Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.15 no.3 Lisboa set. 2019
CASOS CLÍNICOS
Treatment of aortic dissections using a combination of the STABILISE and CERAB techniques - Technical Note
Tratamento de Dissecção da Aorta utilizando uma combinação das técnicas de STABILISE e CERAB - Nota técnica
Ryan Gouveia e Melo1,2,3, Ruy Fernandes e Fernandes1,2,3, Pedro Garrido1,3, Alice Lopes1,3, João Pedro Rato1,3, João Leitão2,3,4 e Luís Mendes Pedro1,2,3
1 Serviço de Angiologia e Cirurgia Vascular, Centro Hospitalar Universitário Lisboa Norte (CHULN)
2 Faculdade de Medicina da Universidade de Lisboa
3 Centro Académico de Medicina de Lisboa
4. Serviço de Imagiologia, Centro Hospitalar Universitário Lisboa Norte (CHULN)
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
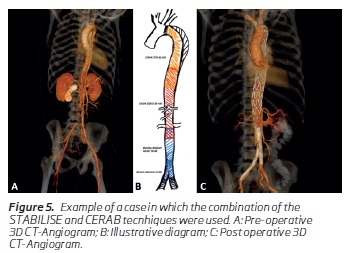
Introduction: Endovascular treatment of type B aortic dissection has focused on the covering of the proximal entry tear. However, recently, concern has emerged regarding the distal aortic remodeling and new techniques such as the Stent-Assisted Balloon-Induced Intimal Disruption and Relamination (STABILISE) technique have gained more acceptance. We describe a technical note regarding the combination of the STABILISE technique in addition to the Covered Reconstruction of the Aortic Bifurcation (CERAB) technique to achieve complete aortic remodeling.
Methods: The authors describe a stepwise approach regarding the endovascular repair of type B aortic dissections. A simple TEVAR is performed first. If the patient still shows signs of true lumen compression, a STABILISE technique is performed in order to achieve true lumen expansion and complete aortic remodeling. However, in some patients, false lumen perfusion and true lumen compression at the very distal aorta is maintained due to distal comunicating tears. In these patients, if there are still signs of infra-renal aortic or iliac compression/occlusion or distal thrombosis of the false lumen, a simultaneous CERAB is performed.
Conclusion: By combining these techniques, we aim to cover both the proximal tear and the distal comunicating tears resulting in a complete flap apposition, false lumen obliteration, re-expansion of the true lumen and achieve optimal remodeling.
Keywords: STABILISE; CERAB, Aortic dissection; Type B aortic dissection; Endovascular repair
RESUMO
Introdução: O tratamento endovascular de dissecções tipo B tem-se focado na cobertura da porta de entrada. No entanto, recentemente, tem surgido a preocupação em relação ao remodeling distal da aorta e novas técnicas como a Stent-Assisted Balloon-Induced Intimal Disruption and Relamination (STABILISE) tem ganho relevo.
Os autores descrevem um nota técnica de uma combinação da técnica de STABILISE com a Covered Reconstruction of the Aortic Bifurcation (CERAB) de forma a obter um remodeling aórtico completo.
Métodos: Neste artigo descreve-se uma abordagem sequencial no tratamento endovascular de dissecções da aorta tipo B. O procedimento é iniciado com um TEVAR simples. Se o doente mantém sinais de compressão do verdadeiro lúmen após a abertura da primeira endoprótese a técnica de STABILISE é realizada sempre que possível de forma a obter expansão do verdadeiro lúmen e remodeling aórtico completo.
No entanto, em alguns doentes, a perfusão do falso e compressão do verdadeiro lúmen mantêm-se devido a portas de re-entrada distais. Nestes doentes, se existirem sinais de oclusão da aorta infra-renal ou iliaca ou ainda a presença de trombose distal do falso lúmen a ténica de CERAB é realizada em simultâneo.
Conclusão:A combinação de ambas as técnicas com o objetivo de cobrir a porta de entrada e as portas de re-entrada distais permite uma união de ambos os flaps, com obliteração completa do falso lúmen, expansão do verdadeiro lúmen e um remodeling aórtico óptimo.
Palavras-chave: STABILISE; CERAB; Dissecção da aorta; Dissecção tipo B da aorta; Reparação endovascular
Introduction
Late aneurysmal degeneration is one of the principal concerns during follow-up of uncomplicated type B aortic dissections (TBAD)(1). Studies evaluating the natural history of these uncomplicated TBAD have shown a high percentage of late complications and a mortality at 5 years of approximately 40%, making the term “uncomplicated” a misnomer(1).For this reason, in the past few years, an attempt at finding morphological and clinical subgroups of these patients has led to a higher degree of patients treated, especially in the sub-acute phase(2,3).
Regarding its repair, endovascular treatment has focused on the covering of the more proximal tear with improvement in both aortic remodeling and survival rates(4).Concern has now emerged regarding the distal aortic remodeling in these patients and new techniques such as the Stent-Assisted Balloon-Induced Intimal Disruption and Relamination (STABILISE) technique have gained more acceptance, with good results shown in the short-term follow-up(5-9).
However, when distal communicating tears are present, the false lumen may maintain its perfusion which can lead to infra-renal aortic true lumen compression, iliac occlusion or late aneurysmal degeneration. For these patients, a combination of the STABILISE and the CERAB(10) (Covered Endovascular Reconstruction of Aortic Bifurcation) techniques may be employed in order to improve remodeling and long-term results.
The authors aim to describe the technical details of this combination of techniques.
Tecnhical description:
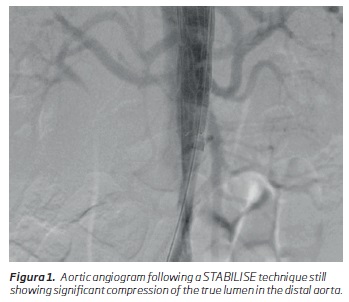
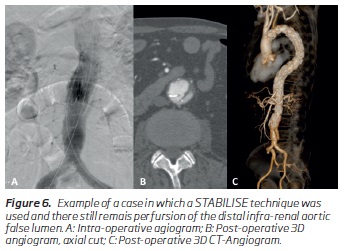
Regarding any surgical technique, patient selection is paramount. There is a small niche of patients in which a combination of the STABILISE and CERAB techniques may be applied. We can consider them a subgroup of the patients that have an indication for TEVAR and STABILISE. In the management of TBADs, first, a decision has to be made if the patient warrants treatment, and if he is applicable for a TEVAR. If the TEVAR is performed and there is still false lumen perfusion and true lumen compression distally in the control angiogram following the endograft placement, an extension using the STABILISE technique may be used. In these patients, if there are still signs of infra-renal aortic or iliac compression/occlusion or distal thrombosis of the false lumen (Figure 1), a CERAB may be performed in order to expand the true lumen and occlude these distal communicating tears.
When a decision is made to treat a patient with a TBAD, it is advised to have a pre-operative CT-angiography (CTA) with at least 1mm cuts in order to plan these procedures, ideally an ECG-gated CTA. At least a 2cm dissection-free proximal landing zone (PLZ) should be obtained in order to achieve adequate sealing, fixation and lower risk for stent induced new entry tears which may lead to retrograde dissections. The aortic diameter at the level of the PLZ is measured (outer to outer) and 10% oversizing is performed using a covered endograft, ideally without proximal bare fixation stents. The aortic diameter in the distal thoracic and abdominal aorta is also measured including both true and false lumens (outer-to-outer) and a plan for a same size graft is made (no oversizing). In the distal aorta and iliacs, the total diameter is also measured including both true and false lumens and a 10% oversizing is used if using covered stents.
The authors perform these procedures in an angiographic suite using the Azurion system from Philips®.
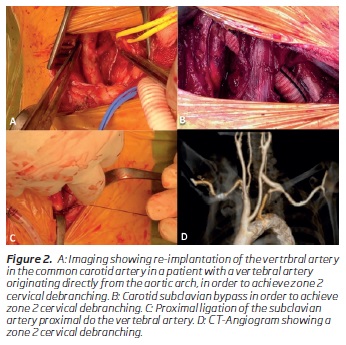
Depending on the patient, in order to achieve an adequate PLZ (more than 2cm of non-dissected aorta), an arch debranching procedure may be needed. Usually a carotid-subclavian bypass using a Dacron 8mm graft is performed Figure 2A,B), followed by, simultaneous ligation of the subclavian artery proximal to the vertebral artery (Figure 2C) whenever possible in order to lower the risk of posterior stroke when opening the endograft in a subsequent phase (Figure 2D).
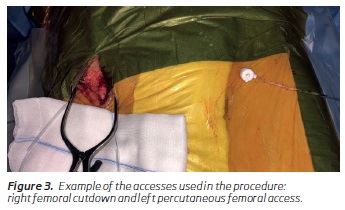
Both femoral accesses are used, one femoral cutdown and one percutaneous. The femoral cutdown access is chosen on the side that looks easier to catheterize the true lumen and advance the aortic devices and purse string sutures are placed in order to rapidly perfuse the limb whenever possible (Figure 3).
If there is a plan to cover more than 15cm of thoracic aorta, or if the patient has already been submitted to abdominal aortic surgery or has hypogastric artery occlusion, the procedure is performed using spinal fluid drainage.
Regarding device selection, for the proximal TEVAR the authors usually choose the COOK Zenith Dissection TX2 device without proximal bare metal fixation stents. However, when not available, the device at hand is used, which, in our institution, is the COOK Zenith Thoracic Alpha and attention is made not to land the bare metal fixation stents on a dissected aorta or with intramural hematoma. A 10% oversizing is used in the proximal landing zone and if an extension is used, the total aortic diameter is used (true plus false lumen) with no oversizing. For the STABILISE extension, a bare metal stent like the COOK Zenith Dissection (ZDES) is used and measured according to the total aortic diameter.
For the CERAB, balloon expandable covered stent grafts are used. Due to more diameter options available the Bentley BeGraft Aortic stent graft is usually used and measured to a 10% oversizing of the total aortic diameter. For the iliac stent, either the Bentley BeGraft Peripheral or Atrium Advanta stents are used.
The procedure is started by catheterizing the true lumen using a hydrophilic 0,035 guidewire over a pigtail, making sequential angiographic checks to make sure one is correctly placed in the true lumen and advancing it all the way to the ascending aorta making one final angiogram to confirm the position. The guidewire is then exchanged to a stiff wire, usually a Lunderquist Extra Stiff wire, which is placed next to the aortic valve. Over this wire a 6F long sheath is advanced to the proximal aorta and a serial of angiographies are performed from proximal do distal to confirm positioning in the true lumen in all of the extent of the aorta.
On the contralateral side, a pigtail is advanced in the same way to the proximal aorta where it “sits” in order to perform the angiograms.
The first endograft is advanced over the stiff wire and the position is confirmed with an angiogram. The endograft is then deployed immediately distal to the left carotid or subclavian artery, depending on the target landing zone. A quick angiogram is performed to confirm the position and the pigtail is removed backwards and positioned inside the endograft. At this time, a complete aortic angiogram is performed in order to evaluate the aortic remodeling. If true lumen compression is still seen, a STABILISE technique is performed.
A second covered endograft extension is usually avoided except when large communicating tears are seen at this level in the pre-operative CTA. In these cases, a covered endograft may be deployed, ending just above the celiac trunk, using full lateral view in order to confirm its origin. A 5cm overlap is used.
When a covered extension is not used, a bare metal aortic stent is used (the authors usually use the COOK® Dissection ZDES) with the same overlap. Usually in these cases two BMS are needed and the first is aimed to be deployed above the celiac trunk in order to avoid placing two BMS over the visceral arteries as it might hinder future vessel catheterization if needed. A 5cm overlap on the second BMS is also used and aimed to deploy above the iliac bifurcation, usually about 3cm.
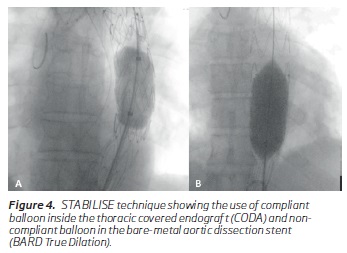
Following the placement of all the components, a semi-compliant (COOK CODA®) balloon is used to balloon the covered endograft to its maximal nominal diameter rupturing the dissection flap and re-laminating the aorta (Figure 4A). This balloon is not used in the BMS zone due to the risk of rupture. In this area a non-compliant balloon is used (BARD® True Dilation), with the same size as the BMS in order not to dilate the aorta beyond its diameter Figure 4B). If after 3 attempts the flap does not rupture and there is no apposition, no additional ballooning is performed.
After all the stents have been ballooned, an angiogram is performed to evaluate the distal aorta. If there are signs of true lumen compression with aortic/iliac compression/occlusion or distal false lumen thrombosis (Figure 1), a CERAB technique is performed.
First, an aortic endograft (Bentley® Aortic BeGraft) is placed just below the renal arteries. After deployment, the proximal two thirds of the graft are ballooned, using the same non-compliant balloon used for the STABILISE. The iliac stent-grafts are then deployed in a kissing stent fashion placed at least 2cm inside the aortic stent-graft. (Figure 5)
A pigtail is then placed in the ascending aorta and a final aortic angiogram is performed and an attentive look is made on the visceral arteries to check for any dissection flaps and correct perfusion.
Following the procedure, normally patients recover immediately with normalization of blood pressure and resolution of the chest/abdominal pain. If this is not the case, a repeat CTA is performed to check for signs of complication.
If the patient recovers well, we will perform a CTA on the first week before discharge and then after one month, 6 months and yearly thereafter.
Patients are kept under dual antiplatelet therapy and strict anti-hypertension control.
Discussion/conclusion:
Aortic dissections are an unpredictable and complex conundrum. In order to improve the care of patients with TBADs one has to pay special attention to the different characteristics of the particular patient’s anatomy and presentation.
Currently type B aortic dissections have been divided accordingly to their timing in acute, sub-acute and chronic dissections(2). Regarding an endovascular repair in patients with uncomplicated TBADs. The acute phase (first 14 days) has been historically avoided by most authors with the fear of rupture and complications. The ADSORB trial, however, showed safe outcomes with better remodeling in this phase, albeit with no differences regarding mortality(11). Recently, authors have described favorable and safe outcomes of patients treated in this setting even with more extensive repairs like the STABILISE technique as described by Melissano et al(7). The exception for this, is the hyperacute phase (first 24h) in which the aorta seems to be more prone to rupture and surgery should be avoided, if possible. However, if necessary, proceeding with a PETTICOAT (Provisional Extension To Induce Complete Attachment) technique and then ballooning it in the sub-acute phase may be safer if one fears aortic rupture(12).
The subacute phase (14-92 days) has been considered the ideal phase, due to the aorta still maintaining its elasticity and having a lower risk of rupture and complications, with favorable results in both remodeling and mortality(3,4,13). In the chronic phase (after 92 days), results have shown a lack of remodeling and there is no evidence currently regarding better future outcomes in uncomplicated patients(13).
Another important definition which mainly influences the choice for a repair is the presence of complications(1).The presence of malperfusion, uncontrolled pain and hypertension and rapid growth are considered signs of complication designating them as complicated dissections which warrant treatment. TBADs in which these factors are not observed have been considered to be uncomplicated and have been historically left for best medical therapy. However, studies evaluating the natural history of these uncomplicated TBAD have shown a high percentage of late complications and a mortality at 5 years of approximately 40%, making the term uncomplicated a misnomer(1,3).
Regarding this fact, new factors have been described which have tried to find clinical or anatomic factors which are related to worse outcomes with the objective of creating subgroups in which early treatment would be beneficial(14).
So far, some relevant criteria have been found, and in which we also use as a criteria for treatment in “uncomplicated dissections”: false lumen diameters over 22mm, entry tears on the inner concave curve of the aorta, entry tears over 10mm in diameter, patent true lumen with elliptical configuration and patent or partially thrombosed false lumen(3,14).
In these patients the focus has been on the coverage of the more proximal entry tear with a TEVAR, with favorable results in the long term follow-up as demonstrated in the INSTEAD-XL(4). However, in these patients, when significant false lumen perfusion exists in the distal aorta, significant morbidity regarding aneurysm degeneration can occur (15,16). In these patients, new techniques such as the PETTICOAT(17) and STABILISE techniques have emerged as a solution for this, which aim at increasing the durability of the repair and preventing future aneurysm degeneration.
The STABILISE technique has shown, so far, excellent results in the short and mid-term follow-up, being demonstrated as both feasible and safe(7-9). However, in order to perform the STABILISE technique one has to follow the indications shown in the literature so far, avoiding treatment of patients with a total aortic diameter over 42mm or patients without an adequate proximal landing zone or if one cannot be achieved by supra-aortic vessel debranching(7).
In some patients, even following placement of a distal bare-metal stent, like the STABILISE technique, false lumen perfusion and true lumen compression at the very distal aorta still persists due to distal communicating tears(6) (Figure 6). In these patients, if there are still signs of infra-renal aortic or iliac compression/occlusion or distal thrombosis of the false lumen, a CERAB may be performed in order to expand the true lumen and occlude these distal communicating tears.
This concept has been explored the Molinari et al using the DEEVAR technique, in which they combine the PETTICOAT technique and place an AFX unibody in the aortic bifurcation aiming to occlude the distal communicating tears(18).
In this paper we describe a similar concept but associating the STABILISE and CERAB techniques.
Conclusion:
The technical details of the combination of the STABILISE and CERAB techniques to treat type B aortic dissections are described. This combination allows for a covering of both the proximal tear and the distal communicating tears which aims to lead to a complete flap apposition, false lumen obliteration and optimal remodeling.
In adequate patients it might lead to a more complete and durable repair.
REFERENCES:
1. Durham CA, MD, Cambria RP, Wang LJ, Ergul EA, Aranson NJ, et al. The natural history of medically managed acute type B aortic dissection.J Vasc Surg 2015;61:1192-9. [ Links ]
2. Steuer J Björck M, Mayer D Wanhainen A, Pfammatter T, Lachat M. Distinction between Acute and Chronic Type B Aortic Dissection: Is there a Sub-acute Phase? EJVES. 2013; Vol 45: 627-631. [ Links ]
3. Verhoeven ELG et al., Looking for the Holy Grail in Acute/Subacute Type B Dissection. Eur J Vasc Endovasc Surg. 2019; 57: 615-616. [ Links ]
4. Nienaber CA, Kishe S, Rousseau H, Eggebrecht H, Rehders TC, Kundt G, et al. Endovascular Repair of Type B Aortic Dissection. Long-term Results of the Randomized Investigation of Stent Grafts in Aortic Dissection Trial. Circ Cardiovasc Interv. 2013;6:407-416. [ Links ]
5. Lombardi JV, Cambria RP, Nienaber CA, Chiesa C, Teebken O, Lee A, et al. Prospective multicenter clinical trial (STABLE) on the endovascular treatment of complicated type B aortic dissection using a composite device design. J Vasc Surg 2012;55:629-40. [ Links ]
6. Canaud L, Faure E, Ozdemir BA, Alric P, Thompson M. Systematic review of outcomes of combined proximal stent-grafting with distal bare stenting for management of aortic dissection. Ann Cardiothorac Surg 2014;3:223-33. [ Links ]
7. Melissano G, Bertoglio L, Rinaldi E, Mascia D, Kahlberg A, Loschi D, et al. Satisfactory short-term outcomes of the STABILISE technique for type B aortic dissection. J Vasc Surg 2018;68: 966-75. [ Links ]
8. Hofferberth SC, Nixon IK, Boston RC, McLachlan CS, Mossop PJ. Stent-assisted balloon-induced intimal disruption and relamination in aortic dissection repair: the STABILISE concept. J Thorac Cardiovasc Surg 2014;147:1240-5. [ Links ]
9. Faure EM, Batti SE, Rjeili MA, Julia P, Alsac JM. Mid-term outcomes of stent assisted balloon induced intimal disruption and relamination in aortic dissection repair (STABILISE) in acute type B aortic dissection. Eur J Vasc Endovasc Surg 2018;56:209-15. [ Links ]
10. Grimme FA, Goverde PC, Verbruggen PJ, Zeebregts CJ, Reijnen MM. First Results of the Covered Endovascular Reconstruction of the Aortic Bifurcation (CERAB) Technique for Aortoiliac Occlusive Disease. Eur J Vasc Endovasc Surg (2015) 50, 638-647 [ Links ]
11. Kamman AV, Brunkwall J, Verhoeven EL, Hejimen RH, Trimarchi S. Predictors of aortic growth in uncomplicated type B aortic dissection from the Acute Dissection Stent Grafting or Best Medical Treatment (ADSORB) database. Eur J Vasc Endovasc Surg. 2013; 45: 627-631. [ Links ]
12. Lopes A, Melo RG, Gomes ML, Garrido P, Junqueira N, Sobrinho G, et al. Aortic Dissection Repair Using the STABILISE Technique Associated with Arch Procedures: Report of Two Cases EJVES Short Reports 2019. 42: 26-30 [ Links ]
13. The VIRTUE Registry Investigators. Mid-term Outcomes and Aortic Remodelling After Thoracic Endovascular Repair for Acute, Subacute, and Chronic Aortic Dissection: The VIRTUE Registry. Eur J Vasc Endovasc Surg. 2014. 48: 363-371 [ Links ]
14. Spinelli D, Benedetto F, Donato R, Piffaretti G, Marrocco-Trischitta MM, Patel HJ, et al. Current evidence in predictors of aortic growth and events in acute type B aortic dissection. J Vasc Surg. 2018. 68: 1925-1935 [ Links ]
15. Fattori R, Montgomery D, Lovato L, Kische S, Di Eusanio M, Ince H, et al. Survival after endovascular therapy in patients with type B aortic dissection: a report from the International Registry of Acute Aortic Dissection (IRAD). JACC Cardiovasc Interv 2013;6:876-682. [ Links ]
16. Faure EM, Canaud L, Agostini C, Shaub R, Böge G, Martyané C, et al. Reintervention after thoracic endovascular aortic repair of complicated aortic dissection. J Vasc Surg 2014;59:327-333. [ Links ]
17. Bertoglio L, Rinaldi E, Melissano G, Chiesa R.The “Petticoat” concept for endovascular treatment of Type B aortic dissection. J Cardiovasc Surg. 2019 60(1):91-99
18. Molinari AC, Leo E, Ferraresi M, Ferrari SA, Terzi A, Sommaruga S, et al. Distal Extended EndoVascular Aortic Repair (DEEVAR) Petticoat: a modified technique to improve false lumen remodeling in acute type B aortic dissection. Ann Vasc Surg. 2019 59:300-305. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: ryan@campus.ul.pt (R. Melo).
Declaration of interest:
This work was not presented in any congress and we did not receive any funding from industry.
Recebido a 15 de junho de 2019
Aceite a 04 de novembro de 2019