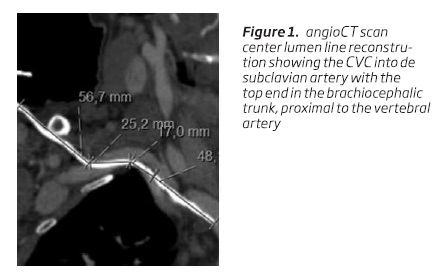
Due to the suspicion of intra-arterial position, a computed tomography (CT) scan was performed and showed that the CVC had been introduced into the subclavian artery with a point of entry proximal to the passage under the clavicle and with the extremity of the CVC in the brachiocephalic trunk proximal to the vertebral artery. Given the risk of peri-catheter thrombosis and consequent embolization, particularly to the vertebral artery, hypocoagulation with unfractionated heparin was initiated and we decided to externalize da CVC so that its end became distal to the vertebral artery after measurements of the angio-CT reconstruction.
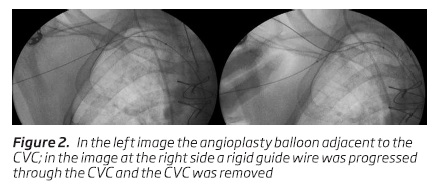
The use of percutaneous Perclose ProGlide® arterial closure device was planned. However, we were afraid of not obtaining an adequate bleeding control, so we planned to place an angioplasty balloon at the level of the CVC entry hole, which would be inflated for temporary bleeding control in the event of Proglide's failure; in which case the procedure would be completed with a covered endoprosthesis.
The procedure was performed in the operating room. The patient had an homolateral brachiocephalic fistula, so it was decided to use this vascular access to place the angioplasty balloon in proper position. Under local anesthesia, a retrograde puncture of the arteriovenous fistula was performed, the guide wire was progressed through the arteriovenous anastomoses to the brachial artery, and then to the subclavian artery. Then the angioplasty balloon (of 12mm diameter) was progressed to the subclavian artery until it was adjacent to the CVC point of entrance in the artery (Figure 2, left image). Then a rigid guide wire was placed through the CVC and the CVC removed (Figure 2, right image).
Two Proglide® closure devices (positioned at 10 p.m. and 2 p.m.) were released. The complete resolution of clinical and imaging hemorrhage was verified with the final control angiography.
Discussion/Conclusions
An increasing number of Central Venous Catheters are placed in the current practice particularly in intensively cared patients. The exponential uptake of means for intravascular access has also increased the risk of related complications(3). In fact, considering the CVC deployment guided by the surface anatomical structures (landmark method), complication and failure rates amount to 19%(4) and these complications can range from minor to life-threatening. Ultrasound guided CVC placement should be privileged, as it allows a safer procedure.
Inadvertent puncture and deployment of the CVC into an artery is an uncommon but difficult to manage complication. Arterial puncture with a small needle during the placement of a CVC ranges from 4.2% to 9.3% and this puncture appears to be harmless(3). However, when arterial puncture is not recognized it can result in the subsequent placement of a large catheter into the artery. In reported series the rate of CVC inadvertently placed in arteries range from 0.1 to 1%.
When a CVC is placed in an artery potentially disastrous complications may occur. One of these is drug infusion. If a drug with potential for limb injury are administrated, it can lead to limb ischemia and even limb loss. In the subclavian position one of the most feared complication is the potential of embolization due to peri catheter thrombosis which can lead to distal embolization and consequently upper limb ischemia or, even more serious, central embolization (to the carotid or vertebral arteries) which can lead to stroke.
Other potentially disastrous complication, that can be life-threatening, is the possibility of difficult to control bleeding in the removal of the CVC. For example, if the perforation of the artery communicates with the pleural space it can lead to hemothorax and as the lung is completely compressible, the pleural space can accommodate near to 3 Liters of blood. It is important to know exactly where the point of entrance of the CVC in the artery is to define a treatment plan and only after a proper image study, such as CT scan, can the catheter be removed. On the other hand, the catheter should be removed as soon as possible because prolonged arterial cannulation can result in thrombus formation and embolization which can result in stroke in the case of subclavian or carotid arteries. For this reason, while planning the procedure, hypocoagulation with unfractionated heparin should be initiated to prevent thromboembolic complications related to peri-catheter thrombosis.
After placement of a CVC in an artery there are three possible options: remove the CVC and apply pressure (“pull-and-pressure” strategy), surgical repair or endovascular repair. In the case of a CVC in the femoral artery, to remove the CVC and apply pressure is a reasonable approach. This “pull-and-pressure” approach is not so safe and effective in the case of carotid or subclavian arteries due to the inability to effectively compress these vessels. Shah et al(5) studied the difference between “pull-and-pressure” and open surgical technique for cannulation of the carotid or subclavian arteries and from a total of 11 patients, 9 were submitted to surgical repair with no complications, in the other 2 patients the sheath was pulled and pressure was applied and 1 of this patients suffered a stroke and the other a pseudoaneurysm. The authors also reviewed 4 previous studies(6-9) and from a total of 11 870 attempted cannulation of the internal jugular artery, there were 20 (0.17%) intra-arterial cannulations. The “pull-and-pressure” technique was applied in 19 cases (2 of them died and 6 suffered complications). From their experience and literature review Shah et al recommended surgical treatment as treatment of choice in these cases. In 2008 Guilbert et al(10) found that mortality and morbidity were unacceptably high in the “pull-and-pressure” technique while surgical and endovascular procedures have better results. From their serie of 13 patients, 5 were submitted to “pull-and-pressure” technique and all of them had major complications including 1 death; the remaining 8 patients submitted to endovascular/surgical techniques had no major complications. Guilbert et al proposed a management algorithm: the catheter should be left in place and if the site is easily accessible surgically a direct exploration, catheter removal and artery repair should be performed. If the site is not easily accessible endovascular repair should be done. Since then different endovascular devices have emerged and the use of closure devices have been reported.
Surgical repair is always an option but may be associated with other complications. The surgical risk of patients must be weighed carefully since they are mostly patients with multiple comorbidities, admitted in intensive care unit or with long-term hospitalization.
Nowadays several percutaneous options are possible for these cases such as stent graft deployment, embolization, and percutaneous closure devices(11). Endovascular techniques, particularly stent grafting, have been used but in the case of subclavian artery sometimes it may be challenging because of the origin of the vertebral artery or, in the case of brachiocephalic trunk, the origin of the right carotid artery. Vascular closure devices have emerged as an improvement in the management of procedures requiring arterial access(12). With the widespread use of these devices, their indications were being extended. One possible applicability of the vascular closure device is to achieve hemostasis in arterial accesses placed in sites which may be difficult to achieve surgically(13,14). The use of vascular closure devices to safely remove a CVC deployed in an artery has been reported, with good results, suggesting that it is a safe and effective treatment option(15,16).
In the presented case we considered the three options: surgical (through a cervical approach), endovascular (placement of a stent graft) and the use of a percutaneous closure device. The surgical approach was our last option because it is a more aggressive procedure. The endovascular deployment of a stent graft in the subclavian artery was possible and, in this case, there is a good landing zone to deploy the graft without risk of occlusion of the vertebral osteo. But we thought that due to the feasibility, simplicity, less aggressiveness, non-interference with the vertebral ostium, and lower cost compared to a covered endoprosthesis, the use of a percutaneous closure device was the best alternative. As predictable difficulties for this option was the long CVC path to the arterial entry point, raising questions about the extent of suture mechanism of the device and the progression of nodes in that path. We did not face any of these difficulties, the procedure was uneventful and success. In our opinion, the use of percutaneous access closure devices should be considered in these cases.
Important to note is that despite all treatment options, the ideal is to avoid arterial injury. The most used method to avoid arterial placement is based in the color and pulsatility of the blood in the needle however this method is unreliable, especially in critical patients. An alternative may be the measure of blood gases. Ultrasound guided placement has been described as a more reliable alternative, but it is important to note that arterial cannulation can occur even with the use of ultrasound guidance.
Conclusions
Inadvertent cannulation of an artery is the most common mechanical complication of CVC placement. In this case, the catheter should be left in place until a strategy is defined, which usually implies an accurate evaluation of the CVC and its point of entrance in the artery, normally obtained with a CT scan. Surgical/endovascular repair is safer than “pull-and-push” strategy. Depending on the presence or absence of the catheter still in place different options are available ranging from percutaneous devices, endovascular techniques (particularly stent grafting) and surgical repair.
REFERENCES
1. Giordano, A. Use of the Perclose Proglide Closure Device to remove a Central Venous Catheter Inadvertently Inserted in the Right Subclavian Artery. Open J Clin Med Case Reports. 2015(1):1-6. [ Links ]
2. Golden LR. Incidence and management of large-bore introducer sheath puncture of the carotid artery. J Cardiothorac Vasc Anesth 1995;9: 425-8 [ Links ]
3. A, Bowdle. Vascular Complications of Central Venous Catheter Placement: Evidence-Based Methods for Preention and Treatment. Journal of cardiothoracic and Vascular Anesthesia. 2014(28):358-368. [ Links ]
4. Seleznova Y, Brass P, Hellmich M, Stock S, Müller D. Cost-effectiveness-analysis of ultrasound guidance for central venous catheterization compared with landmark method: a decision-analytic model. BMC Anesthesiology. 2019:19-51. [ Links ]
5. Shah PM, Babu SC, Goyal A, Mateo RB, Madden RE. Arterial misplacement of large-caliber cannulas during jugular vein catheterization: Case for surgical management. J Am Coll Surg. 2004:198-939. [ Links ]
6. Kron, I. J. Arch vessel injury during pulmonary artery catheter placement. Ann Thorac Surg. 1985(39):223-224. [ Links ]
7. Golden, L. Incidence and management of large-bore introducer sheath puncture of the carotid artery. J Cardiothorac Vasc Anesth. 1995(9):425-428 [ Links ]
8. Shah, KB, Rao TL, Laughlin S, El-Etr AA. A review of pulmonary artery catheterization in 6,245 patients. Anesthesiology. 1984(61):271-275. [ Links ]
9. Schwartz, A. J. Carotid artery puncture with internal jugular cannulation. Anesthesiology. 1979(51) S160. [ Links ]
10. Guilbert MC, Elkouri S, Bracco D, Corriveau MM, Beaudoin N, Dubois MJ,et al.Arterial trauma during central venous catheter insertion: Case series, review and proposed algorithm. J Vasc Surg. 2008(48):918-925. [ Links ]
11. Kastler A, Chabanne R, Azarnoush K, Cosserant B, Camilleri L, Boyer L, et al. Arterial Injury Complicating Subclavian Central Venous Catheter Insertion. Journal of Cardiothoracic and Vascular Anesthesia. 2012(26):101-103. [ Links ]
12. Byrne RA, Cassese S, Linhardt M, Kastrati A. Vascular access and closure in coronary angiography and percutaneous intervention. Nat Rev Cardiol. 2013(10):27-40. [ Links ]
13. Kim TH, Shim WH.. Postclose technique for large sheath arterial access using perclose(TM) in emergency endovascular repair. Nat Rev Cardiol. 2013(83):1176-1179. [ Links ]
14. Schäfer U, Ho Y, Frerker C, Schewel D, Sanchez-Quintana D, Schofer J, et al. Diret percutaneous access technique for transaxillary transcatheter aortic valve implantation: "the Hamburg Sankt Georg approach". JACC Cardiovasc Interv. 2012(5):477-486. [ Links ]
15. Berlet MH, Steffen D, Shaughness G, Hanner J. Closure using a surgical closure device of inadvertent subclavian aretry punctures during central venous catheter placement. Cardiovasc Intervent Radiol. 2001(24):122-124. [ Links ]
16. Meyhoefer J, Lehmann H, Minden HH, Butter C. Closure of the subclavian aretry puncture site with a percutaneous suture device after removal of an arterial pacemaker lead. Europace. 2006(8):1070-1072. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: ines.antunes89@gmail.com (I. Antunes).
Recebido a 03 de junho de 2019. Aceite a 23 de agosto de 2020.