Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.15 no.2 Lisboa jun. 2019
CASOS CLÍNICOS
A hybrid solution to manage a thoracoabdominal aortic aneurysm: the “simplified technique” associated to endografting of the proximal aortic anastomosis
Uma solução híbrida para o tratamento de um aneurisma toracoabdominal: a “técnica simplificada” associada a implantação de endoprótese na anastomose aórtica proximal
Tony R. Soares1,2, Pedro Amorim1,2,3, Carlos Martins1,2, Viviana Manuel1,2, Emanuel Silva1,2, Mariana Moutinho1,2, João Rato1,2, Luís Silvestre1,2,3, Luís Mendes Pedro1,2,3
1 Department of Vascular Surgery, Hospital Santa Maria (CHULN), Lisbon, Portugal
2 Lisbon Academic Medical Centre, Lisbon, Portugal
3 University of Lisbon, Lisbon, Portugal
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Thoracoabdominal aortic aneurysms (TAAA) remain a therapeutic challenge for vascular surgeons. We report a Crawford extent type III TAAA managed with the “simplified technique” to approach TAAA associated to endograft implantation in the proximal aortic anastomosis to minimize the risk of blowout of the aortic stump.
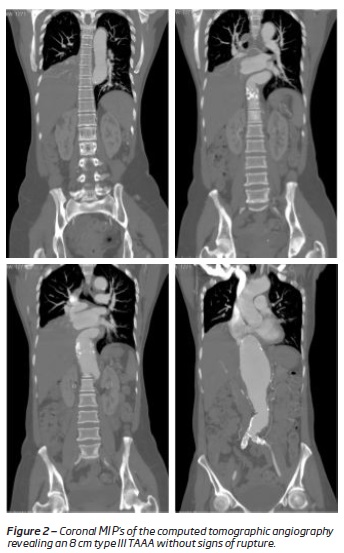
Case Report: A 43-year-old female patient was evacuated from Mozambique with a history of TAAA and admitted in our emergency department with recent chest and abdominal pain. She had history of HIV infection and pulmonary tuberculosis. The physical examination revealed a painful, pulsatile abdominal mass and the computed tomographic angiography (CTA) an 8cm type III TAAA without signs of rupture.
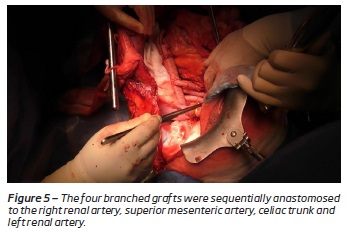
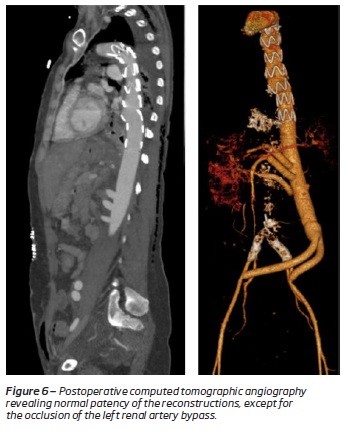
The aneurysm morphology was not adequate for endovascular treatment and, due to the immediate unavailability of the usual adjuncts for Crawford technique (ECC and selective visceral perfusion), this symptomatic patient was submitted to a thoraco-phreno-laparotomy with left medial visceral rotation. A bifurcated Dacron 18x9mm graft was distally anastomosed in an end-to-side fashion to both external iliac arteries and proximally to a 22mm polyester four branched graft (Jotec®). This later graft was proximally anastomosed to the descending thoracic aorta (end-to-side) with no visceral or renal ischemia. The aorta distal to the anastomosis was then cross-clamped as well as the infra-renal segment, the aneurysm opened, and no patent intercostal arteries were visible. The lower limb perfusion was maintained by the lateral shunt. Both kidneys were cooled with lactated Ringer’s solution through Pruitt catheters and the visceral arteries were temporarily occluded with Fogarty catheters. The four anastomoses were sequentially performed to the right renal artery, superior mesenteric artery, celiac trunk and left renal artery. After completing all the reconstructions, a Zenith Alpha® 32x155mm endograft was implanted from the descending thoracic aorta to the pre-branch segment of the lateral shunt. The operation was uneventful, and the patient remained hemodynamically stable. The postoperative period was complicated by pulmonary infection and the postoperative CTA revealed the occlusion of the left renal artery graft (without clinical or laboratory repercussion). The patient was discharged 50 days after the operation due to social reasons.
Conclusion: The adjunct of an endograft to the “simplified technique” was previously described and allows to overcome the risk of aortic stump blowout which is one of the major limitations of this technique. This strategy was a successful alternative to manage a TAAA since organ-protection adjuncts to the Crawford technique were not available.
Keywords: Thoracoabdominal aortic aneurysms; endograft; open surgery; simplified technique
RESUMO
Introdução: O aneurisma da aorta toracoabdominal (ATA) persiste um verdadeiro desafio para o cirurgião vascular. O presente trabalho descreve o caso clínico de um ATA de tipo III (classificação de Crawford) tratado segundo a “técnica simplificada”, associado à implantação de uma endoprótese na anastomose aórtica proximal de forma a minimizar o risco de rotura do coto aórtico.
Caso Clínico: Uma paciente do sexo feminino, de 43 anos de idade, procedente de Moçambique, foi evacuada do seu país e admitida no nosso serviço de urgência por dor torácica e abdominal crónica, com agravamento nos últimos dias. A doente tinha como antecedentes pessoais infeção por HIV e história de tuberculose pulmonar. Ao exame objetivo revelou uma massa abdominal pulsátil e dolorosa, e a angiotomografia computadorizada (angioTC) confirmou um ATA tipo III de 8cm de maior diâmetro, sem sinais de rotura.
O tratamento endovascular não se mostrou ser opção viável derivado à morfologia do aneurisma e, devido à indisponibilidade pontual dos habituais métodos adjuvantes à técnica de Crawford (CEC e perfusão visceral seletiva), optou-se por tratar a paciente utilizando a “técnica simplificada”. Desta forma, foi submetida a uma toracofrenolaparotomia com rotação visceral medial esquerda. Uma prótese bifurcada de Dacron 18x9mm foi anastomosada às artérias ilíacas externas e proximalmente a um enxerto de poliéster de 22 mm com quatro ramos (Jotec®). Por sua vez, foi construída uma anastomose à aorta torácica descendente (término-lateral) com clampagem parcial da aorta de forma a permitir uma contínua perfusão visceral e renal. Por fim, procedeu-se à clampagem do segmento da aorta distal à anastomose proximal e da aorta infra-renal para abertura e ressecção parcial do aneurisma. A perfusão dos membros inferiores foi mantida pelo shunt lateral. Ambos os rins foram perfundidos com solução de lactato de Ringer e as artérias viscerais foram temporariamente ocluídas com cateteres de Fogarty. As quatro anastomoses foram sequencialmente realizadas para a artéria renal direita, artéria mesentérica superior, tronco celíaco e a artéria renal esquerda. Por fim, foi implantada uma endoprótese Zenith Alpha® 32x155mm na aorta torácica descendente de forma a excluir o coto aórtico. A operação decorreu sem intercorrências. O período pós-operatório foi complicado de uma infeção pulmonar, e a angioTC revelou a oclusão do enxerto da artéria renal esquerda (sem repercussão clínica ou laboratorial). A paciente teve alta 50 dias após a operação por motivos sociais.
Conclusão: A exclusão do coto aórtico na “técnica simplificada” com implantação de uma endoprótese aórtica foi previamente descrita e permite controlar umas das principais limitações desta técnica. Essa estratégia foi uma alternativa bem-sucedida para abordar um ATA, já que os métodos adjuvantes de proteção de órgãos não se encontravam disponíveis.
Palavras-chave: Aneurisma thoracoabdominal; endoprótese; cirurgia convencional; técnica simplificada
Introduction
Thoracoabdominal aortic aneurysms (TAAA) remain a therapeutic challenge for vascular surgeons. Despite the advances in endovascular techniques, open repair is still the gold standard for some patients, mostly of them employing the “inclusion technique” described by Crawford et al.(1-5) In 1984, Da Gama et al introduced a conceptually simpler open technique, avoiding the need of adjuvant techniques such as left heart or cardiopulmonary bypass and selective visceral perfusion. This approach, commonly named “simplified technique”, was based in an aorto-aortic or aorto-iliac lateral shunt followed by direct splanchnic and renal revascularization(6). However, this technique has some drawbacks including the risk of aortic stump blowout, as the proximal anastomosis of the lateral shunt is tailored in an end-to-side fashion.
We report a modification of this technique in a patient with a Crawford extent type III TAAA managed with the “simplified technique” associated to endograft implantation in the proximal aortic anastomosis thus avoiding he risk of blowout of the aortic stump.
Case report
A 43-year-old female patient was evacuated from Mozambique and admitted in our emergency department with a history of TAAA already identified and recently complaining of chest and abdominal pain. She had a history of pulmonary tuberculosis 10 years ago and HIV infection under retroviral therapy for 19 years with undetectable HIV viral load.
The physical examination revealed a painful, pulsatile and expandable large abdominal mass, and the computed tomographic angiography (CTA) an 8 cm type III TAAA without signs of rupture (Figures 1 and 2).
The aneurysm morphology was not adequate for endovascular due to several reasons. First, both renal arteries were very thin (3.9-4 mm) and the right renal artery had a steep upward orientation (not amenable for cannulation from an off-the-shelf branched endograft). Also, this symptomatic patient could not wait for the design and manufacturing of a custom-made device. Finally, the common iliac arteries were severely calcification, potentially limiting the adequacy of distal sealing zones. The above-mentioned reasons were also a limitation for abdominal hybrid techniques (with debranching and endografting).
Due to the immediate unavailability of the usual adjuncts for the Crawford technique(7) (extracorporeal circulation and selective visceral perfusion) and facing a symptomatic TAAA not amenable to endovascular treatment, the patient was proposed for an open approach using the "simplified technique" concept combined with endovascular "protection" of the aortic stump.
The patient was then submitted to a thoraco-phreno-laparotomy with left medial visceral rotation.
A bifurcated Dacron 18x9mm graft was distally anastomosed in an end-to-side fashion to both external iliac arteries (Figure 3), due to the heavy calcification of both common iliacs, and proximally to a 22mm polyester four branched graft (FlowWeave® plus from Jotec®). This later graft was proximally anastomosed in an end-to-side fashion to the descending thoracic aorta using partial clamping to maintain visceral and renal perfusion (Figure 4).
At this moment, the aneurysm was still normally perfused. The aorta distal to the anastomosis of the lateral shunt was then cross-clamped as well as the infra-renal segment, the aneurysm was opened, and no patent intercostal arteries were visible. The lower limb perfusion was maintained by the aorto-iliac lateral shunt. Both kidneys were perfused with cold (4oC) Ringer’s lactate solution through Pruitt® catheters to maintain low renal temperature and preserve renal function. Visceral arteries were temporarily occluded with Fogarty® catheters. The four anastomoses of the dacron graft branches to the target vessels were sequentially performed to the right renal artery, superior mesenteric artery, celiac trunk and left renal artery with ischemic times of 14, 22, 35 and 49 minutes, respectively (Figure 5). This step of the operation was completed by ligation of the infra-renal aorta.
After completing all the reconstructions, the lateral shunt was catheterized and a 32x155mm Zenith Alpha" Thoracic Endovascular Graft from Cook® was implanted from the descending thoracic aorta to the pre-branch segment of the lateral shunt, across the proximal anastomosis, which was "converted" in an end-to-end anastomosis. Finally, the thoracic aorta distal to the lateral shunt was ligated and the clamp removed.
The operation was uneventful, and the patient remained hemodynamically stable during the procedure, maintaining a normal urinary output.
The postoperative period was complicated by a pulmonary infection treated medically.
The postoperative CTA revealed the occlusion of the left renal artery graft without clinical or laboratory repercussion (Figure 6).
Due to social reasons, the patient was discharged 50 days after the operation and returned to Mozambique.
Discussion
Open surgical repair remains the gold standard approach to treat some TAAA, particularly in very young patients, with connective tissue disorders, when there is evidence of infection, in complications of previous endovascular treatments, or simply when the anatomy is not appropriate for an endoluminal strategy.
In 1974, Crawford et al published the “inclusion technique” that is based in an intra-aortic anastomosis without total aneurysmectomy(7) combined with the in-lay reconstruction of the visceral and renal arteries using a visceral patch or separate grafts to the target arteries.
In 1986, Crawford et al published a series of a total of 605 patients with a 30-day mortality rate of 8.9% with no adjunct measures except, cold Ringer’s lactate solution of the left renal artery.(1) However, later on, Crawford and his group recognized the usefulness of adjuncts capable of maintain organ perfusion during aortic cross-clamping and their influence in the improvement of the results. Contemporary outcomes of high-volume centers have adopted multiple end-organ protective strategies achieving early mortality rates between 5 and 8%.(3-5) These measures include a left heart bypass (left atrium to left femoral or aneurysm) or a cardiopulmonary bypass (left femoral vein to left femoral artery), to dynamically manage the pressure balance above and below the aortic clamp and to maintain the perfusion of the lower limbs and hypogastric arteries. Also, the selective perfusion of the renal (blood, cold lactate, Custodial®) and visceral arteries (blood) using an octopus system allows the maintenance of flow to the bowels and liver and at the same time protects the kidneys from the ischemic effects, decreasing the rate of renal failure. The spinal cord is protected by cerebrospinal fluid drainage and its function is monitorized by evoked potentials techniques during the operation. In case of loss of these potentials, intercostal arteries are reimplanted and higher blood pressure levels are achieved.(8-10) All these end-organ protective adjuncts to the “inclusion technique” represent essential tools for the modern management of TAAA to minimize renal, mesenteric, and spinal cord ischemia. We systematically use this approach in our department.
In the present case, for logistic reasons, it was not possible to use the strategy previously described in an urgent setting to manage a symptomatic 8 cm type III TAAA. Our option was then to perform a “simplified technique” described by Da Gama et al in 1984 and used frequently in our department for 20 years. This technique is based in creating an aorto-aortic or aorto-iliac lateral shunt, maintaining distal aortic perfusion during the cross-clamping period, followed by splanchnic and renal direct revascularization after opening of the aneurysm sac.(6) The proximal anastomosis of this shunt is end-to-side, thus leaving in the end of the operation a stump vulnerable to rupture.
This technique avoids the need of the mentioned adjuncts and the use of large amounts of heparin but has some disadvantages. In first place, the lateral shunt is passive, and the flow cannot be modified according to the the blood pressure dynamics during the operation. Second, it doesn't include selective visceral and renal perfusion during the clamping period and acceptable ischemic times can simply be achieved by the quick performance of sequential anastomosis by the surgeon. In third place, the aortic stump is left behind and is susceptible to blowout. To minimize this potentially fatal complication, the implantation of an aortic endograft from the descending thoracic aorta to the pre-branch segment of the lateral shunt was described in a technical note by a Brazilian group(11) thus excluding the stump and "converting" an endo-to-side anastomosis into an endo-to-end anastomosis.
This approach was successful to surgically manage our patient.
In the post-operative CT scan, an occlusion of the left renal artery was identified and possibly related to an acute angulation of the transition between the renal graft and the distal renal artery. However, it was not related to any clinical significance.
Conclusion
The endograft implantation in the proximal aortic anastomosis of the “simplified technique” allows to overcome the risk of aortic stump blowout, which is one of the major limitations of this technique. In the reported case, this strategy was a successful alternative to manage a TAAA as the usual organ-protection adjuncts to the Crawford technique were not available.
REFERENCES
1. Stanley Crawford, E. et al. Thoracoabdominal aortic aneurysms: Preoperative and intraoperative factors determining immediate and long-term results of operations in 605 patients. J. Vasc. Surg. 3, 389-404 (1986). [ Links ]
2. Chiesa, R. et al. Management of thoracoabdominal aortic aneurysms. HSR Proc. Intensive Care Cardiovasc. Anesth. 1, 45-53 (2009). [ Links ]
3. Coselli, J. S., Bozinovski, J. & LeMaire, S. A. Open Surgical Repair of 2286 Thoracoabdominal Aortic Aneurysms. Ann. Thorac. Surg. 83, S862-S864 (2007). [ Links ]
4. Svensson, L. G., Crawford, E. S., Hess, K. R., Coselli, J. S. & Safi, H. J. Experience with 1509 patients undergoing thoracoabdominal aortic operations. J. Vasc. Surg. 17, 357-370 (1993). [ Links ]
5. Conrad, M. F., Crawford, R. S., Davison, J. K. & Cambria, R. P. Thoracoabdominal Aneurysm Repair: A 20-Year Perspective. Ann. Thorac. Surg. 83, S856-S861 (2007). [ Links ]
6. Da Gama, A. A simplified technique for the surgical treatment of aneurysms of the thoraco-abdominal and the upper abdominal aorta. J. Cardiovasc. Surg. (Torino). 25, 505-9 (1984). [ Links ]
7. CRAWFORD, E. S. Thoraco-Abdominal and Abdominal Aortic Aneurysms Involving Renal, Superior Mesenteric, and Celiac Arteries. Ann. Surg. 179, 763-772 (1974). [ Links ]
8. Kouchoukos, N. T., Masetti, P., Rokkas, C. K., Murphy, S. F. & Blackstone, E. H. Safety and efficacy of hypothermic cardiopulmonary bypass and circulatory arrest for operations on the descending thoracic and thoracoabdominal aorta. Ann. Thorac. Surg. 72, 699-708 (2001). [ Links ]
9. Svensson, L. G. et al. Reduction of neurologic injury after high-risk thoracoabdominal aortic operation11This article has been selected for the open discussion forum on the STS Web site: http://www.sts.org/annals. Ann. Thorac. Surg. 66, 132-138 (1998).
10. Jacobs, M. J. H. M. et al. Reduced renal failure following thoracoabdominal aortic aneurysm repair by selective perfusion1. Eur. J. Cardio-Thoracic Surg. 14, 201-205 (1998). [ Links ]
11. Espinosa, G. et al. Proximal endovascular blood flow shunt for thoracoabdominal aortic aneurism without total aortic clamping. Rev. Col. Bras. Cir. 42, 189-192 (2015). [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: tony.ramos.soares@gmail.com (T. Soares).
Recebido a 14 de junho de 2019
Aceite a 17 de agosto de 2019