Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.13 no.3 Lisboa dez. 2017
CASO CLÍNICO
Transapical access — a complementary access for tevar in a stanford type a dissection
Acesso transapical- um acesso complementar para tevar na dissecção aortica tipo a de stanford
Inês Antunes1, Rui Machado 1,2, Luís Loureiro1, Carlos Pereira1, Duarte Rego1, Vitor Ferreira1, João Gonçalves1, Gabriela Teixeira1, Carlos Veiga1, Daniel Mendes1, Rui de Almeida1,2
1Serviço de Angiologia e Cirurgia Vascular, Centro Hospitalar do Porto, Hospital de Santo António
2Instituto de Ciências Biomédicas Abel Salazar
Autor para correspondência
ABSTRACT
Introduction/Objectives: Type A aortic dissection (AD) usually requires urgent surgical treatment and aortic segment replacement remains the gold standard. However, it is a very aggressive procedure and some patients are considered too frail for this treatment. Nowadays, endovascular repair represents an alternative treatment but still without precise indications. Our objective is to present a case of hybrid treatment of a type A AD with resource a transapical cardiac access.
Material/Methods: Clinical case and literature review.
Results: A 65-year-old man with history of chronic pulmonary obstructive disease, atrial fibrillation and hypertension came to the emergency department with abdominal pain. He underwent angio-CT that revealed type A AD with an PAU in the ascending aorta (AA). After evaluation by cardiac surgery, he was considered too frail for conventional surgery. Angio-CT was repeated after two weeks of medical treatment and revealed false aneurysm growth, with imminent risk of rupture. We thought about endovascular treatment and different options were considered, the final decision was to propose the patient for an hybrid treatment. The procedure was started with a femoro-rigth axilar bypass and embolization of the brachyocephalic trunk. Then an endoprosthesis (Valiant®) was delivered below the left subclavian artery and two periscopes (Viabahn®) were progressed form left carotid and axillar arteries and the second endoprosthesis (Valiant®) was released into the aorta, inside the first, with coverage of the left common carotid and subclavian, and the Viabahn® were released. After multiple attempts, it was not possible to progress the third endoprosthesis AA because of lack of support and hemodynamic instability whenever the guidewire was progressed for the left ventricle and the procedure was interrupted. Subsequently performed angio-CT revealed permeable AA dissection and untreated false aneurysm. We discussed other options and an anterograde (transapical) approach was considered to progress a guidewire on through-and-through to achieve the support we need to progress the endoprothesis. With the support of the cardiac surgery the cardiac apex was punctured and using the through-and-through technique the guide wire was progressed to femoral artery which allowed advancement of the endoprosthesis (Valiant®) through the retrograde pathway and release under rapid-pacing in the AA with good final result.
Discussion/Conclusions: Endovascular treatment is an alternative in patients of high clinical risk and adequate anatomical characteristics, yet technically challenging. When the retrograde progression of the endoprosthesis is not achieved, the transapical cardiac approach is an alternative to be considered.
Keywords: Transapical access; endovascular treatment; type A aortic dissection
RESUMO
Introdução/Objetivos: A dissecção aórtica tipo A (AD) geralmente requer tratamento cirúrgico urgente e a substituição do segmento aórtico continua o gold standard. No entanto, é um procedimento muito agressivo e alguns doentes são excluídos do tratamento pelas suas comorbilidades. Atualmente, o tratamento endovascular representa uma alternativa, ainda sem indicações precisas. O nosso objetivo é apresentar um caso de tratamento híbrido de uma AD tipo A com recurso a um acesso vascular cardíaco transapical.
Material/Métodos: revisão de um caso clínico e literatura.
Resultados: Homem de 65 anos com antecedentes de doença pulmonar obstrutiva crónica, fibrilação auricular e hipertensão arterial; recorreu ao serviço de urgência por dor abdominal. Realizou angio-TAC que revelou uma AD tipo A e uma úlcera (PAU) na aorta ascendente (AA). Após a avaliação por cirurgia cardíaca, foi considerado não candidato para cirurgia convencional. A angio-TAC foi repetida após duas semanas de tratamento médico e revelou crescimento do falso aneurisma, com risco iminente de rutura. Ponderamos o tratamento endovascular e diferentes opções foram consideradas, a decisão final foi propor um tratamento híbrido. O procedimento foi iniciado com um bypass femoro-axilar direito e embolização do tronco braquiocefálico. Em seguida, uma endoprótese (Valiant®) foi libertada abaixo da artéria subclávia esquerda e dois periscópios (Viabahn®) foram progredidos das artérias axilar e carótida esquerdas e a segunda endoprótese (Valiant®) foi libertada, dentro da primeira, com cobertura da carótida e subclávia esquerdas. Após várias tentativas, não foi possível progredir a terceira endoprótese para a Aorta Ascendente por falta de suporte e instabilidade hemodinâmica e o procedimento foi interrompido. Posteriormente, a angio-TAC foi repetida e revelou dissecção da AA permeável e o falso aneurisma não tratado. Foram discutidas outras opções e foi ponderado um acesso vascular anterógrado (transapical) com o objetivo de conseguir o suporte para progredir a endoprótese. Com o apoio de um cirurgião cardíaco, o ápice cardíaco foi abordado e puncionado e um fio guia rígido foi avançado, criando um throught-and-through, do apéx cardíaco até à artéria femoral, o que permitiu o avanço da endoprótese (Valiant®) por via retrógrada e a sua libertação em rapid pacing sem intercorrências e com bom resultado final.
Discussão/Conclusões: o tratamento endovascular AD tipo A é uma alternativa em doentes de alto risco clínico e características anatómicas adequadas, ainda que tecnicamente possa ser desafiante. Quando a progressão da endoprótese por acesso vascular retrógrado não é conseguida, a abordagem cardíaca transapical é uma alternativa a ser considerada.
Palavras-chave: Acesso transapical, dissecção aórtica tipo A, tratamento endovascular
INTRODUCTION
Acute aortic type A dissection usually requires urgent surgical treatment to avoid lethal complications such as rupture, pericardial tamponade, coronary obstruction or aortic regurgitation but operative mortality remains high (15–30%) despite surgical techniques improvement(1). For untreated acute ascending aortic dissection mortality increases up to 75% whitin two weeks after the initial event(2). Although, it is a very aggressive procedure and some patients are considered too frail for this treatment because of their comorbidities(3). Endovascular repair represents an alternative treatment but still without precise indications or appropriate devices.
Transapical vascular access was first applied for transcatheter aortic valve implantation (TAVI) in the presence of severe aortoiliac disease which invalidate retrograde transfemoral access. A transapical access for aortic endografting was first described by Grenon at al in a pig model(4).
In this paper we present a case of hybrid treatment of a type A aortic dissection with resource a transapical cardiac access.
CASE REPORT
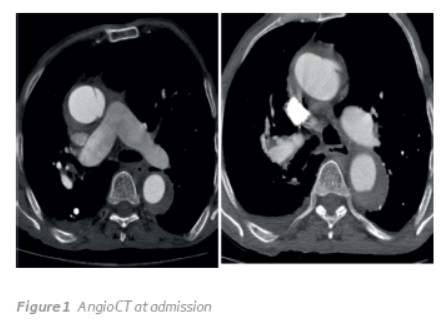
A 65-year-old man with history of chronic pulmonary obstructive disease, pulmonary emphysema, atrial fibrillation and hypertension came to the emergency department with abdominal pain. He underwent angio-CT that revealed type A aortic dissection with a false aneurysm in the ascending aorta (Figure 1) and a visceral false aneurysm (esplenic artery branch) with retroperitoneal haematoma.
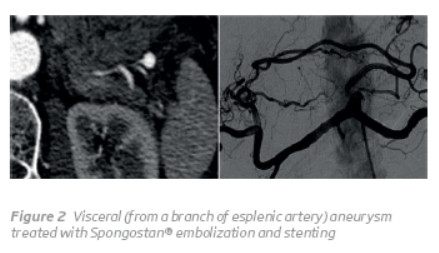
The emergente lesion to treat was the visceral false aneurysm bleeding (Figure 2) so the patient was taken to the angiography room and the source of the visceral bleeding was identified and treated with Spongostan® embolization and covered stenting with resolution of the hemorrhagy.
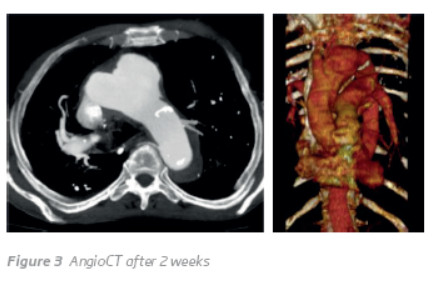
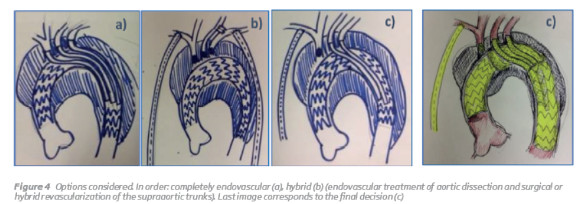
After evaluation by cardiac surgery, he was considered too frail for conventional surgery. The patient was admited in the intensive care unit to do the best medical treatment (strict blood pressure control, analgesia and clinical/analytical monitoring). Angio-CT was repeated two weeks latter and revealed false aneurysm growth, with imminent risk of rupture (Figure 3). So there was a need for treatment. As the patient had been refused for conventional surgery because of his comorbidities, endovascular treatment began to be considered. Several options had been considered (Figure 4). Initially we considered fully endovascular treatment, however our center does not have experience with endovascular treatment in type A aortic dissection. Then we considered a hybrid treatment with endovascular treatment of aortic dissection and surgical or hybrid debranching of the supra-aortic trunks. The final decision was by hybrid treatment.
The procedure was started with a right femoro-axilar bypass and embolization of the brachyocephalic trunk. Then, an endoprosthesis (Valiant®) was delivered below the left subclavian artery, two periscopes (Viabahn®) from left carotid and axillar arteries were progressed and the second endoprosthesis (Valiant®) was released into the aorta, inside the first, with coverage of the left common carotid and subclavian, and then the Viabahn® was released. After multiple attempts, it was not possible to progress the third endoprosthesis to the ascending aorta because of lack of support and the procedure was interrupted. Another CT control was done and revealed permeable ascending aorta dissection with the second endoprotheses towards the false aneurysm (Figure 5).
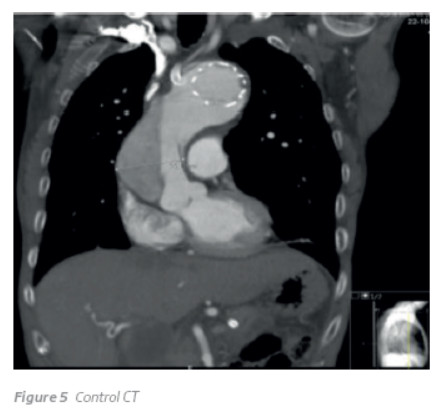
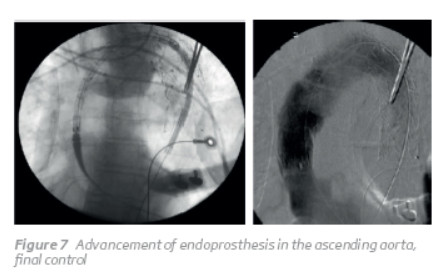
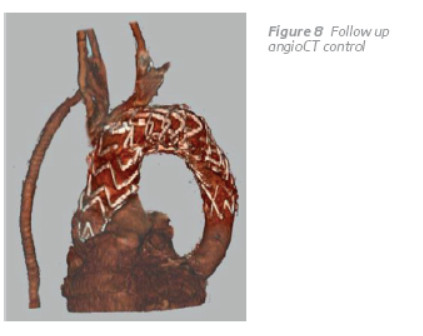
We discussed other options and an anterograde (transapical) approach was considered to progress a stiff guidewire on through-and-through between cardiac apex and femoral access and try to proggress the endoprothesis through the femoral access. With cardiac surgeon support through a mini thoracotomy we approach the apex of the left ventricle. We puncture the apex and introduce a 5Fr sheat. After that we progressed a through-and-through stiff guidewire (Lunderqvist guide-wire) and we progressed the endoprothesis through the femoral access (Figure 6). This through-and-through guide wire allowed advancement of the endoprosthesis (Valiant®) to the ascending aorta, with no intercurrences or hemodynamic instability. After performing angiography for marking coronary arteries ostial, the endoprothesis was released in the ascending aorta under rapid-pacing with good final result (Figure 7). With a follow-up of more than 1 year the patient is alive, with a small dissection in the ascending aorta, with complete thrombosis of the false aneurysm, without endoleaks and with all supra-aortic trunks revascularizations permeable (Figure 8).

DISCUSSION
Thranscatheter treatments for structural heart diseases have emerged as an alternative treatment for patients considered too frail for open surgery(5). In 2002, Cribier performed the first transcatheter aortic valve implantation (TAVI)(6) and in the subsquent decade TAVI evolved. Initially performed via a transfemoral access, transapical access was first reported in TAVI as an access resource in patients with limitative aortoiliac disease (severe calcification/turtuosity which could not acommodate the large sheats required) and was described as a safe method with short-term results comparable with transfemoral access. This transapical access was achieved via a mini-thoracotomy at the fith intercostal space and several advantages were pointed to this access(7). After that, transapical access was used as an access to perform TEVAR. A transapical access for aortic endografting was first described by Grenon at al in a pig model and at the end of the study the authors reported the treatment of a ruptured aortic arch aneurysm via transapical access. In this case, the apex of the left ventricle was accessed via a mini-thoracotomy and the endograft was deployed under rapid ventricular pacing, via a 24Fr sheat.
Type A aortic dissection requires urgent surgical treatment, however, it is a very aggressive surgery and some patients, due to their comorbidities, are excluded from treatment. Endovascular treatment has been used in some particular cases, but still without clear indications and with no suitable devices.
In the present case we could not complete the procedure via retrograde femoral access so we hypothesized to use a transapical access to progress a guide wire on through-and-through to achieve the suport we need to progress the endoprothesis via the usual retrograde access (which is less aggressive). This strategy allowed full support for endograft advancement in the ascending aorta with hemodinamic stability. The endoprothesis was released in ascending aorta under rapid ventricular pacing without complications and with good final result with no endoleak. Postoperative angioCT revealed no image of aortic dissection or false aneurysm and no endoleak. Althoug, there are some possible complications related to this access such as formation of apex pseudoaneurysm and late ventricular septal defect(8) we don't face any of it. With a follow -up of more than 1 year the patient is alive, with a small dissection in the ascending aorta, complete thrombosis of the false aneurysm, without endoleaks and with all supra-aortic trunks revascularizations permeable.
CONCLUSIONS
Endovascular or hybrid treatment is an alternative in patients of high clinical risk and adequate anatomical characteristics, yet technically challenging. When the retrograde progression of the endoprosthesis is not achieved, the transapical cardiac approach is an alternative to be considered.
REFERENCES
Trimarchi S, Nienaber CA, Rampoldi V, Myrmel T, Suzuki T, Mehta RH, et al. Contemporary results of surgery in acute type A aortic dissection: The International Registry of Acute Aortic Dissection experience. The Journal of Thoracic and Carsiovascular Surgery,2005:112–122 [ Links ]
Grabenwoger M, Weiss G. Type A aortic dissection: the extent of surgical intervention. Annals of Cardiothoracic Surgery; 2013;2(2):212–215 [ Links ]
Senay S, Alhan C, Toraman F, Karabulut H, Dagdelen S and Cagil H. Endovascular Stent-graft Treatment of Type A Dissection: Case Report and Review of Literature. Eur J Vasc Endovasc Surg.2007,34:457–460 [ Links ]
Grenon SM, MacDonald S, Sidhu RS, Reid JD, Cheung A, Hsiang Y et al. Successful ventricular transapical thoracic endovascular graft deployment in a pig model. J Vasc Surg,2008;48(5):1301–1305 [ Links ]
Enrico Ferrari. Apical access and closure devices for transapical transcatheter heart valve procedures. Swiss Med Wkly. 2016;146:w141237. [ Links ]
Cribier A. Development of transcatheter aortic valve implantation (TAVI): a 20-year odyssey. Arch Cardiovasc Dis,2012;105(3):146–152 [ Links ]
Shults C, Gunter R, Thourani V. The versatility of transapical access: Will it lead to a completely new approach to valvular therapy? Ann Cardiothorac Surg.2012;1(2):220–223 [ Links ]
Ramponi F, Stephen MS, Wilson MK, Valley MP. Think differently: trans-apical platform for TEVAR. Ann Cardiothorac Surg,2012:1(3):412–416 [ Links ]
Correio eletrónico: ines.antunes89@gmail.com (I. Antunes).
Recebido a 14-06-2017;
Aceite a 25-10-2017;














