Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Angiologia e Cirurgia Vascular
Print version ISSN 1646-706X
Angiol Cir Vasc vol.16 no.3 Lisboa Sept. 2020
EDITORIAL
Actividade de Angiologia e Cirurgia Vascular no período de confinamento devido à pandemia COVID-19 - Hospital da Senhora da Oliveira, Guimarães
Vascular Surgery Practice during the COVID-19 lockdown - Hospital da Senhora da Oliveira, Guimarães
Joana Ferreira1, Pedro Pinto Sousa1, Sandrina Braga1, João Correia Simões1, Celso Carrilho1, Amílcar Mesquita1
1 Serviço de Cirurgia Vascular e Centro Académico do Hospital da Senhora da Oliveira Guimarães; Portugal
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Ever since the first positive case was identified on March 2nd in Lousada, a region close to the border of our catchment area, we reacted immediately by systematically repurposing our surgical wards.
Objective: Describe the changed made by our Vascular Surgery Department from March 13 to May 14.
Methods: We collected clinical, operative, and consultation volume data from March 13 to May 14 and we compared it with the historical averages. We also reviewed the documents related to the planification activity.
Results: At the peak of the outbreak, we adopted a split-team policy and encouraged complete team segregation to reduce the risk of intradepartmental cross-contamination. Non-ambulatory surgical volume decreased by 54.8% (from 31 cases to 14 cases), and the ambulatory surgical activity was cancelled. Our in-person consultation volume decreased 86.4%; 73 consultations were completed by phone, in which the patient was never evaluated in-person. In the emergency room the main difference between the pre-pandemic to the pandemic was in the number of patients observed without vascular pathology (82 versus 28).
Conclusions: The adaptation to COVID-19 pandemic reduced significantly the surgical production of our Vascular Surgery Department.
Keywords: Coronavirus; COVID-19; SARS-CoV-2; Pandemic; Vascular Surgery Department
RESUMO
Introdução: Desde que o primeiro caso positivo de COVID-19 foi identificado a 2 de março em Lousada, uma região próxima à nossa área de influência, tivemos que readaptar a nossa actividade clínica.
Objetivo: Descrever as alterações realizadas pelo nosso Serviço de Cirurgia Vascular de 13 de março a 14 de maio.
Métodos: Recolhemos dados clínicos, da actividade cirúrgica, de internamento e da consulta, de 13 de março a 14 de maio e comparamos com o mesmo período do ano anterior. Também fizemos uma revisão dos documentos relacionados com a planificação da nossa actividade.
Resultados: No pico do surto, dividimos a equipa de trabalho e incentivamos a segregação dos elementos para reduzir o risco de contaminação cruzada. O volume cirúrgico diminuiu 54,8% (de 31 casos para 14 casos) e a atividade cirúrgica de ambulatório foi cancelada. O volume de consultas presenciais diminuiu 86,4%: foram realizadas 73 consultas por telefone. No serviço de urgência, a principal diferença entre o perído pré-pandémico e a pandemia foi no número de doentes observados sem patologia vascular (82 versus 28).
Conclusões: A adaptação à pandemia COVID reduziu significativamente a produção cirúrgica do nosso Departamento de Cirurgia Vascular.
Palavras-chave: Coronavirus, COVID-19; SARS-CoV-2; Pandemia; Departamento de Cirurgia Vascular
Introduction
The Hospital Senhora da Oliveira has a large catchment area from the following regions: Guimarães, Vizela, Fafe, Cabeceiras de Basto e Mondim de Basto, providing healthcare for 240.000 inhabitants.
The first case of COVID-19 declared in Portugal was on March 2nd in Lousada, a region close to the border of our catchment area (figure 1).
On the March 16 we received the first COVID-19 patient in our hospital.
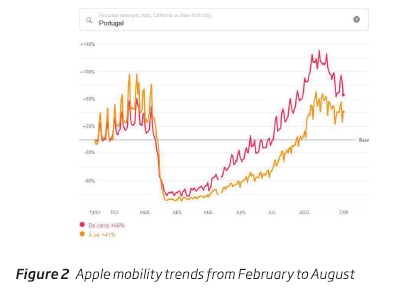
We analyzed our surgical practice from March 13 to May 14 (2 months). The Portuguese Government declared a lockdown on March 16, but, the general population had already curtailed their movements, opting to stay at home from March 6. This is confirmed by Apple Mobility Trends report available online (figure 2):
Mirroring this, before the lockdown had been officially declared, our department decided to postpone elective surgeries and non-essential medical procedures from March 11. All the Vascular Surgeons decided on their own to start using personal protective equipment and stockpiling it.
Overall activity
Our department has six vascular surgeons. At the peak of the outbreak, we adopted a split-team policy and encouraged complete team segregation to reduce the risk of intradepartmental cross-contamination. We were split in three groups. Each team was composed by two senior vascular surgeons. They were responsible for 24 hours shifts. The teams worked on alternate days. The two elements from each team tried to minimize direct contact with each other.
During a 24-hour work period we guaranteed essential surgeries and the care of emergency department patients. We also saw in-patients from other departments and selected outpatients.
Surgical activity
We decided to defer all elective operations to the greatest extent possible according to the international recommendations.(1)
All priority surgical activity at the hospital was performed in the two rooms of the Cardiovascular Intervention Unit. The rooms in the operating theater were converted to a COVID-19 ICU. 50% of the beds were used with that objective. In fact, the maximum capacity of the ICUs created by the hospital to receive COVID-19 patients was not needed.
COVID-19 positive patients were operated in a surgical room, in a different building, with negative pressure, in order to minimize the contact with the general patients. We did not operate any COVID-19 positive patient.
Half of the surgeries were performed without our usual nursing staff.
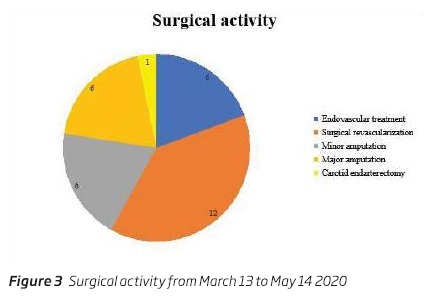
Surgical practice was reduced to only urgent care, totaling 14 patients, 12 of which with critical limb threatening ischemia. The two other surgeries were performed for stump necrosis and neuropathic diabetic foot amputation. No surgeries were performed on COVID-19-positive patients.
In the beginning of the pandemic we decided to increase the number of endovascular procedures to minimize intubation and the use of ventilators, to reduce the potential for exposure to aerosol-generating procedures. This technique could also be beneficial for blood conservation, which is advantageous due to decreased need of blood transfusion. Blood supplies were limited due to restrictions in donations. However, our main goal was always to provide the best and definitive treatment to the patient. According to the following data interventions were evenly split between endovascular and surgical (figure 3).
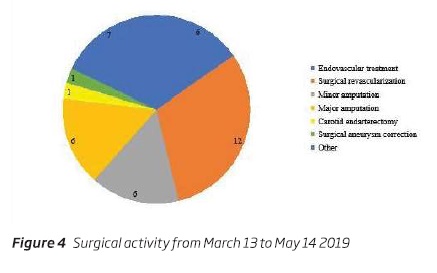
In the same period of the previous year we performed higher number of procedures (31), mainly surgical revascularization and amputations (major and minor). We also operated one patient with an iliac artery aneurysm and performed a carotid endarterectomy in another (figure 4).
We cancelled surgical ambulatory activity, from March 14. In the same period of the previous year 121 patients were submitted to correction of varices.
ICU
Our patients did not require stay in the ICU during the lockdown.
Outpatient Clinics
From March 11, all outpatients were contacted by phone. The healthcare providers of our department called the patients to inform them about the postponement of the activities. We encouraged them to remain home, unless there was an emergency, to limit their exposure to the virus.
They were asked to call in if any priority medical issue affected them, in order to avoid any unnecessary emergency department admission. They were scheduled for a priority observation, if necessary.
However, critical limb threatening ischemia and venous ulcer patients were rigorously scheduled for observation, in order to avoid contact between them.
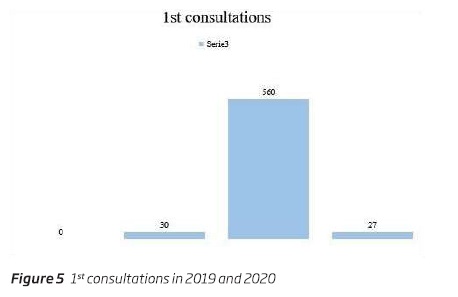
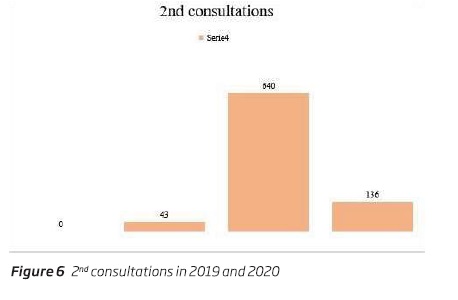
The following graphics show our activity in March 13 to May 14, 2019 and 2020. (figure 5 and figure 6)
There was a significant decrease in our activity and even the phone calls were not enough to balance the restrictions to in-person medical appointments.
Emergency room
A field hospital was created outside the main building to receive the patients with suspected COVID-19 infection, in order to avoid contact between patients. This make-shift building measured 875 m2 and was donated by a local business.
From March 13 to May 14, the Vascular Surgery department saw patients in the emergency department 24/7. Our goal was to avoid the transfer of patients to São Joao Hospital in Oporto. This hospital had its vascular surgeon staff reduced due to COVID-19 infection.
Our Vascular Surgery department tried to minimize the number of concomitant patients in emergency room. In this way, we minimized the presence of priority patients in emergency room. Patients who often needed a prompt observation, but not an emergency one, were scheduled to a priority observation in the outpatient clinics. We called the primary healthcare physician and the general surgeons to organize the referencing of the patients.
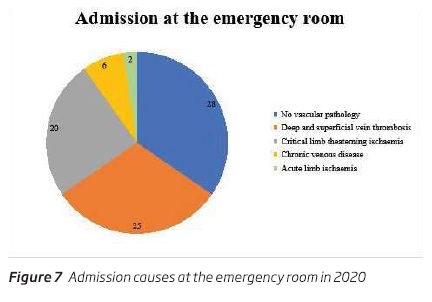
From March 13 to May 14, 81 patients (Mean age: 60.8 years; 52 women) were admitted to Vascular Surgery. The most frequent diagnosis was vein thrombosis (deep or superficial) (figure 7).
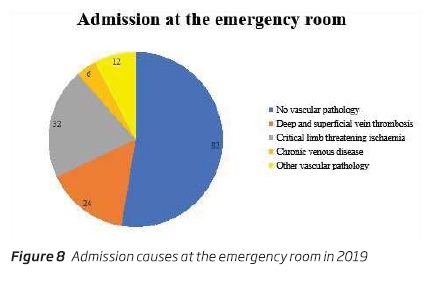
Comparing with the same period of time in the previous year, we admitted 156 patients (Mean age:60.1 years; 72 women). The most frequent diagnosis was also vein thrombosis (figure 8).
The main difference between the pre-pandemic to the pandemic was in the number of patients observed without vascular pathology (82 versus 28).
In selected cases of limb threatening critical ischemia we performed diagnostic angiography at admission in the emergency room to minimize the length of hospital stay. This exam also replaced use of angioCT, which had reduced availability due to the need to scan COVID patients and for thorough cleaning after.
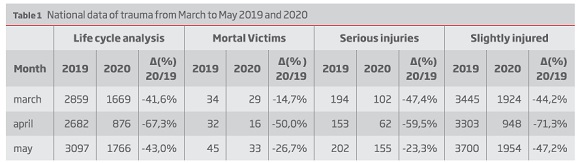
There was a national decrease in trauma patients, (table 1), however we did not notice this difference in our department.
Inpatient admission
The Medicine department had a maximum of 160 patients admitted with COVID-19, which forced the surgical inpatient departments to reduce their admissions. The Vascular Surgery, General Surgery, Orthopedics, Urology and Otolaryngology were restricted to 87 beds from 145 beds, originally.
From March 13 to May 14, 15 vascular patients (11 men, mean age: 65.1 years) stayed in the Vascular Surgery ward. Twelve had critical limb threatening ischemia. There was also one case each of stump necrosis and neuropathic diabetic foot infection and a transfer from an outside hospital for post-operative convalescent care.
We minimized bed occupation time, as well as the patient movement to the hospital to perform the pre-operative evaluation. We admitted the patient in the afternoon before the surgery. The pre-operative study was performed on the day of admission, before the operation. The patient was discharged the day following the operation, if possible. The average stay duration was 3.7 days.
No family visits were allowed since the of March 16.
In the same period of the previous year 48 patients were admitted to the Vascular Surgery ward (29 men; mean age: 70.9 years). The majority of patients had critical limb threatening ischemia. Four patients were admitted for complications of previous interventions, two for acute limb ischemia, one patient for correction of an iliac artery aneurysm and another for carotid endarterectomy. Seven patients were admitted to perform diagnostic angiography and five patients for varices correction. The average stay duration was 6.5 days.
Clinical Trials and Medical Formation
The only ongoing trial in this time period was the Apollo study. Following sponsor recommendation, the investigation protocol was adapted and the included subjects were monitored by phone contact.
Medical teaching and other research activities were canceled.
BIBLIOGRAPHY
1. Imaray C. COVID-19 virus and vascular surgery. Vascular Society for Britain and Ireland, 20th March 2020. [ Links ]
2. https://covid19.apple.com/mobility [ Links ]
3. http://www.ansr.pt/Estatisticas/RelatoriosDeSinistralidade/Documents/2020/Relat%C3%B3rios/Relat%C3%B3rio%20Julho%202020.pdf [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: joana222@gmail.com (J. Ferreira).