Introduction
Postpartum complications such as concealed hemorrhage are uncommon but potentially life-threatening. Among those, retroperitoneal hematomas are extremely rare. Their incidence is unknown since the experience in obstetrics is available almost solely from case reports1. They’re characterized by acute or subacute bleeding from the abdominal tissues into the retroperitoneum2,3. Women typically present with hypovolemic shock out of proportion to their estimated external blood loss, but in most cases the lack of specific signs and symptoms complicates its diagnosis. We present the case of a massive spontaneous onset retroperitoneal hematoma that developed one week following an uncomplicated and non-traumatic vaginal delivery.
Case report
A 27-year-old multipara (gravida 4, para 4) presented to the emergency department accusing severe lumbar and right-lower-quadrant abdominal pain, chills, and vomiting 7 days after an uncomplicated vaginal delivery. No obstetrical maneuver was used to assist the delivery. The patient had no relevant medical or surgical history, her medical record denied any occurrences during pregnancy and her labor was reported as uncomplicated. The symptoms had a sub-acute onset, starting at day 2 postpartum. Two days before, she was treated empirically with oral Amoxicillin-Clavulanic Acid for a suspected UTI, but there was no clinical improvement.
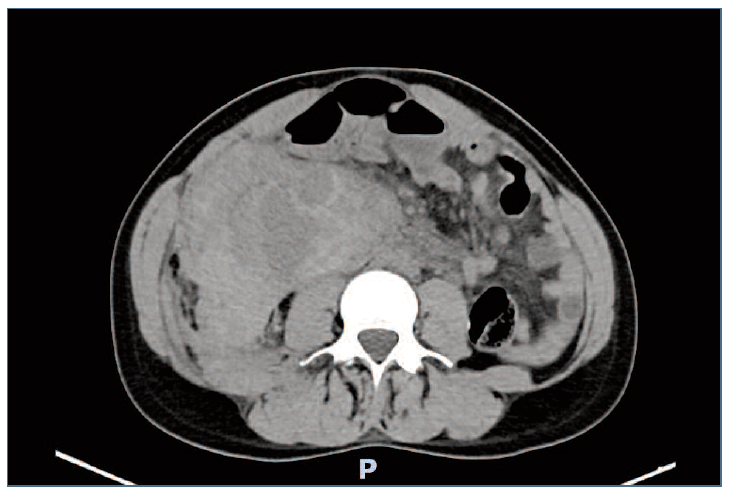
Upon presentation the woman was pale and hypotensive (72/37 mmHg). There was lower-abdominal tenderness at palpation and renal Murphy sign was positive on the right side. On pelvic examination, we found no signs of vulvar or vaginal hematoma, the cervix was atraumatic, and the uterus was in the normal pelvic position without pain on mobilization. Further investigation revealed anemia (Hemoglobin 9 g/dl) and renal function impairment (Serum creatinine 1,09 mg/dl) as well as an increased C reactive protein (CRP) (5,14 mg/dl). Arterial blood gas analysis showed tissue hypoperfusion (pH 7,453, Lactate 1,25). Fluid resuscitation was started immediately, however with no substantial improvement of the blood pressure. Abdominopelvic ultrasonographic findings revealed a mixed hyperechoic formation that extended from the left iliac fossa to the left flank, leading to the suspicion of an internal bleed. This was confirmed by a CT angiography which documented active bleeding in the retro-peritoneal space [Figure 1] and a voluminous hematoma in the right para-renal space, with 30x12x9.5cm. A laparotomy was performed, and the source of the hemorrhage detected: the proximal ends of two right ovarian veins (an anatomical variation) were separated from their insertion in the inferior vena cava, causing an active bleeding in the retroperitoneal space. Hemostasis was obtained ligating both distal ends of the ovarian veins and the vena cava using Vicryl 0. During the surgery, the patient needed continuous hemodynamic support with noradrenaline and was given in total 3 units of Red Blood Cell concentrate (RBC) and 4 units of plasma. After the surgery she was immediately admitted to the ICU with an initial hemoglobin of 6 g/dl. During the first postoperative day, 2 more RBC concentrates were administered, resulting in an improvement of the hemoglobin levels up to 8 g/dl.
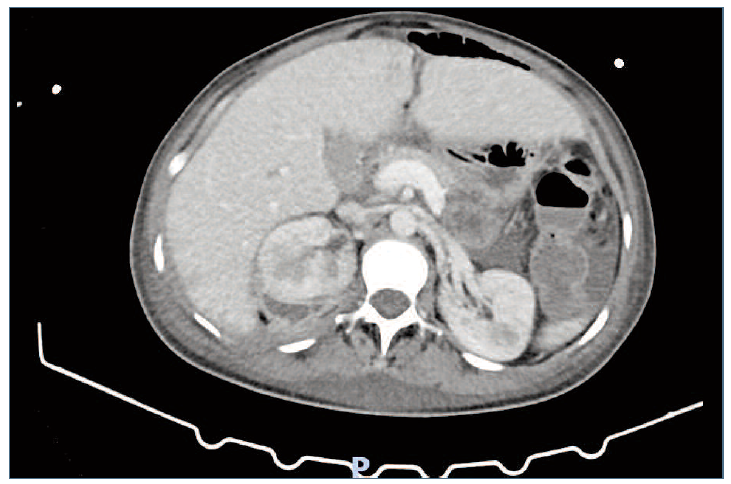
The postoperative period was complicated by infection of the remaining peri-renal hematoma [Figure 2], intestinal sub-occlusion caused by adhesions, and loculated pleural effusion. Upon the suspicion of an intra-abdominal infection, the patient underwent empiric antibiotic treatment with Piperacillin-Tazobactam (11 days) followed by Meropenem (10 days). These complications delayed the clinical improvement of our patient and led to a second laparotomy and a video-thoracoscopy, 10 and 20 days after the first surgery, respectively. The woman spent a total of 37 days hospitalized in the Surgical Intensive Care Unit, and she was discharged, fully recovered [Figure 3], only on the 38th postoperative day, 44 days after giving birth.
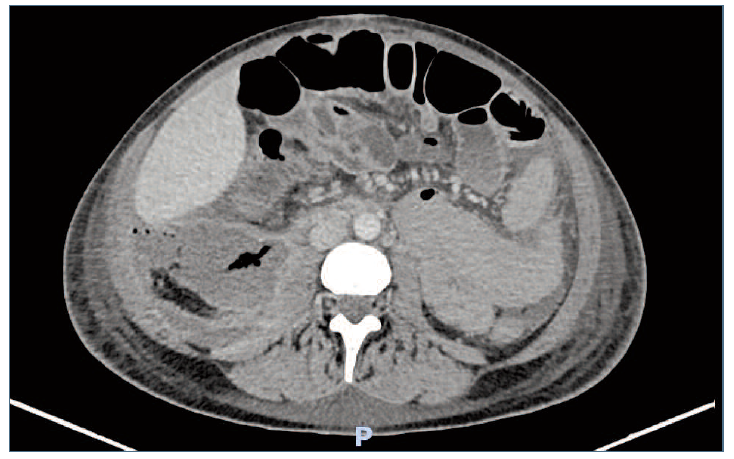
Figure 2 Abdominal CT scan showing the presence peri-renal of air bubbles peri-renal and dilation of intestinal loops confirming, respectively, infection of the remaining peri-renal hematoma and intestinal sub occlusion.
Discussion
Postpartum retroperitoneal hematomas can be a serious complication, sometimes life-threatening. Pregnancy itself is a predisposing condition: the physical stress of labor, vascular wall weakening due to hormonal changes, increased cardiac output and intravascular volume could play a role in the pathogenesis. Several other risk factors have been identified such as coagulation disorders, congenital Ehlers-Danlos syndrome type 4 with rupture of retroperitoneal vessels, prior use of anticoagulant treatment, severe preeclampsia, HELLP syndrome, multiparity, macrosomia, multiple pregnancy, prolonged active phase of labor, traumatic delivery, and manual delivery of the placenta2,3. Nevertheless, spontaneous puerperal retroperitoneal hematomas remain extremely rare in pregnancy. Our patient represents one of these cases: she did not have any of the above-mentioned risk factors, and the traction and damage of pelvic veins during the second stage of labor remains the only possible cause.
The main presenting symptom of retroperitoneal hematomas is acute or subacute onset of abdominal pain. Common signs include those related to hypovolemia: tachycardia, hypotension, and, ultimately, hypovolemic shock. Early diagnosis and management of retroperitoneal hematoma is essential to preventing serious and life-threatening consequences. However, the final diagnosis is frequently delayed due to the lack of specific signs and symptoms. Bleeding associated with retroperitoneal hematoma is frequently only internal, with no evidence of external blood loss from the vagina, as it happens for many other obstetric/gynecological complications.
The diagnostic approach of a retroperitoneal hematoma requires CT scanning to confirm its presence, determine the size and location and the source of bleeding. Ultrasound, while not as accurate as CT scan or magnetic resonance imaging (MRI), is an acceptable alternative method of diagnosing2,3,4, useful especially in the emergency unit when the CT is not available in a short time.
Because of the rarity and varied clinical presentation of such cases, the management should be individualized. Management of retroperitoneal hematomas may be conservative or surgical and will depend on the size and evolution of the hematoma, as well as the hemodynamic status of the patient3,5. A conservative approach is indicated for patients who are hemodynamically stable after fluid resuscitation, and in whom the hematoma is not expanding, and symptoms of pressure are absent6. In those cases, the expansion of the hematoma can be limited by the spontaneous self-tamponading effect that can occur in the confined retroperitoneal space2. As for the surgical approach, there is a growing trend in the use of endovascular techniques as an alternative to open surgery. The main options are selective intra-arterial embolization or stent-grafts to stop the bleeding7. However, vascular embolization requires close coordination of clinical specialists, including an interventional radiologist, gynecologist, and anesthetist, and is not feasible in many resource-limited settings. Finally, laparotomy is indicated in clinically unstable patients who have an extensive hematoma, due to the risk of a hemorrhagic shock, and our case represents one of these cases. Furthermore, a secondary infection from such hematomas is a rare but possible complication, and its management has not yet been fully elucidated8,9. What is clear is that, once an abscess develops, antibiotic treatment has a limited effect despite an in vitro high efficacy. In such cases, surgical drainage should be performed8.
Despite meeting various criteria for initiating postpartum thromboprophylaxis (multiparity, postpartum hemorrhage requiring blood transfusion, surgery during the immediate postpartum period, re-admission in hospital) (10, prophylactic anticoagulation was not administered in this patient. The authors highlight how, in this specific situation, the hemorrhagic risk was superior to the thrombotic risk, therefore representing a contraindication to thromboprophylaxis.
This case report presents an extremely rare postpartum complication, that only has a few other similar documentations. The authors present this case to warn clinicians about its possible occurrence. Despite the rarity of this (especially after a vaginal delivery) we should always maintain a high index of suspicion. Patients can develop symptoms of pelvic hematoma immediately after delivery or it may occur several days later, as in the present case. Differential diagnosis of retroperitoneal hematoma should be considered in patients with persistent abdominal pain with progressively developing anemia without any evidence of external bleeding. We presented this case to highlight also how the negative impact of these rare events is not only related to the immediate and direct consequences of the hemorrhage and hypovolemic shock, but also to the possible complications that might occur during the immediate post-operative period.
Author contributions
Noemi Curzel: Contributed to the collecting and analysis of the data, reviewing the literature, and drafting the article. Elsa Landim: Contributed to the critical review of the article and final approval of the submitted version. Teresa Costa: Contributed to the critical review of the article and final approval of the submitted version. Ana Paula Ferreira: Supervision and revision of the article, final approval of the submitted version.